Abstract
This study examined differences in mental health outcomes, substance use behaviors, and treatment access by state income level and age group (18-25 vs. 26+) in the United States. Using chi-square tests and two-proportion Z-tests, we found that individuals aged 18-25 had significantly higher rates of Any Mental Illness (AMI), Serious Mental Illness (SMI), and Attempted Suicide (AS), while tobacco and alcohol use were more prevalent among those aged 26 and older. Higher-income states had significantly higher rates of AMI, SMI, illicit drug use, and alcohol use, as well as greater access to mental health treatment. Notably, both the proportions of individuals who received substance use treatment (RSUT) and those who needed but did not receive treatment (NRSUT) are higher compared to lower-income states. This suggests that despite greater access to treatment, a considerable unmet need for substance use care persists even in resource-rich environments. Tobacco use was more common in lower-income states, and no significant differences were observed in suicide attempts between income groups. These findings underscore the influence of socioeconomic and age-related factors on behavioral health disparities.
Keywords:Mental health disparities; Substance use behaviors; Tobacco use; Behavioral health; Serious Mental Illness; Any Mental Illness; Illicit drug use
Abbreviations: AMI: Any Mental Illness, SMI: Serious Mental Illness, AS: Attempted Suicide; NIMH: National Institute of Mental Health; WHO: World Health Organization; NSDUH: National Survey on Drug Use and Health; ACS: American Community Survey;
Introduction
Even though mental health is a vital component of a person’s total wellbeing, it is still a taboo and frequently disregarded topic in society. In the words of former US President Bill Clinton,
“Mental illness is nothing to be ashamed of, but stigma and bias shame us all.” [1]
Similarly, actress and mental health advocate Glenn Close emphasized the importance of open discussions, stating,
“What mental health needs is more sunlight, more candor, and more unashamed conversation.” [2]
Despite growing awareness and advocacy, mental illness continues to affect millions of people in the United States, with young adults being particularly vulnerable.
The National Institute of Mental Health (NIMH) claims that, approximately 59.3 million adults in the U.S. experienced mental illness in 2022, with 23.1 million suffering from serious mental health conditions [3]. Young adults aged 18-25 face heightened risks, exhibiting higher rates of mental health disorders, substance use, and suicidal behaviors compared to older age groups. The World Health Organization (WHO) underscores the essential role of mental health, stating, “Indeed, there is no health without mental health” [4]. Mental health is defined as a state in which individuals can realize their abilities, manage stress, work productively, and contribute to their communities. However, various economic and behavioral factors influence mental health outcomes, contributing to disparities across different populations and regions.
Numerous studies have established a connection between economic circumstances and outcomes related to mental health. According to McLaughlin [5], those with lower incomes are more likely to suffer from depression, anxiety, and substance use disorders because they are under financial strain, have less access to healthcare, and are more likely to face negative life events. Unemployment has been identified as a major risk factor, with studies indicating that job insecurity increases stress, depression, and suicidal ideation [6].
Interestingly, while higher income is generally associated with better mental health, some research suggests that high median household income can contribute to increased mental illness. Work-related stress, financial pressures, and competitive environments may lead to anxiety, depression, and burnout [7-9]. The relationship between substance uses and mental health is well-documented. Individuals with mental health disorders are significantly more likely to use alcohol, tobacco, and illicit drugs, often as a means of coping with psychological distress [10]. However, substance use can also exacerbate mental health conditions, creating a cycle of dependency and distress. Chronic alcohol consumption, for example, has been linked to higher rates of depression, cognitive impairment, and suicidal ideation [11]. Research indicates that alcohol usage is linked to attempted suicide, while tobacco use is linked to mental illness. In certain instances, alcohol use has also been linked to a decrease in the number of attempted suicides. Additionally, there is a strong correlation-which varies by age group and state-between drug use and markers of mental illness [12].
This study examines disparities in mental health and substance use across U.S. states by analyzing how economic and behavioral factors influence these outcomes. It focuses on the prevalence of Any Mental Illness (AMI), Serious Mental Illness (SMI), Attempted Suicide (AS), substance use (tobacco, alcohol, and illicit drugs), and treatment access includes RSUT (received substance use treatment), NRSUT (needed but did not receive substance use treatment), and RMHT (received mental health treatment). These measures are compared across higher- and lower-income states and between two age groups: 18-25 and 26 or older, to assess differences, particularly between age groups.
