A Retrospective Study on Profile and Outcomes of Upper Aero Digestive and Bronchial Foreign Bodies from Tertiary Care Institute
David Victor Kumar Irugu1*, CH. Sravan Kumar2, Kapil Sikka2, Amit Chirom Singh2, Hitesh Varma2 and Sridhar Reddy Dandala3
1Department of Otorhinolaryngology and Head & Neck surgery, All India Institute of Medical Sciences, India
2Department of Otorhinolaryngology and Head & Neck surgery, All India Institute of Medical sciences, New Delhi, India
3Department of Otorhinolaryngology and Head & Neck surgery, Osmania Medical College, India
Submission: September 18, 2016; Published: September 27, 2016
*Corresponding author: David Victor Kumar Irugu, Assistant Professor, Department of Otorhinolaryngology and Head & Neck Surgery, Room No- 4057, Academic Block, Fourth Floor, All India Institute of Medical Sciences, Ansari Nagar, New Delhi-110029, India, Tel: +91- 8826509845, Email:dvki2016@gmail.com
How to cite this article: David V K I, CH. Sravan K, Kapil S, Amit C S, Hitesh V, et al. A Retrospective Study on Profile and Outcomes of Upper Aero Digestive and Bronchus Foreign Bodies from Tertiary Care Institute. Glob J Otolaryngol. 2016; 2(1): 555577. 10.19080/GJO.2016.02.555577
Abstract
Objectives: To evaluate the clinical presentations and outcomes of pediatric patients involving FB in upper aero digestive tract.
Material and methods: A retrospective study of 270 patients in one year period (2013- 2014) underwent bronchoscopy and oesophagoscopy for various foreign body ingestion in air and food passages.
Objectives: To evaluate the clinical presentations and outcomes of pediatric patients involving FB in upper aero digestive tract.
Results: Most frequent signs and symptoms of oesophageal and hypopharyngeal foreign bodies were dysphagia, vomiting and drooling of saliva. In cases of foreign bodies of airway, choking, cough, inspiratory stridor and decreased air entry were common. The most common foreign bodies were coins (47.06%) in food passages and ground nut seeds (41.25%) in air passages. We reported two deaths due to local as well as systemic causes.
Conclusion: Utmost care must be exercised during bronchoscopy and oesophagoscopy procedure to avoid injuring the underlying structures. Special care should be exercised in children under six years of age.
Keywords: Foreign body; Choking; Bronchoscopy; Oesophagoscopy; Computer tomography; Necrosis
Introduction
Foreign body (FB) is defined as an endogenous or exogenous substance in an unusual anatomical site [1]. FB in the aero digestive tract is an emergency condition, more common in children between six months to six years of age [2]. FB in the air and food passages is responsible for many accidental deaths at home in children under the age of six years. Children with unexplained dysphagia, dyspnea, cyanosis or wheezing needs comprehensive evaluation for ruling out foreign bodies [1-4]. Carelessness is the most common cause for lodgment of FB in the aero digestive tract [5].
Aim: The aim of the study is to assess the clinical presentations and outcome of the pediatric patients involving FB in aero digestive tract.
