An Overview of Management of Hypertension in Clinical Practice
Mudasir Maqbool* and Imran Gani
Department of Pharmaceutical Sciences, University of Kashmir, India
Submission: September 25, 2018; Published: October 23, 2018
*Corresponding author: Mudasir Maqbool, Department of Pharmaceutical Sciences, University of Kashmir, Hazratbal Srinagar-190006, Jammu and Kashmir, India.
How to cite this article: Mudasir M, Imran G. An Overview of Management of Hypertension in Clinical Practice. Glob J Nano. 2018; 4(4): 555641. DOI: 10.19080/GJN.2018.04.555641
Abstract
Hypertension is an important risk factor for the development of cardiovascular morbidity and mortality. In 2002, 10.9% of all deaths in the developed countries were attributable to hypertension, making it the second major risk factor of overall death just below tobacco use (12.2%) but over high cholesterol (7.6%), alcohol use (9.2%) and obesity (7.4%). In addition, about half of all cardiovascular disease (mortality and morbidity combined) is attributable to high blood pressure. High blood pressure in early stages causes no symptoms, so it is easy to ignore. However, if left untreated it can damage vital organs over the years and eventually it can lead to serious complications. Fortunately, it is widely considered as one of the most preventable causes because of the availability of effective antihypertensive drugs. Many pharmacological agents are available for treatment; however, the choice depends on the patients‟ age, diagnosis, co-morbidities, appropriate strength-dosage scheme and patients‟ tolerability. Hypertension can affect all ages despite gender and ethnicity. This review gives a general overview about the management of hypertension.
Keywords: Hypertension; Lifestyle changes; Antihypertensive drugs; Tolerability; Diagnosis
Introduction
Hypertension is an important risk factor for the development of cardiovascular morbidity and mortality. In 2002, 10.9% of all deaths in the developed countries were attributable to hypertension, making it the second major risk factor of overall death just below tobacco use (12.2%) but over high cholesterol (7.6%), alcohol use (9.2%) and obesity (7.4%). In addition, about half of all cardiovascular disease (mortality and morbidity combined) is attributable to high blood pressure. Fortunately, it is widely considered as one of the most preventable causes because of the availability of effective antihypertensive drugs [1]. Arterial hypertension or high blood pressure is a chronic medical condition which is characterized by elevated blood pressure in the arteries and is an important risk factor for future development of cardiovascular disease.
Arterial hypertension belongs to asymptomatic diseases because it usually does not cause symptoms for years until a vital organ is damaged [2]. Hypertension is reported to be the fourth contributor to premature mortality in developed countries and the seventh in developing countries. Almost 12.8% (7.5 million) of the total deaths and around 3.7% of the total DALYS (disability adjusted life years) are due to raised blood pressure (BP) [3,4]. Recent epidemiological data suggest both an increase in the prevalence (urban: 25% and rural: 10-15%) and poor levels of control of hypertension in India [4,5].
Hypertension is a major health problem throughout the world because of its high prevalence and its association with increased risk of cardiovascular disease. Advances in the diagnosis and treatment of hypertension have played a major role in recent dramatic declines in coronary heart disease and stroke mortality in industrialized countries [6]. However, in many of these countries, the control rates for high blood pressure have actually slowed in the last few years. It is estimated that by 2010, 1.2 billion people will be suffering hypertension worldwide. Elevated BP is an established risk factor for cardiovascular disease. The relationship between BP level and cardiovascular risk is continuous, therefore the distinction between normotension and hypertension is arbitrary [7,8].
Appropriate management of hypertension reduces the risk for cardiovascular disease, renal disease, cerebrovascular disease, and death [9-12]. However, determining the most appropriate BP targets, particularly for adults aged 60 years or older, has been controversial. Debate about the goal for systolic BP (SBP) among adults treated for hypertension has intensified, especially in light of recent recommendations [13].
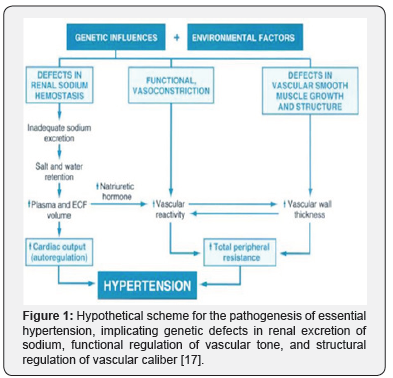
Blood pressure is represented by two values. The higher value called systolic is the highest pressure in the arteries when the heart contracts (systole). The lower value is the lowest pressure in the arteries when the heart relaxes between beats (diastole).Arterial hypertension for adults, who don’t suffer from any other kind of diseases, is defined by an elevation of blood pressure to 140 / 90 mm Hg or to higher values [14,15]. On the table below there is a classification of arterial blood pressure according to European Society of Hypertension (ESH) [16] (Table 1 & Figure 1).