Ultimately, the study seeks to contribute to the broader understanding of mental health disparities across the United States, with the goal of informing actionable strategies to improve mental health equity-particularly for vulnerable populations in economically disadvantaged states. The analysis draws on data from the 2021-2022 National Survey on Drug Use and Health (NSDUH) and the U.S. Census Bureau’s 2022 American Community Survey (ACS) [13,14]. The study focuses on the top 10 states with the highest median household income and the bottom 10 with the lowest, using these as proxies for economic comparison. Data are analyzed using Chi-Square tests to compare the distribution of mental health conditions, substance use, and treatment access across state income levels and age groups. Two proportion Z-tests are then used to assess differences in prevalence rates between age groups.
The organization of the paper is as follows: Section 2 presents the data source and descriptive analysis. The methodology and results are discussed in section 3. Section 4 offers conclusions, limitations and directions for future research.
Data Source and Descriptive Analysis
Data sources
This study relies on two primary datasets:
The 2021-2022 National Survey on Drug Use and Health (NSDUH) provided the data used in this investigation. The analysis covers 35 measures across different age groups: 12 or older, 12 to 17, 18 or older, 18 to 25, 26 or older, and 12 to 20 for specific alcohol measures. Here, we only use age groups 18-25 and 26 or older. Median household. Income was obtained from the American Community Survey (ACS) 1-Year Supplemental Estimates for 2022. The states were divided into two groups based on median income: the top 10 states with the highest median income (higher-income states) and the bottom 10 states with the lowest median income (lower-income states).
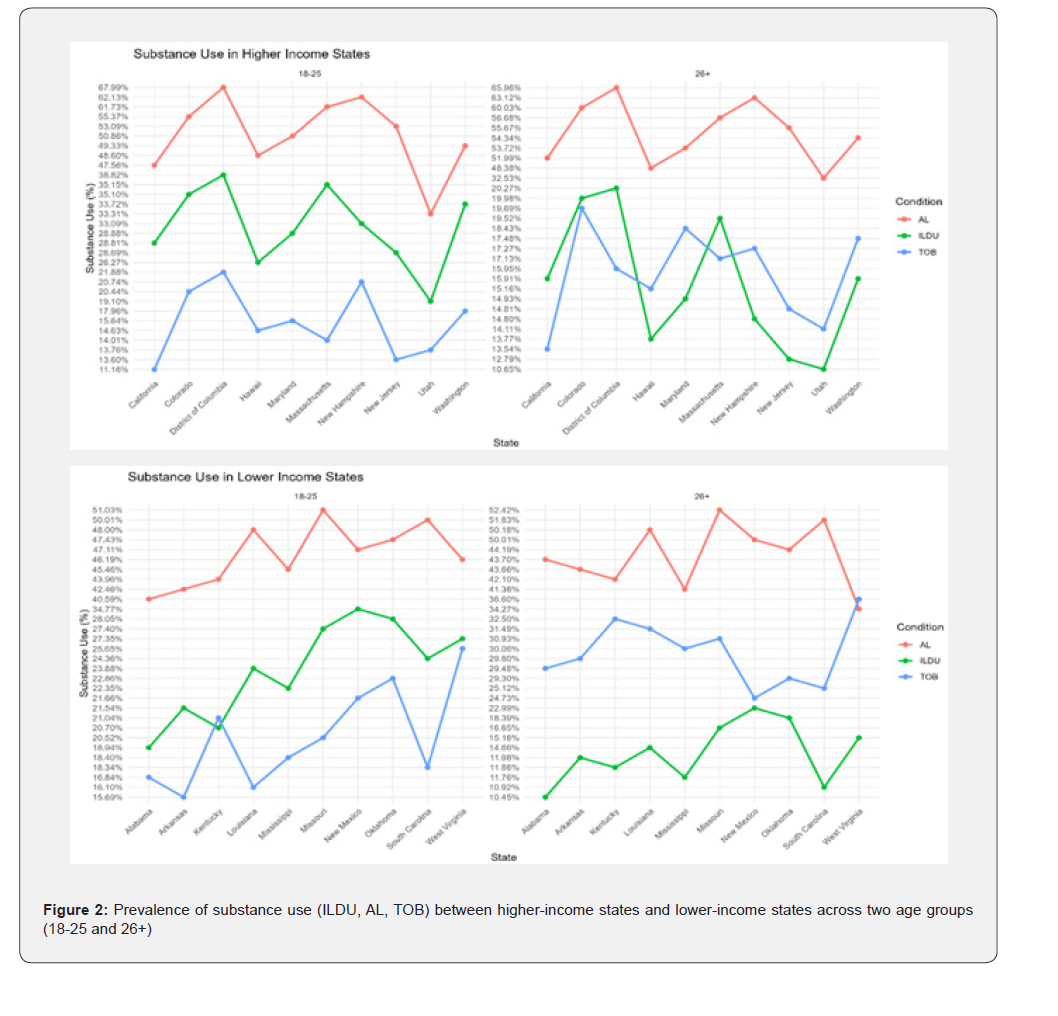
The following (Table 1) presents a comparison of median household incomes between the top 10 higher-income states and the bottom 10 lower-income states in the U.S., based on the 2022 American Community Survey. This categorization provides the basis for examining how socioeconomic conditions may relate to differences in mental health and substance use across states.