Material and Methods
A retrospective study of 270 patients with FB in aero-digestive tract reported to Government ENT Hospital / Osmania Medical College, Hyderabad, Telangana state, India in year 2013- 14. 136 cases were FB’s in Esophagus and 80 patients FB had bronchus in pediatric age group. Out of 136 FB oesophagus
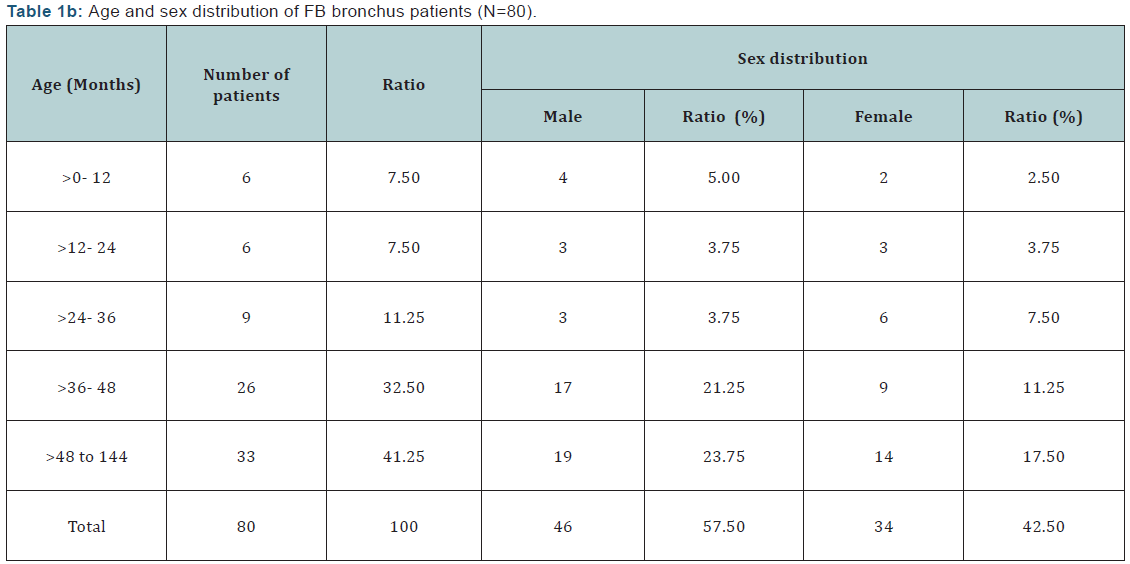
patients, the youngest age was three months & eldest age was 12 years and the incidence was more in males than in females. Among air way foreign bodies, the minimum age was three months and maximum was 11years and males were more than female with 46:34 (Male: Female) ratio in the total of 80 patients. The demography and patient profile are tabulated below (Tables 1a & 1b).

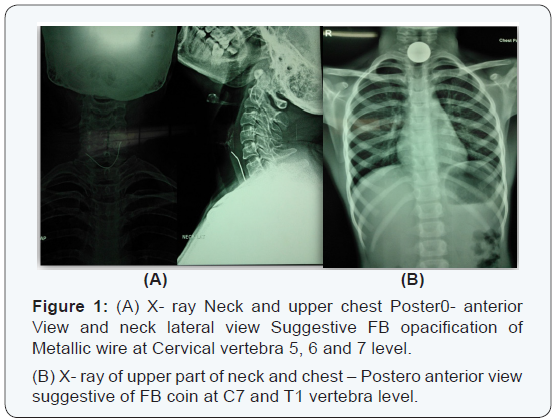
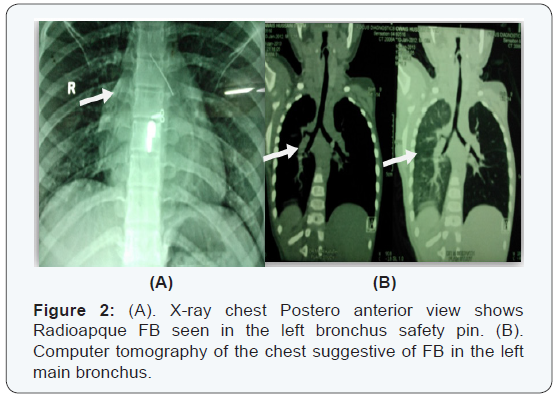
Every patient was admitted and underwent a complete clinical and radiological evaluation with x-ray neck anteroposterior, lateral views and x-ray chest Postero-anterior view for all the cases, except in some selected cases CT chest was done in view of long standing history of FB aspiration ((Figures 1A & 1B)- FB Oesophagus)) and ((Figures 2A & 2B)- FB Bronchus)). Most common signs and symptoms are mentioned below (Table 2). After ambulatory evaluation every patient was posted for FB removal in emergency operating theatre under general anaesthesia. We used oesophagoscopy, upper oesophagoscopy or bronchoscopy depending upon the anatomical location of the FB to remove them. After removal of the FB, the patients were observed in hospital for at least three days in case of FB oesophagus and seven days for FB bronchus with two consecutive normal x-ray chest PA views postoperatively. The patients were followed up for 6 months. There were a total of 54 adult patients excluded from study (FB oesophagus 32 & FB bronchus 14).
