Fast Psychophysical Tuning Curves and Threshold Equalizing Noise Test in Individuals with Meniere’s Disease
Srishti Rawat*, Suchi Soni and Hrudananda Sahoo
Sardar Vallabh Bhai Patel Hospital and AIISH, India
Submission: October 01, 2016; Published: October 12, 2016
*Corresponding author: Srishti Rawat, Alpha 2nd, Grater Noida, Uttar Pradesh, India, Tel: 9891497704; Email: rawat.sis@gmail.com
How to cite this article: Srishti R, Suchi S, Hrudananda S. Fast Psychophysical Tuning Curves and Threshold Equalizing Noise Test in Individuals with 009 Meniere’s Disease. Glob J Otolaryngol. 2016; 2(2): 555582. DOI: 10.19080/GJO.2016.02.555582
Abstract
Objective:The purpose of the present study was to assess Inner hair cells functioning in Meniere’s disease using fast PTCs and TEN tests. If IHC dysfunction was detected, the secondary purpose was to test the agreement between TEN test and PTC results.
Design:Ten adults (27-59 years) diagnosed as having MD participated in the study. All of them had sensorineural hearing loss of greater than 40dB at low frequencies. Duration of MD ranged between 4 months and 3 years. With their consent to participate in the study, fast PTCS and TEN (HL) test were administered in the standard testing conditions.
Result:Results showed presence of Inner hair cells dysfunction in individuals with MD. The IHC dysfunction seemed to be related to several factors such as audiometric frequency, degree of hearing loss at low frequencies, age of the individual, and duration of MD. IHC dysfunction was more likely at lower frequencies, older individuals, in greater degree of hearing loss and in those having long-standing MD. There was a good agreement between PTCs and TEN (HL) test, particularly when 20% criterion was used to interpret PTCs. PTCs detected IHC dysfunction in more number of occasions than TEN tests.
Conclusion:The findings indicate high prevalence of IHC dysfunction in individuals with Meniere’s disease, especially in long standing MD and in older individuals with hearing loss of greater than 50dB at lower frequencies. Neither PTCs nor TEN tests seem to be a gold standard test for detecting IHC dysfunction. Therefore a combination of TEN (HL) test and, PTCs with 20% criteria is recommended for the clinical testing.
Keywords:Meniere’s Disease; IHC Dysfunction; Fast PTCs; TEN testAbbreviations:TEN: Threshold Equalizing Noise; MD: Meniere’s disease; PTC: Psychophysical Tuning Curves; IHA: Inner hair cells; SWPTC: Software for Fast Psychophysical Tuning Curves; SRT: Speech Reception Threshold; SIS: Speech Identification Score; ABR: Auditory Brainstem Response; LPTA: Low frequency Pure-Tone Average
Introduction
Meniere’s disease is an idiopathic condition which leads to inner ear disorder, characterized by episodic vertigo, fluctuating hearing loss, aural fullness and tinnitus [1]. Hearing loss is one of the major symptoms, usually reported in one ear, typically at low-frequencies [2]. Endolymphatic hydrops is suggested to be the mechanism causing Meniere’s disease, with support from histological studies [3,4]. Endolymphatic hydrops refers to bulging of the cochlea at the scala media boundaries due to endolymph build up. This excess fluid accumulation inside the scala media tends to bulge basilar membrane where it is most flaccid. Excess pressure of endolymph thus becomes most evident at the apex of the cochlea, and mostly shall affect the low-frequency hair cells. This leads to ruptures of membrane resulting in mixing of inner (endolymph) and outer (perilymph) fluids which in turn damages hair cells and leads to hearing loss.
Nadol & Thornton [5] performed a morphometric analysis on hair cells, spiral ganglion cells, dendritic fibers in the osseous spiral lamina, afferent and efferent endings, and afferent synaptic contacts in an individual with documented unilateral Meniere’s disease. They found damaged outer and inner hair cells, including disruption of the cuticular bodies and basal-ward dislocation of some outer hair cells. Also, there were significantly less number of afferent nerve endings and afferent synapses at the base of hair cells in the ear with Meniere’s disease as compared to the contralateral ear. The damage of OHCs and IHCs can be psychoacoustically determined using psychophysical tuning curves (PTC) and threshold equalizing noise (TEN) test. PTCs show broader tuning curve for OHC damage and shift in the peak frequency indicates off frequency listening due to IHC damage.
Although clinically very useful, the traditional method for determining PTCs was a lengthy and time consuming procedure [6]. This lead to advent of fast PTCs. Sęk, et al. [7] introduced a fast method for determining PTCs, using a band of noise that sweeps in centre frequency and a Bekesy method to adjust the masker level required for threshold. They reported that the PTCs shapes were similar for the fast and traditional methods, for both normally hearing and hearing-impaired individuals. TEN (HL) test, on the other hand, is an established test for assessing IHC dysfunction and takes lesser time than conventional PTCs. However, precise identification of edge frequency is not possible due to the large mid octave steps utilized in the TEN (HL) test.
Studies have shown that there is a reduction in the number of afferent nerve endings and afferent synapses at the base of both inner hair cells (IHCs) and outer hair cells in the ears with Meniere’s disease [5]. Consequently, predominant low frequency hearing loss has been reported in these individuals. However, there is a dearth of documentation of IHC functioning in Meniere’s disease. The low frequency hearing loss seen in individuals with Meniere’s disease may involve IHC dysfunction. Fluctuating nature is a trademark of Meniere’s disease. The understanding of IHC functioning in the individuals would help us infer about reversibility of hearing loss and thus, guide in counseling the clients. Further, the understanding may also be useful in hearing aid gain prescription, thus aiding rehabilitation process. Hence, the present study was taken up.
