Ileal Gastrointestinal Stromal Tumors Mimicking Gynecologic Masses: A Single Institutional Experience
Anna Myriam Perrone1*, Giulia Dondi1, Margherita Nannini2, Antonio De Leo3, Donatella Santini3, Maristella Saponara2, Marco Tesei1, Maria Pantaleo2 and Pierandrea De Iaco1
1 Department of Gynaecological Oncology Unit, S Orsola-Malpighi Hospital, Italy
2Department of Specialized, Experimental and Diagnostic Medicine, S Orsola-Malpighi Hospital, Italy
3 Department of Pathology Service, Addarii Institute of Oncology, S Orsola-Malpighi Hospital, Italy
Submission: July 19, 2018; Published: October 31, 2018
*Corresponding author: Anna Myriam Perrone, Department of Gynaecological Oncology Unit, S Orsola-Malpighi Hospital, Via Massarenti 13, 40138 Bologna, Italy.
How to cite this article: Anna Myriam P, Giulia D, Margherita N, Antonio D L, Donatella S, et al. Ileal Gastrointestinal Stromal Tumors Mimicking Gynecologic Masses: A Single Institutional Experience. Curr Trends Clin Med Imaging. 2018; 2(4): 555594. DOI: 10.19080/CTCMI.2018.02.555594
Abstract
A gastrointestinal stromal tumor (GIST) has a wide spectrum of clinical presentations. Occasionally it can be diagnosed as an asymptomatic pelvic mass detected by chance by trans-vaginal ultrasound and wrongly diagnosed as a mass of gynecologic origin. In literature 35 cases of ileal GISTs mimicking gynecologic masses have been described. We report five cases of female patients referred to our institution from March 2013 to January 2017, presenting with a pelvic mass at trans-vaginal ultrasound resulting, at final histologic examination, in an ileal GIST. We also describe in detail the trans-vaginal sonographic features.
Keywords: Ileal gastrointestinal stromal tumor; Gynaecologic mass; Trans-vaginal ultrasound; Ovarian mass
Abbrevations: GISTs: Gastrointestinal Stromal Tumors; TVU: trans-vaginal ultrasound; CT: Computed Tomography; 18F-FDG PET: 18-Fluorodeoxyglucose Positron Emission Tomography; MRI: Magnetic Resonance Imaging
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common mesenchimal neoplasm of the gastrointestinal tract. The small intestine is the second predominant site of origin of GISTs. Ileal GISTs have a wide spectrum of clinical presentations, ranging from asymptomatic incidental nodules to acute abdominal pain, intestinal obstruction or tumor rupture with intra-abdominal hemorrhage [1,2]. On rare occasions, ileal GISTs can be diagnosed as an asymptomatic pelvic mass detected by chance through trans-vaginal ultrasound (TVU) and thus wrongly diagnosed as a gynecologic tumor.
To date, in literature 35 cases of ileal GISTs mimicking gynecologic masses have been described [3-11]. The aim of this study was to review and describe ileal GISTs mimicking gynecologic tumors among female patients with an ileal GIST referred to our Center. We retrospectively reviewed the records of 64 female patients with diagnosis of ileal GIST from our database collected from January 2001 to January 2017. Five patients with a pelvic mass evaluated by a gynecologist as the first diagnostic step were selected.