Management of Hypertension
All patients should be managed with non-pharmacologic interventions/therapeutic lifestyle modifications to lower BP. Patients with pre-hypertension should be followed up yearly to detect and treat HPT as early as possible. Decisions regarding pharmacological treatment should be based on the individual patient’s global cardiovascular risk. In subjects with MEDIUM RISK or HIGHER, the threshold for commencing HPT treatment should be lower. Therapeutic lifestyle changes should be recommended for all individuals with HPT and pre-HPT. It may be the only treatment necessary in Stage 1 HPT. A high degree of motivation is also needed to sustain the benefits of nonpharmacological treatment. It is also important to remember that lifestyle modification requires a concerted effort and reinforcement on behalf of the practitioner. Lifestyle modification works better with concurrent behavioral intervention than just passive advice. This non-pharmacological management includes weight reduction, sodium restriction, avoidance of alcohol intake, regular physical exercise, healthy eating and cessation of smoking [18].
Weight reduction
Weight-reducing diets in overweight hypertensive persons can result in modest weight loss in the range of 3-9% of body weight [19] and are associated with blood pressure reduction of about 3-6 mmHg. It is advisable for overweight hypertensive patients to lose at least 5% of their weight.
Sodium intake
High salt intake is associated with significantly increased risk of stroke and total cardiovascular disease [20]. Evidence from published systematic review and meta analyses showed that restricting sodium intake in people with elevated blood pressure in the short term leads to reductions in blood pressure of up to 10.5 mmHg systolic and 2 mmHg diastolic [20-22]. An intake of <100 mmol of sodium or 6g of sodium chloride a day is recommended (equivalent to <1¼ teaspoonfuls of salt or 3 teaspoonfuls of monosodium glutamate) [23-26].
Avoidance of alcohol intake
Alcohol consumption elevates BP acutely. For those who consume alcohol, intake should be restricted to no more than 21 units for men and 14 units for women per week (1 unit is equivalent to one half-pint of beer or 100 ml of wine or 20 ml of “proof whisky”). Meta analyses have shown that, interventions to reduce alcohol consumption caused a small but significant reduction (3.3/2 mmHg) in both systolic and diastolic blood respectively [27]. Hypertensives who are heavy drinkers are also more likely to have hypertension resistant to drug treatment. The only way to reduce these patients’ BP effectively is by reducing or stopping their alcohol intake [28].
Regular physical exercise
Aerobic exercise is more effective than resistance training (e.g., weight lifting) [29]. Exercise like walking-jogging can result in a reduction of 13/18 mmHg in SBP/DBP [30]. More recent evidence showed that resistant exercise is effective in lowering blood pressure among normotensives and pre-hypertensives but not among hypertensives [31]. However isometric resistant exercise can reduce BP by 10.4/6.7 mmHg as shown by a recent meta-analysis [32]. General advice on cardiovascular health would be for modest exercise, such as brisk walking for a total of at least 150 mins per week [33,34].
Healthy eating
A diet rich in fruits, vegetables and low-fat dairy products with reduced saturated and total fat can substantially lower BP (11/6 mmHg in hypertensive patients and 4/2 mmHg in patients with high normal BP). 55 (Level I) More recently, diet high in L-Arginine has been shown to be able to reduce BP by 5.4/2.3 mmHg [35].
Cessation of smoking
Smoking can raise BP acutely. However, the effect of chronic smoking on BP is less clear. Nevertheless, smoking cessation is important in reducing overall cardiovascular risk.
Relaxation therapy
Relaxation interventions were shown to be associated with statistically significant reductions in systolic and diastolic blood pressure of about 3 mmHg [34]. However, another systematic review of studies on the effect of stress reduction on blood pressure found small and non-significant effect on blood pressure [36]. It is not recommended for routine provision in primary care.
Others
These include micronutrient alterations, caffeine reduction and dietary supplementation with fish oil, potassium, calcium, magnesium and fibre. However, the evidence for its beneficial effect is limited [37-40]. In summary while weight reducing diet, regular exercise, alcohol and salt restriction have been consistently shown to be beneficial in reducing BP in patients, the evidence thus far has not been consistent for relaxation therapies and supplementations with calcium, magnesium or potassium [41] (Table 2).