Methods
TEN test and Fast PTCs were carried out in individuals with MD and results of these tests were analyzed to find the presence or absence of Inner hair cells (IHC) dysfunction.
Participants
The study involved 9 adults (3 females and 6 males) in the age range of 27 to 59 years. All of them had sensorineural hearing loss consequent to their onset of MD diagnosed by qualified ENT surgeon. The pure tone thresholds were at least 40dB at lower frequencies (250, 500, & 1000 Hz) in the affected ear. The symptoms of MD persisted for a minimum of 4-5 months and maximum of 3 years among the 9 participants. There was no indication of middle ear pathology according to immittance findings. Auditory brainstem response and Otoacoustic emissions ruled out the presence of retrocochlear pathology. All participants were categorized as per the AAO-HNS criteria as “definite” MD.
Instrumentation
A calibrated two channel Maico MA53 audiometer, a personal computer and a Grason- Stadler Incorporated Tympstar (version 2) tympanometer were the equipments used in the study. TEN (HL) and Software for fast psychophysical tuning curves (SWPTC) were used through the computer for administration of TEN test and PTCs. All instruments were calibrated according to ANSI standards. All the tests were carried out in acoustically treated audiometric room where the ambient noise levels were within the permissible limits as per calibrated according to ANSI S3.1 [8].
Test procedure
Preliminary evaluation was carried out to ensure that the participants fulfilled all the inclusionary criteria. A detailed case history was taken from each participant and presence of triad of MD (hearing loss, tinnitus & vertigo) along with nature and duration of the problem was noted. The individuals who fulfilled the AAO-HNS criteria for “definite” MD, i.e., suffered two or more impulsive episodes of vertigo that lasted for at least 20 minutes, had sensorineural hearing loss, and tinnitus or aural fullness during episodes of vertigo in the affected ear were included. Further, all participants were diagnosed as MD by the ENT surgeon. A written consent was taken from all the participants included in this study.
Pure tone audiograms were obtained using modified Hughson-Westlake method [9]. Air conduction thresholds were estimated for 250-8000Hz audiometric frequencies and bone conduction thresholds were estimated between 250 Hz to 4000 Hz. Speech audiometry was administered to measure speech reception threshold (SRT), speech identification score (SIS) and uncomfortable level. Tympanometry was done to rule out middle ear pathology using 226 Hz probe tone. Acoustic reflex thresholds were measured for 500, 1000, 2000 and 4000 Hz. Oto-acoustic emissions and Auditory Brainstem Response (ABR) were used to rule out retrocochlear pathology.
Experimental Evaluation
A. Administration of TEN (HL) Test
Unmasked pure tone thresholds were measured for signals from 500 to 4000Hz in 2dB steps with MAICO MA53 audiometer. Patients were instructed to ignore the noise and raise their finger on hearing the tone. Audiometer was then connected to a computer and two tracks from TEN (HL) CD containing the pure tones and the threshold equalizing noise (TEN) were fed to audiometer, where the tracks were mixed and presented to the same ear. Test frequencies were 0.5, 0.75, 1, 1.5, 2, 3, and 4 kHz. The TEN (HL) level is specified as the level of a one-ERBN wide band centered at 1 kHz, where ERBN stands for the equivalent rectangular bandwidth of the auditory filter determined by using young normally hearing subjects at moderate sound levels [10].
A TEN level of 70dB HL/ERBN was used [11]. However, a lower level was used for one participant who was unable to tolerate the loudness of the TEN. The level of the signal and the TEN were controlled using the attenuators in the audiometer. The signal level was varied in 2dB steps to determine the thresholds [6]. A ‘no response’ was recorded when the subject did not indicate hearing the signal at the maximum output level of the audiometer.
B. Fast PTCs
Fast PTC software, SWPTC, installed in computer was used for measuring psychophysical tuning curves (PTCs) using a narrowband noise masker that sweeps in frequency. The software was calibrated before starting the test to ensure the correct level of signal being transmitted by the computer. The sensitivity of the Senheisser headphones used, i.e., 108.5dB SPL for 0.5 RMS according to manufacturer’s specifications, was entered and instrument was calibrated automatically by the software. The software generates a full-scale sine-wave on both channels of the sound card and the RMS voltage was measured manually at the input to the headphones. This voltage was found to be 0.28 VRMS which was entered to get the maximum levels of sine wave and noise band. Maximum levels of sine wave and noise band were found to be 103dB SPL and 91dB SPL respectively
SWPTC software was installed on a PC with a standard sound card. The signals were played out from the PC and presented using Sennheisser HDA200 headphones. The masker was a narrowband noise that continuously swept in frequency. The probe signal was a pulsed pure tone signal fixed in frequency and presented at an intensity of 10dB above the absolute threshold at the probe frequency. Probe frequencies of 250 to 4000 Hz in mid-octave steps were used. The center frequencies of the noise ranged from one octave below the probe frequency to one octave above the probe frequency. Ear to be tested was selected in the software and participant’s task was to detect a sinusoidal signal, which pulsed on and off, in the presence of masker whose centre frequency slowly changed, from low to high (Forward sweep). The intensity of the masker was increased at a rate 2dB/s as long as the signal remained audible, after which, intensity was decreased at the rate of 2dB/s. In this way, the software tracked masker level required just to mask the signal using a Bekesy tracking method. The frequency tip of Psychophysical tuning curves was derived from the output curve.