Results
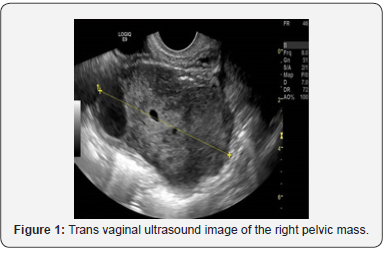
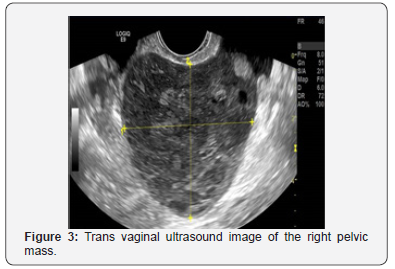
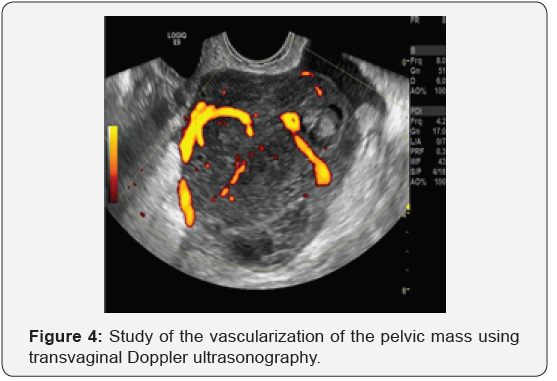
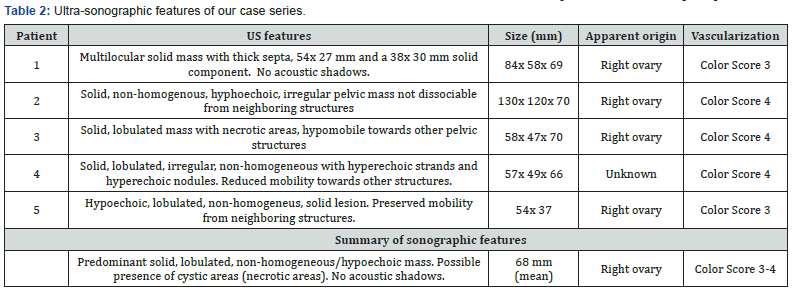
Characteristics of cases are listed in Table 1. Clinically, one patient was asymptomatic, and the mass was found during a routine gynecological consultation by TVU, two presented with abdominal pain, one with melena and one with left inguinal swelling. CA 125 was negative or mildly increased (< 170 U/ml) in all patients. TVU appearances of the pelvic mass are reported in Table 2. The lesions were mainly solid, inhomogeneous and hypoechoic in all cases (Figures 1 & 2). In four cases it was described as a “lobulated mass”. Cystic areas due to necrosis was described in one patient. No acoustic shadows were observed in all cases. The masses had no adhesion to the pelvic structures in three cases and were localized in the rightpelvismimicking a right ovarian lesion in four cases. All cases showed high vascularization at TVU (Figures 3 & 4).
In all cases a computed tomography (CT) scan showed a lobulated pelvic mass with contrast enhancement suggesting ovarian neoplasia. 18F-FDG PET/CT was performed in three patients: it showed a pathological up-take in one case only. In one case pelvic magnetic resonance imaging (MRI) was performed and confirmed the presence of a right adnexal mass. All patients underwent surgery in our Gynecologic Oncology Unit. A laparotomic ileal resection was performed in all cases. Hysterectomy and bilateral salpingo-oophorectomy were performed in two cases and left salpingo-oophorectomy in one. Pelvic peritonectomy and removal of peritoneal nodules and omentum was necessary in two patients with advanced disease. Four patients achieved complete cytoreduction at the end of surgery.
The median size of the ileal GIST was 7.5cm ranging from 6.5cm to 17cm. Histology confirmed infiltration of pelvic, abdominal, mesenteric and right diaphragmatic peritoneum and omentum in the patient with residual disease after surgery and bilateral ovarian metastases with infiltration of left Douglas pouch peritoneum in the other patient with advanced disease. All patients presented an intermediate or high risk of relapse according to Mittie’s classification. Imatinib at the standard dose of 400 mg daily was started in three patients however in two cases this was discontinued due to intolerance after a few months. One patient commenced a surveillance program due to the mutational status (any exon 8, 9, 11, 13, 17 exons KIT or 12, 14, 18 exons PDGFRA mutations).

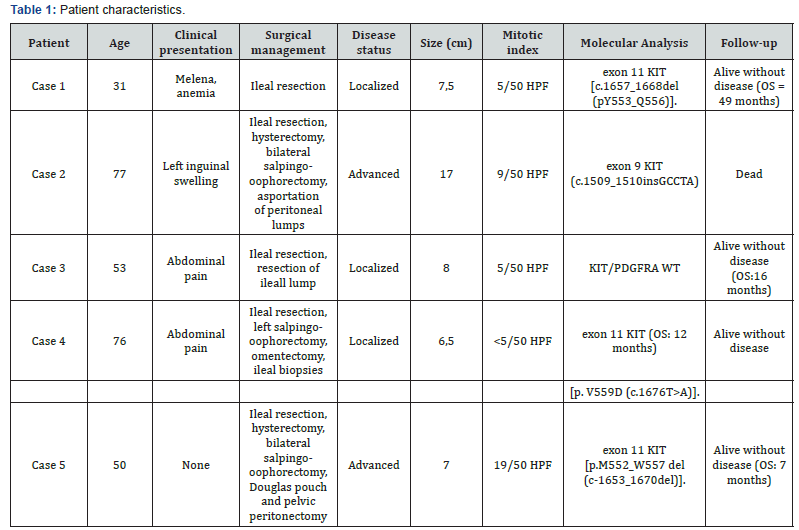
In the patient with persistence of abdominal disease there was a mutation in KIT exon 9 and therefore Imatinib at the dose of 800mg/daily was started but discontinued soon due to heart failure. This was then restarted at the reduced dose of 400mg daily. At progression of the disease, a second line therapy with Sunitinib at the low dose of 25mg/daily was started. This patient died of disease 44 months later. At the time of writing four patients are in follow-up alive without disease.