Pharmacotherapy
It has been proved by way of a large number of RCTs that by lowering the blood pressure values in hypertensive subjects the subsequent complications of HT can be reduced. Though some trials depict superiority of one class of antihypertensive drug over other types, meta-analyses from trials of larger sample size have failed to show clinically significant differences between drug classes and hence the beneficial effects of BP lowering are largely independent of the drugs employed [43,44]. Lifestyle modifications can be very effective but in real life patients usually need a combination of them with pharmacological therapy. Very often they need more than one type of anti-hypertensive medication or combination of more in order to achieve their blood pressure target goal.
Combination of lifestyle modifications and pharmacological medication may allow reduction of drugs doses, better therapeutic control, more effective treatment and prevention of other cardiovascular risks factors [2,16,45].
Classification of Antihypertensive Agents [2,16]
a) Antagonists of β-adrenoreceptors (Beta-blockers).
b) Diuretics (mainly thiazide, loop and potassium sparing).
c) Calcium channel blockers (dihydropyridines – non dihydropyridines).
d) Angiotensin cconverting enzyme inhibitors (ACEis).
e) Angiotensin II receptors blockers (Sartans).
f) Direct inhibitors of renin (Aliskiren-New in therapy, lack of experience) (Table 3).
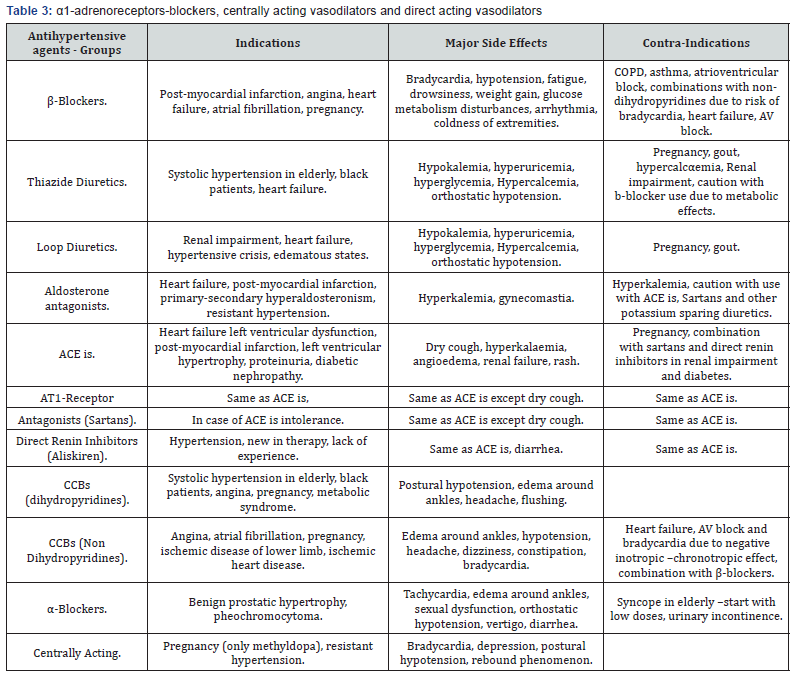
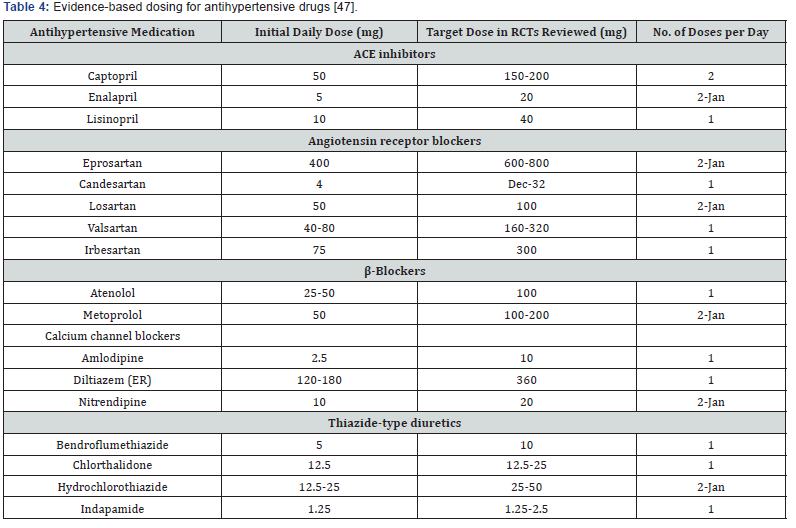
For better pharmacological treatment outcomes, drugs should be chosen on the basis of efficacy, safety, convenience to the patient and cost. For assessment of efficacy evidence from large scale clinical trials should be used. Moreover, recognition of adverse effects is another important factor because is associated with patient adherence and effectiveness of treatment. In addition, the use of regimens (FDC) that is more convenient to the patient like once-daily regimens and also cost of treatment are other important factors because could help to improve the patient compliance [46] (Table 4).
