Congenital Stenosis of the Larynx: A Case Report
Rubianne Ligório de Lima1*, Mariana Nagata Cavalheiro1, Rafaela Mabile Ferreira dos Santos Sobreiro1, Vinicius Ribas Fonseca1 and Fabiano Gavazzoni2
1Department of ENT, Hospital da Cruz Vermelha Brasileira, South America
2Department of ETN Service, Hospital Pequeno Principe, South America
Submission: May 05, 2016; Published: October 03, 2016
*Corresponding author: Rubianne Ligório de Lima, Hospital Pequeno Principe, Department of ENT, Hospital da Cruz Vermelha Brasileira, Rua Desembargador motta, 1070, Curitiba Paraná, Brazil, Tel: +4199416723, Email:rubillima@hotmail.com
How to cite this article: Rubianne L d L, Mariana N C, Rafaela M F d S S, Vinicius R F, Fabiano G. Congenital Stenosis of the Larynx: A Case Report. Glob J Otolaryngol. 2016; 2(1): 555578.DOI: 10.19080/GJO.2016.02.555578
Abstract
Introduction: Subglottic stenosis may be considered congenital or acquired. The levels of severity of subglottic stenosis are classified according to the classification system of Myer-Cotton (stages I to IV), to the degree I varying from without obstruction 50% obstruction and grade IV showing no detectable lumen.
Symptoms: Symptoms of acquired and congenital subglottic stenosis are similar and basically involve mild biphasic stridor severe curtailment with episodes of apnea. The diagnosis is made using the flexible laryngoscopy should be performed in all cases. The type of treatment is determined by the extent and degree of airway stenosis involving expectant conduits, expansion and tracheostomy.
Objective: The objective of this study is to report a case of a patient with congenital stenosis of the larynx, being a rare diagnosis and succeeded in making the diagnosis and treatment with symptom improvement.
Case report: B.P.W.L, male and 5 months of age, premature, born vaginally without neonatal resuscitation, hospitalization in ICU or intubation tracheal. It started in the first 5 days of life with mild stridor that was presented progressive worsening. At 10 days of life it was performed an nasofibrolaryngoscopy that showed a posterior subglottic stenosis of 70% with an oval appearance to the level of the cricoid cartilage without progression nasofibroscope of 2.4mm. A series of dilatation balloon was then performed. After the expansion maintained a reduction in the laryngeal lumen of approximately 30%. We chose clinical and expectant management, because the patient would no longer gains with new expansion to showed improvement of symptoms.
Conclusion: Congenital stenosis of the larynx is a rare differential diagnosis of the various causes of stridor in children. The diagnosis is made by fiberoptic laryngoscopy, where we can see the stenosis and classify it as mild to severe and treatment ranges from expectant management to the need for expansion or tracheostomy.
Introduction
The subglottic stenosis may be considered congenital or acquired. Since the advent of prolonged mechanical ventilation in cases of premature babies born with an immature lung development, the incidence of acquired subglottic stenosis is greater than the congenital form. Furthermore, the shape of congenital stenosis tends to be less severe; it is diagnosed when there is a narrowing of the laryngeal lumen, defined as a diameter smaller than 4mm lumen cricoid region and no history of trauma or surgical intubation. The subglottic stenosis may be associated with other congenital anomalies, such as vocal cord paralysis or congenital syndromes, such as Down syndrome [1-3].
Congenital subglottic stenosis may be classified as membranous or cartilaginous. The membranous stenosis is the most common and mildest of congenital stenosis. It is the result of a hypoplastic gland with excessive fibrous connective tissue. Since the cartilaginous stenosis has three common variants: one cricoid cartilage with an abnormally with side shelves, and an elliptical shape, or cricoid cartilage usually shaped with a reduced diameter. The levels of severity of subglottic stenosis are classified according to the classification system of Myer-Cotton (stages I to IV), to the degree I varying from without obstruction 50% obstruction and grade IV showing no detectable lumen [2].
Symptoms of acquired and congenital subglottic stenosis are similar. Symptoms of obstruction of the upper airways prevalent in children who have laryngeal stenosis, although these symptoms vary depending on the location and extent of injury. Obstructive symptoms range from mild to severe stridor obstruction, with episodes of apnea, suprasternal and subcostal retractions, dyspnea and tachypnea. Hypoxia leads to cyanosis and anxiety. Chronic obstruction can cause growth failure. A very characteristic symptom is stridor which tends to be biphasic or inhaling. In mild cases, the symptoms are manifested only during respiratory infections, edema, and when the thick secretions further compromise the way aéreas [1,2,4].