Conclusion
Ileal GISTs have a wide spectrum of clinical presentations, they can occasionally present as pelvic masses and wrongly be of gynecologic origin [3-11]. In this case series we tried to create some tips and advice to better recognize ileal GIST mimicking pelvic mass. From a sonographic point of view, after reviewing all images, we found some peculiar features: the mass frequently appeared solid, irregular, hypo-echoic, with small anechoic parts, without acoustic shadows, highly vascularized, frequently dislocated in the right pelvis mimicking a right ovarian neoplasia and the median diameter was 68 mm (Table 2). The pelvic mass had generally no signs of adhesions to other pelvic organs. The sonographic features of the cases previously reported in the literature are like those reported in our series [3-11].
Clinical presentation in our case series and in literature was heterogeneous and nonspecific and this does not permit differential diagnosis between GISTs and ovarian tumors. If we consider other cases described in literature [3-11], abdominal or pelvic pain is the most frequent symptom, probably due to the enlargement of the mass and compression of pelvic structures.
18F-FDG PET is used mainly in the detection of tumor response to treatment because GISTs frequently demonstrate high 18F -FDG avidity but in our patients the avidity was high in only one case out of three.
These observations underline that in some cases the traditional radiological techniques may be inadequate in the identification of the origin of a GIST located in the pelvis whereas for ovarian masses TVU can be more useful than a CT scan for diagnosis and definition of the lesion. Moreover, we tried to identify other differences between GISTs and early stage ovarian cancer. Normal or mild serum levels of CA 125 (< 170 U/ml) and the absence of free fluid in the Douglas pouch can be considered ancillary features for suspicion of GIST.
After our analysis two issues arose; whether the pelvic GIST should be treated by a gynecologist or a general surgeon and what is the appropriate work-up in the case of suspected GIST. Surgery of ileal GIST requires a gastrointestinal surgeon, but the role of a gynecologic surgeon can be relevant if GIST involves the genital tract and hysterectomy and sapling-oophorectomy may be required. The principle of GIST surgery is the achievement of a complete excision of the disease with negative margins, avoiding intraoperative tumor rupture. Imatinib pre-operative treatment represents the standard of care in locally advanced GIST. In this context, histological examination by multiple core needle biopsies of the mass should be considered with the aim of achieving a histological diagnosis and the molecular status, necessary for medical treatment [12].
The hypothetical risk of cell seeding into the abdominal cavity and conversion of a local GIST into a disseminated one is present, however the ESMO/European Sarcoma Network Working Group guidelines and the National Comprehensive Cancer Network guidelines of the United States of America accept the procedure if the biopsy is properly carried out in specialized centers. According to Eriksson et.al. a preoperative diagnostic percutaneous biopsy of a suspected GIST did not increase the risk of GIST recurrence in a patient population who receive adjuvant Imatinib after biopsy [13]. Similarly a trans-vaginal biopsy probably would not increase the risk of dissemination.
Moreover, a pre-operative diagnosis allows us to plan the appropriate surgical strategy for GIST and to avoid the risk of rupture during surgical manipulation, since it represents a validated poor prognostic factor [14]. Attention must be paid to the possibility of ovarian metastases from GIST that, even though rare, can occur [15]. We suggest that careful evaluation of both ovaries by TVU must be included in the pre-operative work-up as well as during follow-up. We invite gynecologists to consider a GIST in the case of atypical solid pelvic mass without a CA125 increase and ascites. If GIST is suspected a surgical approach is suggested if complete removal of the disease is possible and if it does not require multi-visceral resection, otherwise preoperative medical treatment is recommended. A gynecologic evaluation should be proposed in patients with a history of GIST because of the possibility of metastases to the genital tract. Increasing clinical records of GISTs mimicking pelvic masses have been reported, further collection and sharing of data is needed and the creation of a network between gynecologists, gastrointestinal surgeons and oncologists must be encouraged.