Response analysis
- TEN test: Pure tone thresholds without TEN were compared with that of the masked thresholds. The criteria for presence or absence of IHC dysfunctions were as follows [6].
- If the masked threshold is 10dB or more above the TEN levels, and the TEN elevated the absolute threshold by 10dB or more, then an IHC dysfunction was considered to be present.
- If the masked threshold in presence of TEN is less than 10dB above the TEN levels and the masked threshold is greater than the unmasked threshold 10dB or more, then no IHC dysfunction.
- Fast PTCs: In this study both 10% and 20% PTC shift criteria were taken to detect IHC dysfunction, i.e., a shift in tip of PTC more than 10% and 20% respectively, of test frequency will be considered as IHC dysfunction.
Results
A total of 10 ears of 9 participants with Meniere’s disease were assessed using Threshold equalizing noise (TEN) test and fast psychophysical tuning curves (PTC) and following results were obtained:
Individual Demographic Data and Basic Audiological Details of Participants
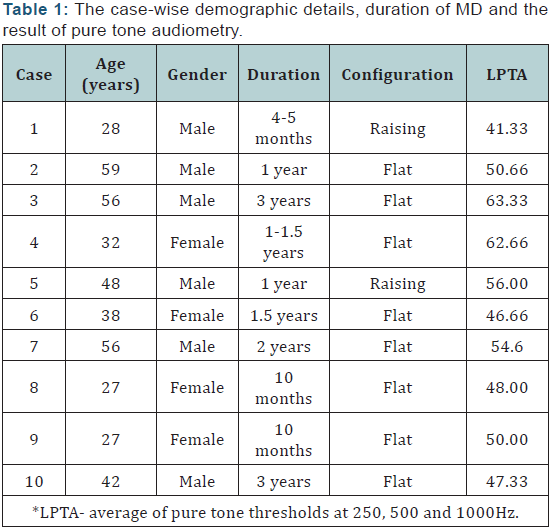
Low frequency pure-tone average (LPTA) was derived for all the participants on the basis of three-frequency average (0.25, 5, and 1 kHz) [12]. Data of each patient are as follows. (Table 1) gives the case-wise demographic details, duration of MD and the result of pure tone audiometry. All subjects were in age range of 27 to 59 years with mean age of 41 years. The duration of MD ranged from 4 months to 3years. Low frequency pure tone average (250, 500 and 1000 Hz) revealed hearing loss above 40dB with most of the participants (8/10) having flat hearing loss. Criterion recommended by Moore, Huss, Vickers, Glasberg, and Alcantara [13] was used to classify TEN test results as normal or abnormal. Fast PTCs tips were generated using MATLAB. Results of Fast PTCs were compared with both 10% and 20% [14] shift of PTC tip criteria.
Prevalence of inner hair cell dysfunction
Prevalence, in this context, refers to proportion of the group found to have inner hair cell dysfunction. Out of ten subjects, three were found to have no inner hair cell dysfunction at any frequency in any of the tests. In rest of the seven participants, there was an indication of inner hair cell dysfunction on PTCs using 10% shift criterion at one or more frequencies. The number of participants with inner hair cell dysfunction decreased to five when 20% shift criterion was used. On the other hand, in TEN tests, only three participants showed inner hair cell dysfunction at one or more frequencies, while in others IHC functioning was found to be normal.
Prevalence of inner hair cell dysfunction as a function of hearing threshold at the test frequency
Most participants having inner hair cell dysfunction had their audiometric thresholds above 50dB HL at the test frequency. No IHC dysfunction was found at any audiometric frequency when the hearing loss was 40dB or less, except in Case 1 on fast PTCs using 10% criterion indicated presence of IHC dysfunction. All the participants with LPTA of more than 60dB were found to have inner hair cell dysfunction at least at one test frequency. The dysfunction was more likely at lower frequencies than
Relationship between inner hair cell dysfunction and age
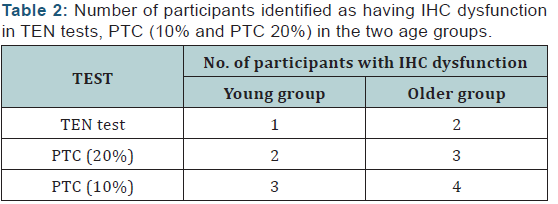
To see the effect of age, participants had to be divided into two groups of equal number. For this, a scatter plot of the age was derived and a cut off age that divides the group into two with equal number in both was found. This cut off age was 40 years. First group constituted of younger participants, aging 20 to 40 years and the second group included older participants aging above 40 years. (Table 2) gives the number of participants in the younger and older group, detected as having IHC dysfunction according to TEN test and PTCs. From the table it can be noted that number of individuals detected as having IHC dysfunction were more in older group compared to younger group.