Results
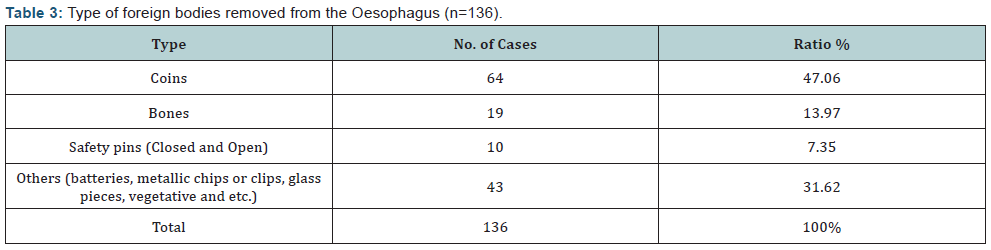
In our series, FB oesophagus was commoner in males (53.68%) than the females (46.32%). The more common age group is 4 to 6 years (27.21%) in male where as in females; foreign bodies are commoner in less than two years of age. However, with the increasing age the incidence decreased (Table 1a). Combinations of symptoms are more common than the single symptom. Here dysphasia and vomiting are the more common complaint (66.51%) than any single symptom. Most common examination findings were pooling of saliva & odynophagia (53.68%) (Table 2). Most common FB seen the oesophagus was the coins (47.06%) (Table 3).
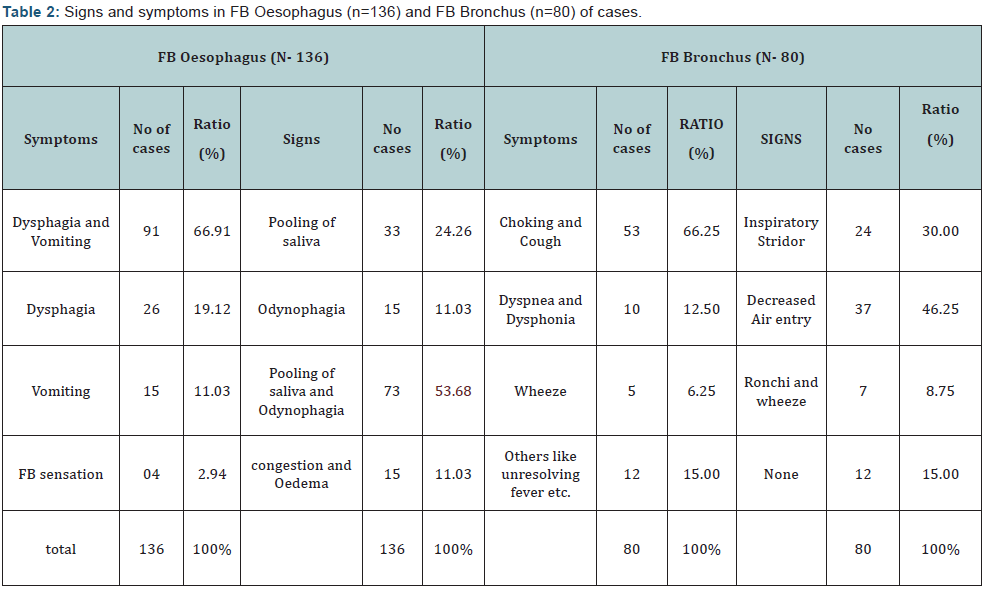
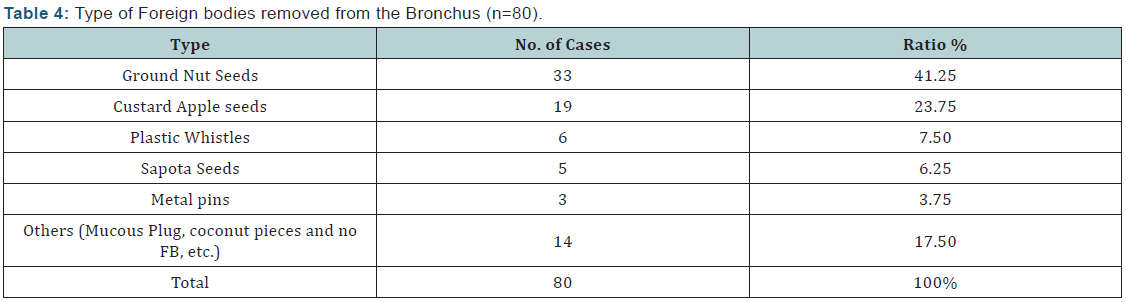
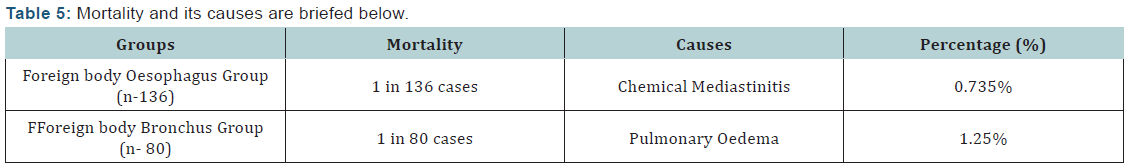
FB bronchus is a life threatening condition which one treats immediately. Bronchial foreign bodies are commonest in three to ten years of age. Incidence in males (57.50%) was higher than females (42.50%) (Table 1b). Cough and choking was most common symptom (66.25%) and decreased air entry onauscultation (46.25%) followed by inspiratory Stridor (30%) are common signs (Table 2). The common FB recovered from the bronchus was the ground nut seeds (41.25%) and custard apple seeds (23.75%) (Table 4). Two patients were died in which one FB battery lodged in oesophagus for one week after successful removal of FB patient developed chemical mediastinitis (1 in 136/ 0.735%).And other patient was 3-year-old female child with foreign body in Rt. Main bronchus for 5 days developed pulmonary oedema after FB removal (1 in 80/ 1.25%) (Table 5).
Discussion
Foreign body (FB) is as an endogenous or exogenous substance in an unusual anatomical site [1]. They are most commonly seen in children from six months to six years of age group. FB bronchus is a life threatening condition and needs to be treated immediately [1,2]. It causes lot of anxiety to parents. FB is more common in the aero digestive passages and occurs due to accidental aspiration or ingestion [3]. There are many causes of FB aspiration and ingestion under consideration, A. Mishra et al. [3] stated that the developmental reflexes of the infant have tendency to keep every object into mouth and this causes more incidence of pediatric FB. Undeveloped molars for grinding, lack of chewing ability, lack of coordination between the swallowing and respiration in young children while playing and laughing causes FB in air food passages [2,6-8].