If GIST is suspected a surgical approach is suggested if complete removal of the disease is possible and if it does not require multi-visceral resection, otherwise pre-operative medical treatment is recommended. A gynecologic evaluation should be proposed in patients with a history of GIST because of the possibility of metastases to the genital tract. Increasing clinical records of GISTs mimicking pelvic masses have been reported, further collection and sharing of data is needed and the creation of a network between gynecologists, gastrointestinal surgeons and oncologists must be encouraged.
Acknowledgements
Conflict of interest the authors whose names are listed immediately below certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non- financial interest in the subject matter or materials discussed in this manuscript.
References
- Biasco G1, Velo D, Angriman I, Astorino M, Baldan A, et al. (2009) Gastrointestinal stromal tumors: report of an audit and review of the literature. Eur J Cancer Prev 18(2):106-16.
- DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, et al. (2000) Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 231(1): 51-58.
- Dayan E, Zhu H, Copperman AB, Lewis S, Kamath A (2017) Gastrointestinal stromal tumor presenting as a right adnexal mass with histopathologic correlation. Clin Imaging 44: 97-100.
- Ijeri SK, Rathod PS, Kundargi R, Pallavi VR, Shobha K, et al. (2016) Gastrointestinal Stromal Tumor Mimicking as Ovarian Tumor in Gynaecologic Oncology. Indian J Surg Oncol 7(1): 56-61.
- Karaca N, Akpak YK, Tatar Z, Batmaz G, Erken A (2015) Gastrointestinal Stromal Tumor: May Mimic Adnexal Mass. Glob J Health Sci 8(2): 20-26.
- Muñoz M, Ramirez PT, Echeverri C, Alvarez LG, Palomino MA, et al. (2012) Gastrointestinal stromal tumors as an incidental finding in patients with a presumptive diagnosis of ovarian cancer. J Gynecol Oncol 23(1): 48-52.
- Teoh WC, Teo SY, Ong CL (2011) Gastrointestinal stromal tumors presenting as gynecological masses: usefulness of multidetector computed tomography. Ultrasound Obstet Gynecol 37(1): 107-9.
- Angioli R, Battista C, Muzii L, Terracina GM, Cafà EV, et al. (2009) A gastrointestinal stromal tumor presenting as a pelvic mass: A case report. Oncol Rep 21(4): 899-902.
- Pinto V, Ingravallo G, Cicinelli E, Pintucci A, Sambati GS et al. (2007) Gastrointestinal stromal tumors mimicking gynecological masses on ultrasound: a report of two cases. Ultrasound Obstet Gynecol 30(3): 359-61.
- Morimura Y, Yamashita N, Koyama N, Ohzeki T, Takayama T, et al. (2006) Gastrointestinal stromal tumor mimicking gynecological disease. Fukushima J Med Sci 52: 21-8.
- Zighelboim I, Henao G, Kunda A, Gutierrez C, Edwards C (2003) Gastrointestinal stromal tumor presenting as a pelvic mass. Gynecol Oncol 91(3): 630-635.
- ESMO/European Sarcoma Network Working Group (2014) Gastrointestinal stromal tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25 Suppl 3: iii21-6.
- Eriksson M, Reichardt P, Sundby Hall K (2016) Needle biopsy through the abdominal wall for the diagnosis of gastrointestinal stromal tumourdoes it increase the risk for tumour cell seeding and recurrence? Eur J Cancer 59: 128-33.
- Hohenberger P, Ronellenfitsch U, Oladeji O, Pink D, Ströbel P, et al. (2010) Pattern of recurrence in patients with ruptured primary gastrointestinal stromal tumour. Br J Surg 97(12): 1854-1859.
- De Leo A, Nannini M, Dondi G, Santini D, Urbini M, et al. (2018) Unusual bilateral ovarian metastases from ileal gastrointestinal stromal tumor (GIST): a case report. BMC Cancer 18(1): 301.






