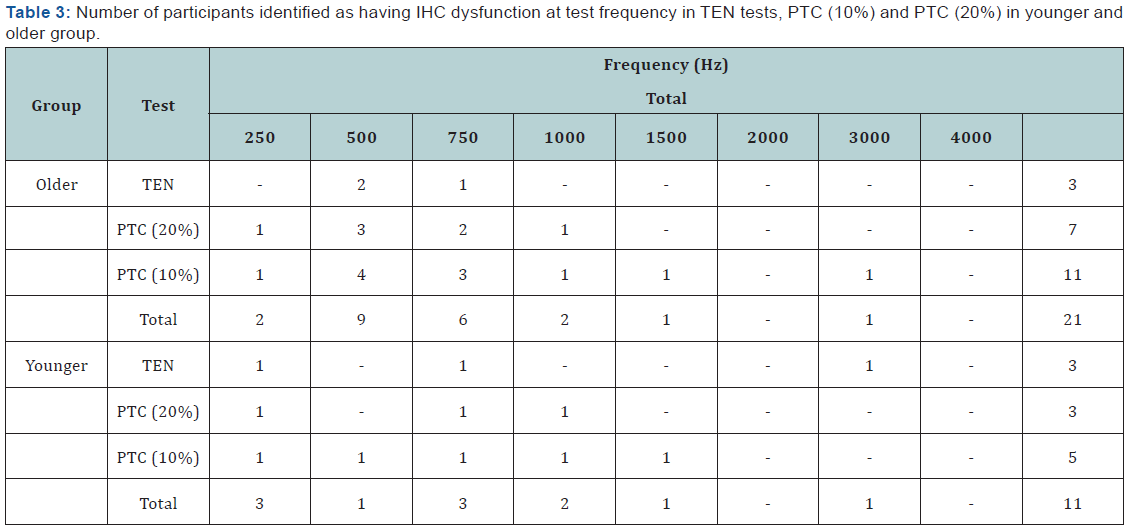
Frequency-wise analysis of IHC dysfunction, in each group was also carried out. (Table 3) gives the number of frequencies in each group according to TEN tests, and PTCs detected as having IHC dysfunction. Results for individual frequencies indicated that prevalence of inner hair cell dysfunction was more in older group in all the three tests and more number of participants had inner hair cell dysfunction at low frequencies (250, 500 and 750 Hz) than higher frequencies.
Relationship between inner hair cell dysfunction and duration of MD
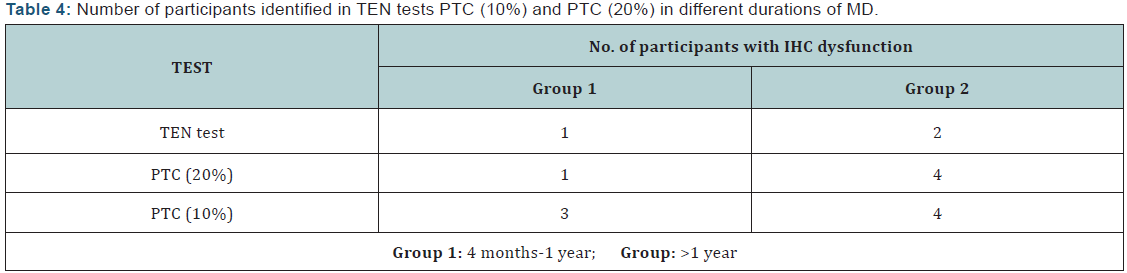
To verify the relationship between IHC dysfunction and duration of MD, the participants were divided into two groups on the basis of duration of MD, such that both groups had equal number of participants. A method similar to that used in age groups was used to derive the cut-off duration of 1 year. Group 1 had 5 participants with duration of MD from 6 months to 1 year while 5 participants from group 2 had MD for more than 1 year. (Table 4) gives the number of participants detected as having IHC dysfunction in two groups divided based on age of onset. It can be seen from the table that total number of participants in group 2 having IHC dysfunction was more than group1. This was true for both TEN test and PTC (10 and 20%).
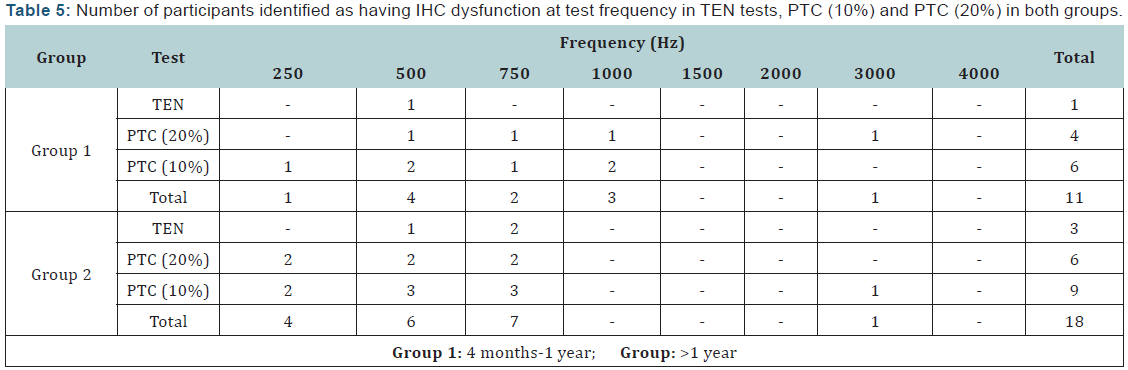
Frequency-wise analysis of IHC dysfunction, in each group was carried out. (Table 5) gives the number of frequencies in each group according to TEN test, and PTCs. Results for individual frequencies indicated that prevalence of inner hair cell dysfunction was more in group 2 in all the three tests and more number of participants had inner hair cell dysfunction at low frequencies (250, 500 and 750 Hz) than higher frequencies.
Correlation between results of TEN test and PTCs
First symbol depicts result of PTCs and second symbol stands for TEN test result. “+” and “-” signs depict presence and absence of inner hair cell dysfunction respectively.