In Oesophagus foreign bodies are commoner in school going age group but in our study they were more commonly seen in the under two years of age especially in female child. Rural population in India has more sex discrimination than the urban population. Among which difficulty in swallowing along with vomiting and pooling of saliva were common signs and symptoms, Shasanka Shekhar Panda et al. [1], revealed the same. Shasanka Shekhar Panda et al. [1], in their study reported dyspnea and cough to be commonest presenting complaints and ronchi and inspiratory stridor are more common signs. In our study same complaints and signs were observed, however, choking and coughing, decreased air entry was also observed. When there is an inspiratory stridor, wheezing and decreased air entry in a normal healthy playful child with a sudden cessation of breath is more suggestive of FB in the airway and patient need to be evaluated immediately.
In our study most common site of lodgment of FB is was cricopharynx which is a narrow part of food passage while in air passages the important site is trachea and right bronchus. Shasanka Shekhar Panda et al. [1], study suggestive of same as above because of anatomical narrowing of the cervical oesophagus with weak peristalsis and direct accesses to trachea through the laryngeal inlet as well as wide and shortness of the right main bronchus.
- Clear history of aspiration,
- Coughing/ Choking,
- Hoarseness,
- Cyanosis and Gagging.
Other late symptoms include fever, dyspnea and chest pain due to inflammatory reaction. The suspected FB in the aero digestive passages needs to be evaluated immediately by clinical examination and radiological evaluation. The radiological evaluation can provide either direct or indirect evidence. Although X- Ray chests PA view and Soft tissue neck in lateral view is an excellent tool to diagnose the FB oesophagus and also provides information regarding the FB in bronchus, they will not provide diagnosis in case of radiolucent FBs in air and food passages. The direct evaluation with oesophagoscopy and rigid bronchoscopy provides a definitive diagnosis.
Early extraction of the FB bronchus with rigid bronchoscope and FB oesophagus with Oesophagoscopy is important. The most common problem encountered during removal of FB bronchus is hypoventilation to overcome this, smaller size bronchoscope can be used with jet ventilator assisted anesthesia [3,6,8]. Serious complications such as Mediastinal emphysema, Atelectasis, Pneumothorax, Tracheoesophageal fistula and Bronchiectasis have been reported after bronchoscopy [2,8,9]. In our study one patient developed pulmonary edema after successful removal of FB and subsequently died on the 1st post-operative day. This may be due to long time impact of the foreign body which was a seed with multiple spines and the air passages were oedematous.