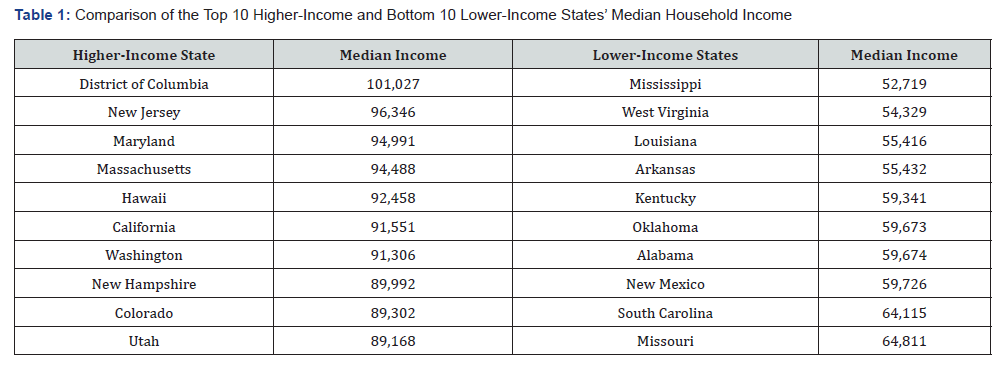
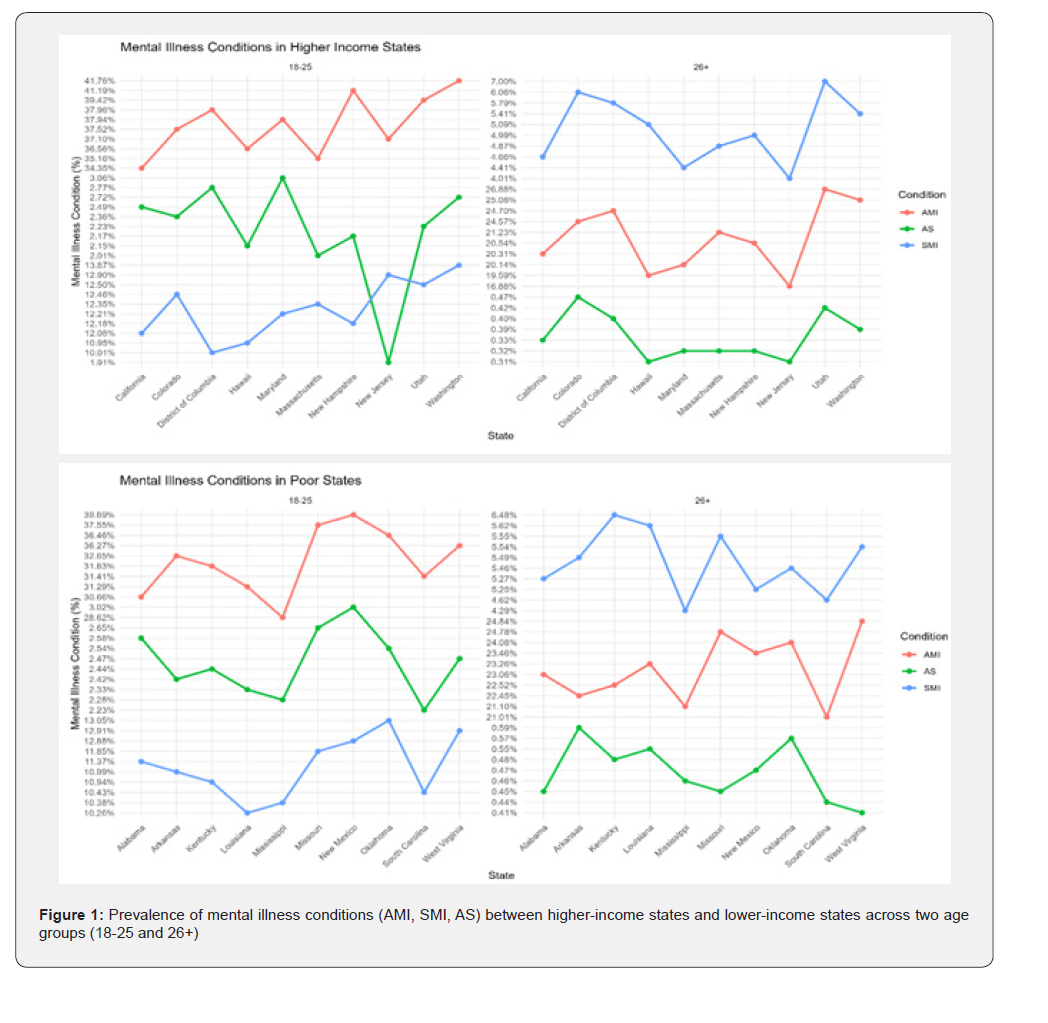
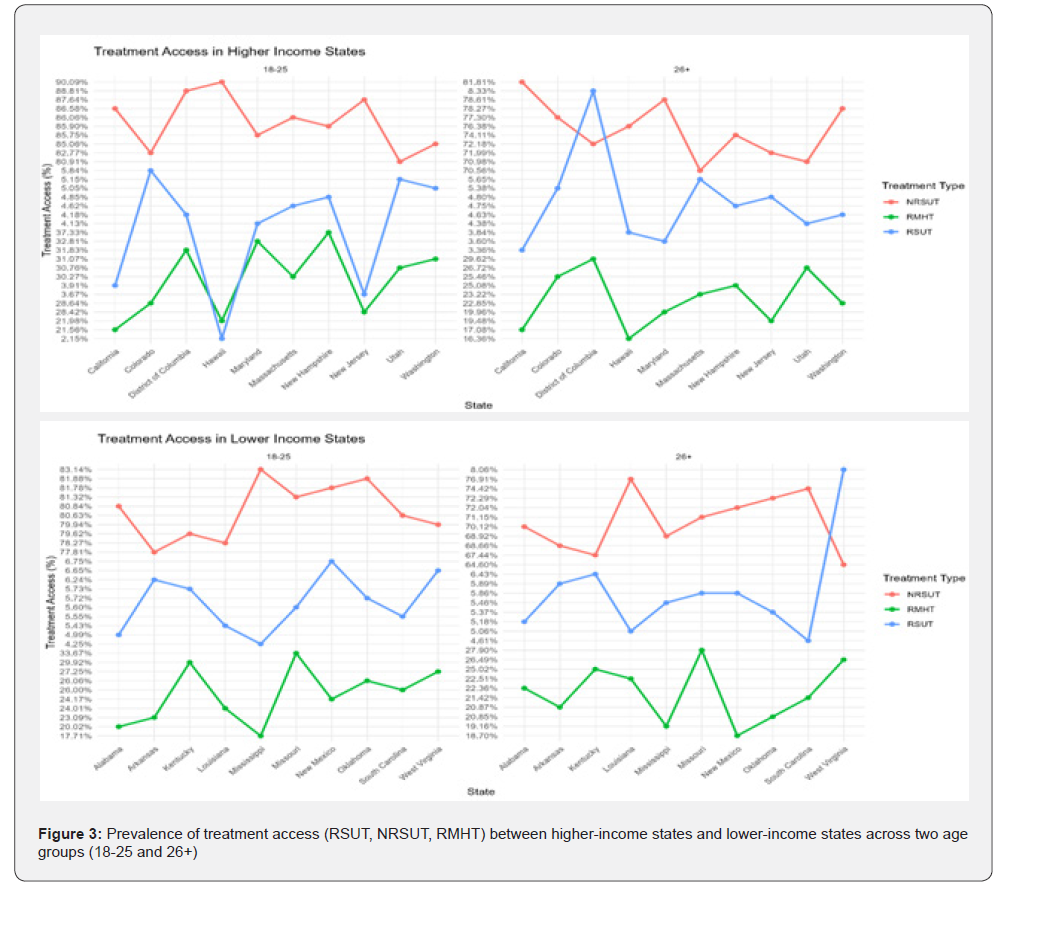
To visualize the disparities in behavioral health outcomes and treatment access, Figures 1 through 3 present comparisons between higher- and lower-income states across two age groups: 18-25 and 26 years or older. These figures illustrate differences in the prevalence of mental health conditions, substance use behaviors, and access to treatment services, highlighting how age and socioeconomic context influence public health indicators.