Conclusion
In conclusion arterial hypertension is an important risk factor for cardiovascular diseases and also contributes to increased morbidity and mortality. Hypertension’ is indeed a major public health problem accounting for drastic downward shifts in the economic progress of a country. That too in a country like India, the impact of this dreadful disease on the healthcare system as a whole is humongous. Figures portray that about Rs. 43 billion of the annual income among the adult working class in our country is spent for the management of HT. Suboptimal control of BP is the most common attributable risk for death worldwide. HT goals can be achieved and maintained only by a team-based approach with aid from all health personnel like general physicians, medical specialists, trained nurses, dieticians and pharmacists. Moreover, studies have shown the significance of multi-disciplinary approach in the management of HT. Emphasis should also be on strict lifestyle modifications which act as the cornerstone for prevention and treatment of HT
Many pharmacological agents are available for treatment; however, the choice depends on the patients‟ age, diagnosis, comorbidities, appropriate strength-dosage scheme and patients‟ tolerability. Hypertension can affect all ages despite gender and ethnicity. Lifestyle modifications, including weight loss, reduction of dietary sodium intake, aerobic physical activity of at least 30 minutes a day at least three times a week, and a reduction in alcohol consumption, are a relatively cost-effective way to reduce high blood pressure. There is wide variability in the cost of antihypertensive medications; newer and more expensive agents have not been shown to be significantly safer or more effective than many older, well-established medications that are available in generic form. Fixed combinations of antihypertensive medications offer less dosing flexibility and are often substantially more expensive than prescribing the component medications independently. It is our goal to not just decrease the risk of CV diseases brought about by elevated BPs but to prolong their lives as well.
References
- (2006) The Atlas of Heart Disease and Stroke.
- Walker R, Whittlesea C (2012) Clinical Pharmacy and Therapeutics- Hypertension. (5th edn.), Churchill Livingstone, Elsevier, UK, pp: 295- 307.
- Victor RG (2012) Arterial hypertension, Goldman’s Cecil Medicine. In: Goldman L, Schafer AI, (24th edn.), Elsevier Saunders, UK.
- (2013) Special issue on Indian guidelines on hypertension (I.G.H.) p: 61.
- (2014) Hypertension the silent killer (Weekend edition), The New Sunday Express Magazine, India, p: 1-2.
- (1997) Sixth report of the Joint National Committee on prevention. detection, evaluation, and treatment of high blood pressure. Archives of Internal Medicine 157(21): 2413-2446.
- Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, et al. (2013) ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 31(7): 1281-1357.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, et al. (1967) Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360(9349): 1903-1913.
- (1967) Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg, JAMA 202(11): 1028-1034.
- (1992) Medical Research Council trial of treatment of hypertension in older adults: principal results. MRC Working Party, BMJ 304(6824): 405-412.
- (1970) Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA 213(7): 1143-1152.
- (1980) The Australian therapeutic trial in mild hypertension. Report by the Management Committee, Lancet 1: 1261-1267.
- James PA, Oparil S, Carter BL, Cushman WC (2014) evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311(5): 507-520.
- (2012) American Heart Association (AHA): Understand Your Risk for High Blood Pressure.
- (2012) American Heart Association (AHA): Understanding Blood Pressure Readings.
- Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, et al. (2013) European Society of Hypertension (ESH) Guidelines and European Society of Cardiology (ESC) for Management of Hypertension; Greek Translation of Hypertension J 31(7): 1281-1357.
- Raj GM, Priyadarshini R, Mathaiyan J (2015) Current Perspectives in the Management of Hypertension. SAJ Cardiol 1(1): 1-3.
- AR Abdul Rashid, Y Khalid, YC Chia (2011) Management of Hypertension Malays Fam Physician 6(1): 40-43.
- Siebenhofer A, Jeitler K, Berghold A, Waltering A, Hemkens LG, et al. (2011) Long-term effects of weight reducing diets in hypertensive patients. Cochcrane Database Syst Rev 7(9): CD008264.
- Taylor RS, Ashton KE, Moxham T, Hooper L, Ebrahim S, et al. (2011) Reduced dietary salt for the prevention of cardiovascular disease: a meta-analysis of randomized controlled trials (Cochrane review). Am J Hypertens 24(8): 843-853.