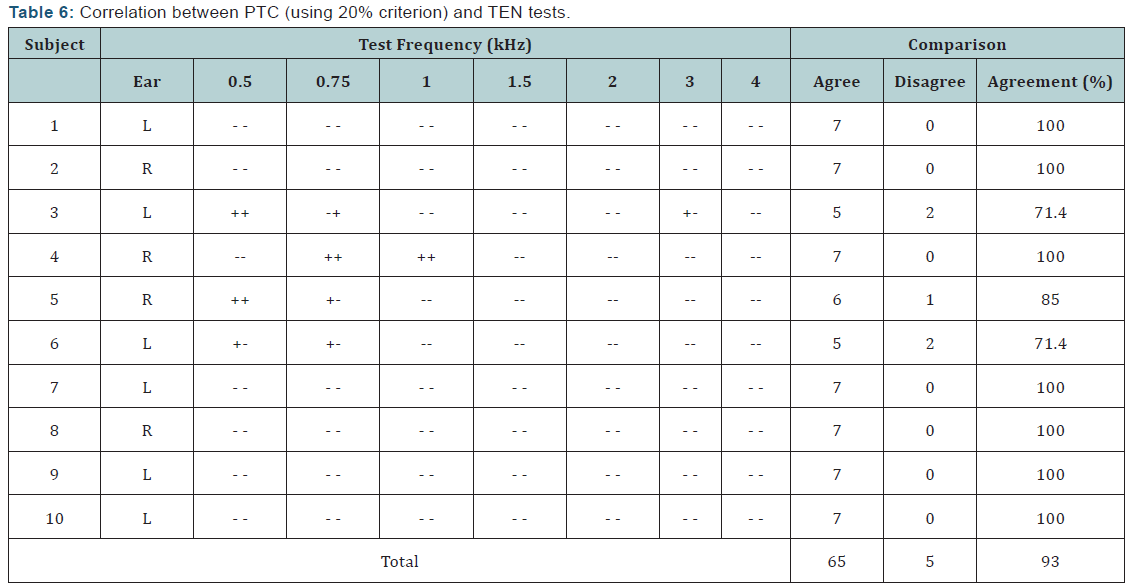
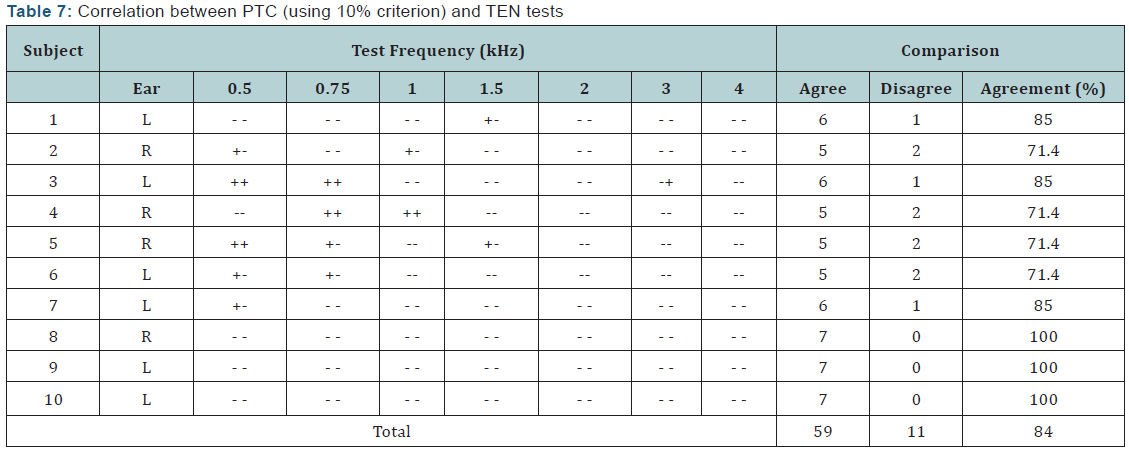
The agreement between PTC and the TEN test results was evaluated separately using 10% and 20% criteria. (Tables 6 & 7) depicts the agreement of TEN test and PTCs with 20% and with 10% criteria respectively. The agreement between TEN test and PTCs based on the presence or absence of inner hair cell dysfunction across tested frequencies was found to be 93% using 20% tip-shift criterion for PTCs.
Using 20% criterion, PTC and TEN test diagnoses were in 100% agreement in seven years (Case 1, 2, 4,7-10). In rest of the three ears, for one ear (case 6), agreement was found to be 71.4% while for two years (case 3 and 5) it was found to be 85%. On the other hand, the agreement between PTC and the TEN test results based on the presence or absence of inner hair cell dysfunction across tested frequencies was found to be 84% using 10% tip-shift criterion.
With this criterion, PTC and TEN test diagnoses were in 100% agreement in 3 years (Case 8-10). In rest of the seven ears, four ears (case 2, 4-6) showed agreement to be 71.4% while for the other three participants (case 1,3 and 7), it was found to be 85%. Therefore, degree of correspondence between TEN test and PTCs using 20% tip-shift criterion is found to be better than correspondence between TEN test and PTCs using 10% tip-shift criterion.
Discussion
The participants of this study had typical features of MD in terms of demographic, otological and audiological results. Watanabe [15] reported age of onset of MD to be 41 to 42 years.