Figure 1 shows that, across both higher- and lower-income states, Any Mental Illness (AMI) and Attempted Suicide (AS) are more prevalent in the 18-25 age group, while Serious Mental Illness (SMI) is more prevalent in the 26+ age group.
As shown in Figure 2, tobacco use (TOB) is higher in the 18-25 age group within higher-income states, while illicit drug use (ILDU) is higher in the 18-25 age group within lower-income states.
Figure 3 shows the prevalence of Received Substance Use Treatment (RSUT) is more prevalent in the 26+ age group within higher-income states.
The following Table 2 presents summary statistics for mental health conditions, substance use, and treatment access variables in higher-income states, broken down by age group (18-25 and 26+). The data indicate a general trend of increased alcohol and tobacco use with age, while a notable proportion of individuals, particularly those in the younger 18-25 age group, are not receiving substance use treatment.
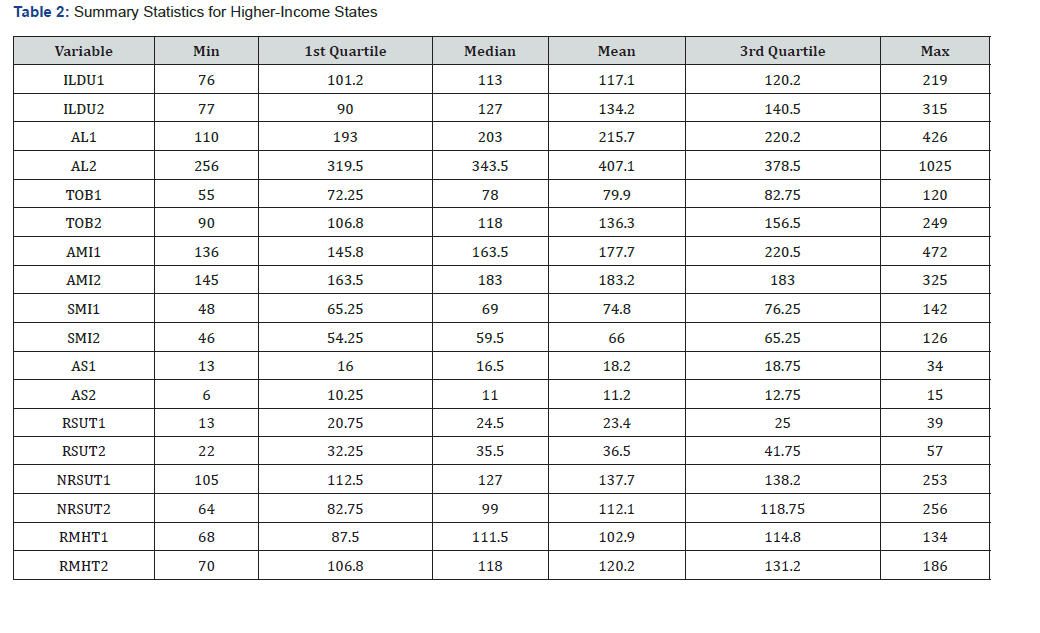
Notes: ILDU1 (Illicit Drug Use 18-25), ILDU2 (Illicit Drug Use 26+), AL1 (Alcohol Use 18-25), AL2(Alcohol Use 26+), TOB1 (Tobacco Use18-25), TOB2 (Tobacco Use 26+), AMI1 (Any Mental Illness 18-25), AMI2 (Any Mental Illness 26+), SMI1 (Serious Mental Illness 18-25), SMI2 (Serious Mental Illness 26+), AS1 (Attempted Suicide 18-25), AS2 (Attempted Suicide 26+), RSUT1 (Received Substance Use Treatment 18-25), RSUT2 (Received Substance Use Treatment 26+), NRSUT1 (Not Received Substance Use Treatment 18-25), NRSUT2 (Not Received Substance Use Treatment 26+), RMHT1 (Received Mental Health Treatment18-25), and RMHT2 (Received Mental Health Treatment 26+).