- Graudal NA, Hubeck-Graudal T, Jürgens G (2012) Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review). Am J Hypertens 25(1): 1-15.
- Jürgens G, Graudal NA (2004) Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride. Cochrane Database Syst Rev 1: CD004022
- He FJ, MacGregor GA (2004) Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev 3: CD004937
- (1997) Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention Collaborative Research Group. The Trials of Hypertension Prevention, Phase II. Arch Intern Med 157(6): 657-667.
- Graudal NA, Galloe AM, Garred P (1998) Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols and triglyceride: A meta-analysis. JAMA 279(17): 1383-1391
- Norimah AK Jr, Safiah M, Jamal K, Haslinda S, Zuhaida H, et al. (2008) Food Consumption Patterns: Findings from the Malaysian Adult Nutrition Survey (MANS). Malays J Nutr 14(1): 25-39.
- Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, et al. (2001) Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 38(5): 1112-1117.
- Morgan TO (2000) Hypertension: Dietary and Lifestyle Measures in a Nutshell. Medical Progress 26(7): 5-9.
- Halbert JA, Silagy CA, Finucane P, Withers RT, Hamdorf PA, et al. (1997) The effectiveness of exercise training in lowering blood pressure: a meta-analysis of randomized controlled trials of 4 weeks or longer. J Hum Hypertens 11(10): 641-649
- Petrella RJ (1998) How effective is exercise training for treatment of hypertension? Clin J Sport Med 8(3): 224-231.
- Cornelissen VA, Fgard RH, Coeckelberghs E (2011) Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension 58(5): 950-958.
- Owen A, Wiles J, Swaine I (2010) Effect of isometric exercise on resting blood pressure: a meta-analysis. J Hum Hypertens 24(12): 796-800.
- Rogers MW, Probst MM, Gruber JJ, Berger R, Boone JB (1996) Differential effects of exercise training intensity on blood pressure and cardiovascular responses to stress in borderline hypertensive humans. J Hypertens 14(11): 1369-1375.
- Ebrahim S, Smith GD (1998) Lowering blood pressure: a systematic review of sustained effects of nonpharmacological interventions. J Public Health Med 20(4): 441-448.
- Dong JY, Qin LQ, Zhang Z (2011) Effect of oral L-arginine supplementation on blood pressure: a meta-analysis of randomized, double blind, placebo-controlled trials. Am Heart J 162(6): 959-965.
- Dickinson HO, Beyer FR, Ford GA, Nicolson DJ, Cook JV, et al. (2008) Relaxation therapies for the management of primary hypertension in adults. Cochrane Database Syst Rev 1(23): CD004935.
- Dickinson HO, Nicolson D, Cook JV, Campbell F, Beyer FR, et al. (2006) Calcium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev 2: CD004639.
- Beyer FR, Dickinson HO, Nicolson D, Ford GA, Mason J (2006) Combined calcium, magnesium and potassium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev 19(3): CD004805
- Dickinson HO, Nicolson D, Campbell F, Cook JV, Beyer FR, et al. (2006) Magnesium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev 19(3): CD004640.
- Dickinson HO, Nicolson D, Campbell F, Beyer FR, Mason J (2006) Potassium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev 19(3): CD004641.
- Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, et al. (2006) Lifestyle interventions to reduce raised blood pressure: a systematic review of randomsied controlled trials. J Hypertens 24(2):215-233.
- Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, et al. (2013) Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the american heart association. Hypertension 61(6): 1360-1383.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. (2003) The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JNC 7 report. JAMA 289(19): 2560-2572.
- Mancia G, Fagard R, Narkiewicz K, Redόn J, Zanchetti A, et al. (2013) ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34(28): 2159-2219.
- Wald D, Law M, Morris JK, Bestwick JP, Wald NJ (2009) Combination Therapy Versus Monotherapy in Reducing Blood Pressure: Meta- Analysis on 11000 Participants From 42 Trials. Amer J Medic 122(3): 290-300.
- Gupta A, Arshad S, Poulter NR (2010) Compliance, Safety and Effectiveness of Fixed-Dose Combinations of Antihypertensive Agents: A Meta-Analysis. Hypertension 55(2): 399-407.
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, et al. (2014) Evidence-based guideline for the management of high blood pressure in adults. Report from the panel appointed to the Eighth Joint National Committee (JNC 8). JAMA 311(5): 507-520.






