While removing the FB oesophagus, gentle manipulation is essential. Open safety pins and material with pikes are dangerous and it may cause tearing of the oesophagus. Ingested batteries can cause serious injuries in as little as two hours. When in contact with normal tissue they cause electrolysis reaction producing sodium hydroxide and potassium hydroxide. These hydroxide metabolites cause alkaline burns, liquefaction necrosis and denaturation of proteins in the oesophagus [10]. We lost a three-year-old female girl with one-week history FB battery ingestion. After successful removal of FB and the local site their lot of Charring and extensive tissue necrosis was noticed and a Ryle’s tube was passed. But subsequently the child developed mediastinitis and was referred to cardio-thoracic surgery department for further management, but the child expired after 24 hours.
Recommendations to Parents are [11],
- Should not encourage holding small objects to play. Such objects should be discarded or kept in safe places and closed containers.
- Caregivers should pay attention not to allow the child to put things in their mouth since it is a natural reflex.
- Should not allow eating of nuts, raw vegetables below fours year of age especially while playing and laughing.
- Should not slap the child on the back it causes choking leads lodgment of FB in critical areas.
Summary
- FB in air and food passages is a diagnostic and therapeutic challenge to Otorhinolaryngologist and early evaluation is needed.
- FB is most commonly seen in children from 6 months to 6 years age group.
- The most common location of FB is at the right main bronchus and post cricopharynx.
- Rigid bronchoscopy and oesophagoscopy is the modality of choice to remove the FB.
- The surgeon should be aware of the complications which could occur after rigid bronchoscopy and oesophagoscopy.
- Parents should take preventive measures to avoid these conditions. Prevention is most important factor
Acknowledgement
I am very thankful to Prof. S. Rama Krishna, HOD, Department ENT & HNS, Osmania Medical College, Hyderabad, India.
Conflict of interest
none
There is no funding from any agency.
References
- Kamath P, Bhojwani KM, Prasannaraj T, Abhijith K (2006) Foreign bodies in the aerodigestive tract-a clinical study of cases in the coastal belt of South India. Am J Otolaryngol 27(6): 373-377.
- Panda SS, Bajpai M, Singh A, Baidya DK, Jana M (2014) Foreign body in the bronchus in children: 22 years experience in a tertiary care paediatric centre. Afr J Paediatr Surg 11(3): 252-255.
- Anupam Mishra, GK Shukla, Naresh Bhatia (2000) Aerodigestive Foreign Bodies. Indian Jounal of Pediatrics 67(6): 429-433.
- Dray X, Cattan P (2013) Foreign bodies and caustic lesions. Best Pract Res Clin Gastroenterol 27(5): 679-689.
- BML Abercromby (1945) Foreign Bodies in The Bronchi And Oesophagus In Children. Br Med J 2: 647-648.
- Aydoğan LB, Tuncer U, Soylu L, Kiroğlu M, Ozsahinoglu C (2006) Rigid bronchoscopy for the suspicion of foreign body in the airway. Int J Pediatr Otorhinolaryngol 70(5): 823-828.
- Ragab A, Ebied OM, Zalat S (2007) Scarf pins sharp metallic tracheobronchial foreign bodies: Presentation and management. Int J Pediatr Otorhinolaryngol 71(5): 769-773.
- Tamiru T, Gray PE, Pollock JD (2013) An alternative method of management of pediatric airway foreign bodies in the absence of rigid bronchoscopy. Int J Pediatr Otorhinolaryngol 77(4): 480-482.
- Parag Tambe, LS Kasat, Anagha P Tambe (2005) Epidural emphysema associated with subcutaneous emphysema following foreign body in the airway. Pediatric Surgery International 21(9): 721-722.
- Christopher I. Cruz and Darshan Patel (2013) Clinical Communications: Pediatrics. The Journal of Emergency Medicine 45(1): 30-33.
- Pasquariello PS, Kean H (1975) Cyanosis from a Foreign Body in the Esophagus. Clin Pediatr (Phila) 14(3): 223- 226.





