Similar to his report, although only of 10 individuals, the mean age in the present study was 41.3 years. All the participants had two or more impulsive episodes of vertigo that lasted for at least 20 minutes in duration as well as sensorineural hearing loss, and tinnitus along with aural fullness during episodes of vertigo in the affected ear. Therefore, all participants fell in range of “definite” MD according to AAO-HNS criteria [16]. Most of the participants exhibited sensorineural hearing loss of flat or rising configuration which again is typical of MD.
Configuration of hearing loss was flat in most participants, while in some cases it was rising. Enander and Stahle [17] found that hearing loss in initial stages of MD is affecting only in the low frequencies, leading to rising configuration of audiograms, while in later stages it becomes flat. Therefore, one can infer that most cases in the present study belonged to advanced stage of MD as they had flat hearing loss configurations. One possible explanation for the flat hearing loss is that, in endolymphatic hydrops which is suggested to be the mechanism underlying MD, [3,4] there is a heavy accumulation of the endolymph. This excess build-up of endolymph inside the scala media tends to distend the membrane where it is most flaccid.
Excess pressure of endolymph thus becomes most evident at the apex of the cochlea which is most flaccid, and hence, affects the low-frequency hair cells. As the disease advances, endolymphatic pressure increases, which in turn, causes a rupture in the Reissner membrane leading to mixing of perilymph and endolymph that causes mechanical disturbance in organ of corti and damage to inner and outer hair cells. Hearing loss, at this stage becomes flat and irreversible [18]. Average degree of hearing loss in all the participants was more than 40dB at low frequencies (250, 500 & 1000 Hz). This was one of the important inclusionary criteria as in earlier studies, it was reported that sensorineural hearing loss of 40 to 50dB at low frequencies is often associated with low-frequency IHC dysfunction [19,20]. Since, aim of the present study was to investigate the possibility of IHC dysfunction in MD, a minimum criterion of low frequency pure tone average of 40dB was used.
IHC functioning in MD
Tools available to assess IHC dysfunction include TEN test and PTCs. Although clinically very useful, the traditional method for determining PTCs was a lengthy and time consuming procedure. This demerit led to the advent of fast PTCs, which along with TEN was utilized to detect presence of IHC dysfunction in this study. The results indicated presence of IHC dysfunction in most participants. These results show experimental evidence for the assumption made by Halpin, Hasso and Thornton [18]. Halpin assumed that IHC dysfunction may be present in MD at advanced stages, when the hearing loss becomes irreversible. This might be due to rupture of the Reissner membrane leading to permanent damage to OHCs and IHCs. Criterion recommended by Moore, Glasberg and Stone [13] was used to classify TEN test results as normal or abnormal, i.e., if the masked threshold is 10dB or more above the TEN levels, and the TEN elevated the absolute threshold by 10dB or more, then an IHC dysfunction was considered to be present.
Results of TEN test were compared with both 10% and 20% shift of PTC tip criteria
Moore, et al. [13] stated that a shift of PTC tip by more than 10% of the probe frequency is indicative of IHC dysfunction while Warnaar & Dreschler [14] found a higher agreement between fast PTCs and TEN tests when a PTC shift of 20% was considered. Further, even in normal hearing individuals PTC shift is found to be as high as 20% [21]. Therefore, in the present study correlation was assessed using both criteria.
IHC dysfunction is found to be correlated with degree of hearing loss. Most participants having IHC dysfunction had their audiometric thresholds above 50dB HL at the test frequency. These results are in agreement with previous studies in suggesting that, for a large number of listeners with moderate to severe hearing loss, cochlear damage may involve IHC dysfunction [20,22]. There was no evidence of IHC dysfunction at any audiometric frequency where hearing loss was 40dB or less, except in Case 1 where fast PTCs using 10% criterion indicated presence of IHC dysfunction. This probably is because of the reason that even in individuals with normal IHC functions; PTC tips can vary within 20% of the test frequency [21]. In such cases, using 10% criterion may cause false alarm.
Degree of correspondence between TEN test and PTCs using 20% tip-shift criterion was found to be better than correspondence between TEN test and PTCs using 10% tip-shift criterion. These results were consistent with the data obtained by Warnaar & Dreschler [14] that compared 10% and 20% criteria of PTC shift in sensorineural hearing loss cases with TEN test results and recommended use of 20% criterion as there was a better correlation with TEN test results.
Subject related factors affecting IHC functioning in MD
Subject- related factors that were found to affect IHC functioning were age and duration of MD. Total number of participants in older age group having IHC dysfunction was more than younger age group for both TEN test and PTCs. These results were consistent with study by Vinay and Moore [11] where they indicated a higher prevalence of dead regions in adults with sensorineural hearing loss above the age of 50 years. Therefore, age can be considered as a precipitating factor for IHC dysfunction.
The prevalence of IHC dysfunction in participants with longer duration of MD was more compared to those with lesser duration of MD. This might be attributed to the reason that patients with MD since longer time had higher degree of hearing loss as compared to other group. Further, it was seen that most of the participants, with longer duration of MD, who showed IHC dysfunction, were from older age group. In contradiction to the above, participant-10, who had MD since 3 years (maximum duration of MD in the study), did not show any evidence of IHC dysfunction. On the other hand, participant-3 who also had Menieres’s disease for 3 years had IHC dysfunction at three frequencies. This difference can be attributed the fact that the age of onset of MD in participant-10 was 39 years and in participant 3 was 56 years.
Thus, it is plausible to infer that duration of MD affects the cochlear function differently depending on the age of onset. Two possible explanations can be considered in this regard.