The diagnosis can be made with radiographic techniques, where patients have a classic hourglass subglottic narrowing the column of air. Another method used is the flexible laryngoscopy should be performed in all cases to exclude other pathology of the glottis or supraglottic like paralysis of the vocal cords or laryngomalacia. The definitive diagnosis is made in the operating room using rigid endoscopy. Most patients with congenital subglottic stenosis overcome the disease early in life. Severe cases, however, may require a tracheostomy or tracheal reconstruction using costal cartilage graft for expanding air column subglótica [1].
The symptoms disappear for several years in most cases. The type of surgical intervention is determined by the extent and degree of airway stenosis. Thus, for mild stenosis, the right approach is to wait. For more severe cases of congenital subglottic stenosis, surgery may be necessary. Less than 50% of children need a tracheotomy and most that do can be extubated as the air improves sufficiently. Other surgical options, and anterior decompression laryngotracheal or reconstruction have been advocated to avoid the potential complications of tracheostomy including an increased risk of infection. Dilation and endoscopic laser surgery is ineffective, particularly in stenosis cartilaginosa [2,5,6].
Case Report
B.P.W.L male patient five months of life, coming from Curitiba, 36 weeks of late premature, born vaginally without neonatal resuscitation, hospitalization in ICU or intubation tracheal at any time since its birth. It started in the first 5 days of life with mild stridor that was presenting progressive deterioration leading to difficulty in later feedings. From birth already had a hoarse and mild respiratory distress cry. At 10 days of life it was performed an nasofibrolaryngoscopy that showed a posterior subglottic stenosis of 70% with an oval appearance to the level of the cricoid cartilage without progression nasofibroscope of 2.4mm, where he was diagnosed a congenital subglottic stenosis, since the airway of the patient he had never been manipulated. With 17 days of life was made new nasofibrolaryngoscopy which confirmed this diagnosis and was then chosen to perform balloon dilation as treatment.
This expansion was made with number of balloon 6 and after there was progression of endotracheal tube number 2.5. With 23 days the patient remained respiratory effort and an important biphasic stridor. So we carried out another survey showing reduction of light by approximately 50% with progression of an endotracheal tube number 2 with resistance, and opted to wait for clinical outcome. With 48 days kept the same signs and symptoms that had previously. Being carried out further examination showed that maintain 50% stenosis and then held new balloon dilatation number 6.
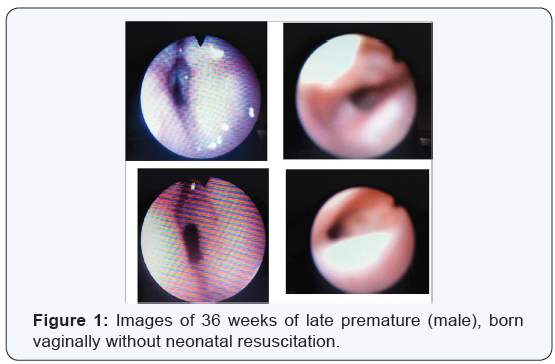
After the expansion maintained a reduction in the laryngeal lumen of approximately 30% with progression cannula number 3 with ease. Still symptoms, but milder, at 2 months and 18 days passed new procedure showed subglottic stenosis in the cricoid further wedge the 50% level, after further expansion progressed easily cannula number 3 and number 3.5 with resistance. Patient held up well without respiratory effort without difficulties feedings and mild stridor. We chose clinical and expectant management, because the patient would no longer gains with new dilations since had no more difficulty breathing (Figure 1).
Conclusion
Congenital stenosis of the larynx is a differential diagnosis of the various causes of stridor in children. We must remember also that it can be classified as congenital or acquired, which is the most common form. The diagnosis is made by fiberoptic laryngoscopy, where we can see the stenosis and classify it as mild to severe and treatment ranges from expectant management to the need for expansion or tracheostomy.
References
- Wiatrak BJ (2000) Congenital anomalies of the lariynx and trachea. Update on the pediatric airway. Otolaryngol Clin North Am 33(1): 91- 110.
- Ahmad SM, Soliman MD (2007) Congenital Anomalies of the Larynx. Otolaryngol Clin N Am 40(1): 177-191.
- Rutter MJ (2014) Congenital laryngeal anomalies. Braz J Otorhinolaryngol 80(6): 533-539.
- Schoeder JW, Holinger LD (2008) Congenital Laryngeal Stenosis. Otolaryngol Clin N Am 41(5): 865-875.
- Miller CK, Kelchner LN, Alarcon A, Willging JP (2014) Compensatory Laryngeal Function and Airway Protection in Children Following Airway Reconstruction. Ann Otol Rhinol Laryngol 123(5): 305-313.
- Ximenes JA, Nakanishi M, Montovani JC (2002) Estenose laríngea em crianças. Arquivos internacionais de otorrinolaringologia 6:181.





