- There could have been a pre-existing hearing loss due to aging which might have been exacerbated by the MD,
- The cochleae in older individuals are generally more vulnerable to damage. All the participants in the study reported of hearing difficulties only after the onset of MD. This supports the second explanation suggesting the vulnerability of the aged cochlea to damage in the absence of any pre-existing hearing loss. Therefore, age may be considered an important pre-disposing factor for IHC dysfunction. The duration of MD further precipitates IHC dysfunction depending on the age of onset.
- Sajjadi H, Paparella MM (2008) Meniere disease. Lancet 372(9636): 406-414.
- Ophiem, Flottrop G (1955) Joint meeting at Northwegian societies of otology and Neurology.
- CS Hallpike, H Cairns (1938) Observations on the Pathology of Ménière’s Syndrome. The Journal of Laryngology & Otology 53(10): 625-655.
- Horner KC (1991) Old theme and new reflections: Hearing impairment associated with endolymphatic hydrops. Hear Res 52(1): 147-156.
- Nadol JB, Thornton AR (1987) Ultrastructural findings in a case of Menière’s disease. Ann Otol Rhinol Laryngol 96(4): 449-454.
- Moore BC, Glasberg BR, Stone MA (2004) New version of the TEN test with calibrations in dB HL. Ear Hear 25(5): 478-487.
- Sek A, Alcántara J, Moore BC, Kluk K, Wicher A (2005) Development of a fast method for determining psychophysical tuning curves. Int J Audiol 44(7): 408-420.
- American National Standard Institute (1991) Maximum permissible ambient noise for audiometric test rooms. American Journal of Audiology 9(1): 3-8 New York.
- Raymond Carhart, James F Jerger (1959) Preferred method for clinical determination of pure-tone thresholds. JSHD 24: 330-345.
- Moore BC, Glasberg BR, Stone MA (2004) New version of the TEN test with calibrations in dB HL. Ear Hear 25(5): 478-487.
- Vinay, Moore BC (2007) Prevalence of Dead Regions in Subjects with Sensorineural Hearing Loss. Ear Hear 28(2): 231-241.
- Battista RA (2004) Audiometric Findings of Patients with Migraine- Associated Dizziness. Otol Neurotol 25(6): 987-992.
- Moore BC, Huss M, Vickers DA, Glasberg BR, Alcántara JI (2000) A test for the diagnosis of dead regions in the cochlea. Br J Audiol 34(4): 205- 224.
- Warnaar B, Dreschler WA (2012) Agreement between psychophysical tuning curves and the threshold equalizing noise test in dead region identification. Int J Audiol 51(6): 456-464.
- Watanabe I (1985) Incidence of Meniere’s disease including some other epidemiological data. In: Meniere’s disease: A comprehensive Appraisal. Edited by WJ Oosterveld (Wiley).
- Committee on Hearing and Equilibrium (1995) Meniere’s disease: Criteria for diagnosis and evaluation of therapy for reporting. AAOHNS Bulletin 5: 6-7.
- Enander A, Stahle J (1967) Hearing in Meniere’s disease. Acta Oto- Laryngologica 64(1-6): 543-556.
- Halpin C, Thornton A, Hasso M (1994) Low-frequency sensorineural loss: Clinical evaluation and implications for hearing aid fitting. Ear Hear 15(1): 71-81.
- Thornton AR, Abbas PJ, Abbas PJ (1980) Low-frequency hearing loss: Perception of filtered speech, psychophysical tuning curves, and masking. J Acoust Soc Am 67(2): 638-643.
- Vickers DA, Moore BC, Baer T (2001) Effects of low pass filtering on the intelligibility of speech in quiet for people with and without dead regions at high frequencies. J Acoust Soc Am 110(2): 1164-1175.
- Carney AE, Nelson DA (1982) An analysis of psychophysical tuning curves in normal and pathological ears. J Acoust Soc Am 73(1): 268- 278.
- Summers V, Molis MR, Müsch H, Walden BE, Surr RK, et al. (2003) Identifying Dead Regions in the Cochlea: Psychophysical Tuning Curves and Tone Detection in Threshold-Equalizing Noise. Ear Hear 24(2): 133-142.
- Kluk K, Moore BC (2005) Factors affecting psychophysical tuning curves for hearing-impaired subjects with high-frequency dead regions. Hear Res 200(1-2): 115-131.
- Shannon RV, Zeng FG, Wygonski J (1998) Speech recognition with altered spectral distribution of envelope cues. J Acoust Soc Am 104(4): 2467-2476.
- Baer T, Moore BC, Kluk K (2002) Effects of low pass filtering on the intelligibility of speech in noise for people with and without dead regions at high frequencies. J Acoust Soc Am 112(3): 1133-1144.
- David A DeBonis, Constance L Donohue (2008) (Eds.), Survey of Audiology: Fundamentals for Audiologists and Health Professionals (2nd edn), Illinois Academy of Audiology, Otovestibular Resources, Chicago, USA, pp: 219.
- Flottorp G (1980) Cochlear non linearity in Meniere’s syndrome. Hear Res 2(3-4): 407-409.
- David Johnson‐Davies, Roy D Patterson (1979) Psychophysical tuning curves: Restricting the listening band to the signal region. J Acoust Soc Am 65: 675-770.
- O’Loughlin BJ, Moore BC (1981) Off-frequency listening: Effects on psychoacoustical tuning curves obtained in simultaneous and forward masking. J Acoust Soc Am 69(4): 1119-1125.
- Thornton AR, Farrell G (1991) Apparent travelling wave velocity changes in cases of endolymphatic hydrops. Scand Audiol 20(1): 13- 18.
Comparison between TEN test and PTC
Differences in results of TEN test and PTCs in some patients indicate that either of the two tests is only partially reliable in detecting IHC dysfunction. Studies in literature report that the TEN (HL) test may fail to diagnose a dead region when the frequency of the test tone falls only a little inside a dead region [13,20,23]. Vinay and Moore [11] recommended applying TEN test only when the audiometric threshold exceeds 60dB HL at one or more frequencies. Furthermore, TEN test measurements may be affected by high presentation levels, producing noise-like perception of pure tones, and is not transparent for OHC activity that may influence results [14]. Therefore, PTC results are more reliable when there are unresolved disagreements.
PTCs also are affected by various factors like, beats, criterion used for interpretation etc [23]. It has been found that even in individuals with normal IHC functioning, the PTC tips may vary within 20% [21] or 10% [7] of the test frequency. Therefore, it is better to use a stringent criterion of 20% tip shift. Due to the above cited reasons, neither PTC nor the TEN tests can be considered as the ‘gold standard’ for identification of IHC dysfunction. Thus, the use of both would yield more meaningful conclusions about IHC functioning. Summers et al. [22] found a 56% correlation between PTCs and TEN test using 10% PTC tip shifts and 10dB TEN criterions. They suggested that TEN test is not a reliable tool for identifying IHC dysfunction as it is affected by many other factors like processing efficiency deficits and also deficits in central auditory processing unrelated to IHC functioning.
Contrary to the above, [14] showed a good agreement of 80% between PTCs and TEN for a 20% PTC tip shift and 10dB TEN criterion, and 67% with a 10% PTC tip shift and 10dB TEN criterion. The results of the current study showed 13% (20% PTC tip shift - 10dB TEN criterions) and 17% (10% PTC tip shift - 10dB TEN criterions) higher agreements between PTCs and TEN tests compared to the results of Warnaar and Dreschler [14]. Hence, the criteria of 20% PTC tip shift and 10dB TEN criterions are suggested in identifying IHC dysfunction.
Vinay & Moore [11] found that individuals with Auditory Neuropathy showed abnormalities on the TEN tests and not in PTCs. They suggested that the PTCs primarily reflect cochlear functioning, whereas, TEN results are also affected by retrocochlear lesions. TEN and PTCs reflect different levels of processing of the sound and when used together, provide a better insight into the cochlear and the IHC functioning in particular. Three of the participants in the current study indicated IHC dysfunction at 250 Hz on the PTCs. But they were missed on the TEN tests as the TEN tests do not include the 250 Hz frequency. Thus, the use of the two tests in combination would give more reliable and meaningful information about the IHC functioning over a broad range of frequencies. The use of PTCs, especially in the low frequencies are important in studying IHC functioning in conditions like MD, where the low frequencies are relatively more affected.
IHC functioning in MD and amplification strategies
Moore & Kluk [23] and, Vinay & Moore [11] showed that patients with IHC dysfunction at low frequencies extracted little or no information from low-frequency components in the speech. Further, it was suggested for patients with lowfrequency hearing loss that, amplification of the low frequencies via a hearing aid be provided only when there was no IHC dysfunction at low frequencies as in presence of a low frequency IHC dysfunction, even after adequate amplification of lowfrequencies, limited benefit is reported in literature. In addition, components of speech are detected and analyzed via higher frequency channels leading to distortion of high frequencies and cause difficulty in understanding the information obtained from the low frequencies [24]. Therefore, amplification should be provided in cases of low frequency IHC dysfunction, as in Meniere’s disease, with high caution.
It is stated in literature that MD may cause IHC damage at advanced stages, which is due to Reissner membrane rupture and mixing of endolymph and perilymph leading to destruction of sensory elements [11]. The current study provides evidence for the assumption in the above mentioned studies. The presence of IHC dysfunction in our study was strongly associated with late age of onset, duration of MD and greater degrees of hearing loss. This suggests that IHC dysfunction is seen in advanced stages of MD in contrast to earlier stages. The presence of IHC dysfunction in advanced stages of MD reflects the severity of damage to the cochlear structures. Thus, it is reasonable to assume that the hearing loss associated with IHC dysfunction is possibly irreversible; however, this needs experimental validation. More evidence in this regard will guide us in the rehabilitation and counseling of individuals with MD [25-30].
Conclusion
Inner hair cells dysfunction was found to be present in individuals with MD and seemed to be related to several factors such as audiometric frequency, degree of hearing loss at low frequencies, age of the individual, and duration of MD. IHC dysfunction was more likely at lower frequencies, older individuals, in greater degree of hearing loss and in those having long-standing MD. A good agreement was found between PTCs and TEN (HL) test, particularly when 20% criterion was used to interpret PTCs. PTCs detected IHC dysfunction in more number of occasions than TEN tests. However, either PTCs or TEN tests seem to be a gold standard test for detecting IHC dysfunction. Therefore a combination of TEN (HL) test and, PTCs with 20% criteria is recommended for the clinical testing.
The findings of the present study have important implications. One, it contributes to the existing theoretical knowledge in the areas of MD as well as dead regions. Second, the information derived from this study is clinically useful in the management of individuals with MD. If one is found to be having IHC dysfunctions, the amplification should exclude the frequencies showing IHC dysfunction to minimize the input distortions of the signal. The information is also useful in counseling the individuals about the pathophysiology, prognosis and management strategies.





