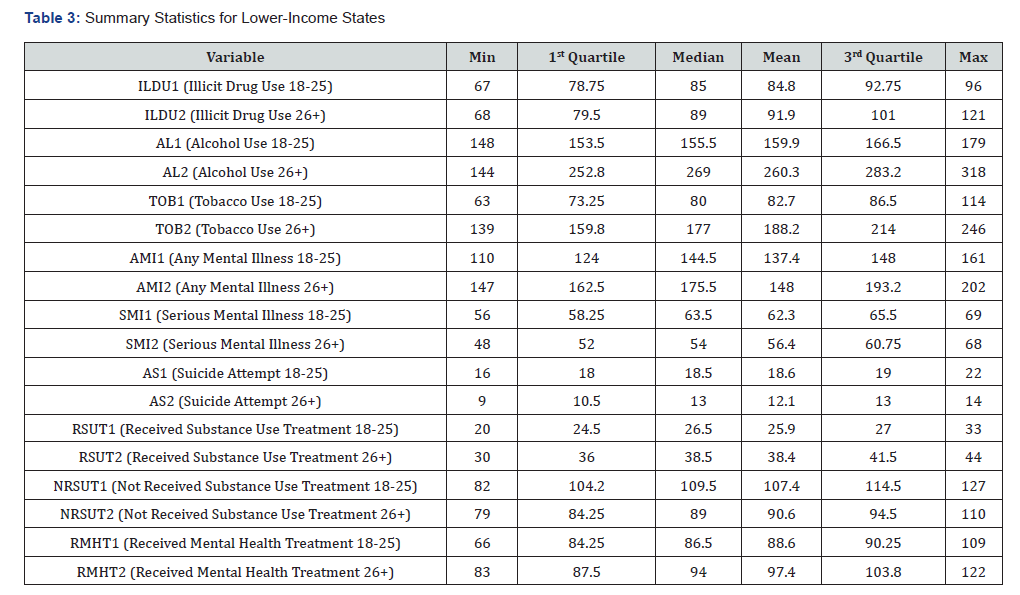
The following Table 3 presents summary statistics for mental health conditions, substance use, and treatment access variables in lower-income states, broken down by age group (18-25 and 26+). The data indicates that substance use and mental health conditions are prevalent across both age groups. Specifically, alcohol and tobacco use generally increase with age, while illicit drug use and suicide attempts are higher for the 18-25 age group.
Determination of sample size
The initial data was presented as percentages with confidence intervals. Since chi-squared tests require count data, we had to transform the data appropriately. Given that we had the confidence intervals for the data, this was easily done by getting the sample size from the margin of error of the confidence interval and then converting the percentages to counts. The specific steps are as follows:
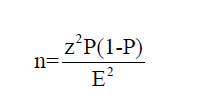
To determine the sample size from a given 95% confidence interval (CI) for a proportion (percentage data), we used the formula for the margin of error (E) in a confidence interval for a proportion:
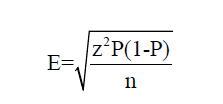
where E is the margin of error, Z is the Z-value corresponding to the desired confidence level (for 95%, Z≈1.96), p is the sample proportion (expressed as a decimal), and n is the sample size. Rearranging the formula to solve for n:
Once the sample size was determined, the observed frequencies (counts) were calculated by dividing the percentage by 100 to get the proportion. Then, we multiplied the proportion by the sample size to get the count. This method was used to calculate the observed frequencies for all variables analyzed in this study.
Methodology and Results
Chi-Square Tests Between States and Mental Health, Substance Use, and Treatment Across Age Groups (18-25 and 26+)
This section investigates whether key behavioral health outcomes differ significantly between higher-income and lower-income states. Specifically, we aim to determine if state-level economic status is associated with variations in mental health conditions, substance use behaviors, and access to treatment, and whether these associations differ by age group (18-25 vs. 26+). Understanding these relationships will help clarify how socioeconomic factors at the state level contribute to disparities in behavioral health and treatment utilization across different populations.
To assess these associations, Chi-square tests of independence were conducted for each outcome category: mental health conditions (Any Mental Illness [AMI], Serious Mental Illness [SMI], Attempted Suicide [AS]), substance use behaviors (Illicit Drug Use [ILDU], Tobacco Use [TOB], Alcohol Use [AL]), and access to treatment (Received Substance Use Treatment [RSUT], Not Received Substance Use Treatment [NRSUT], Received Mental Health Treatment [RMHT]). The analysis was performed separately for two age groups: 18-25 and 26 years or older.
Using RStudio, we applied Chi-square tests to the data, and (Table 4) summarizes the tested hypotheses along with test statistics, degrees of freedom, p-values, and significance at the 0.05 level.
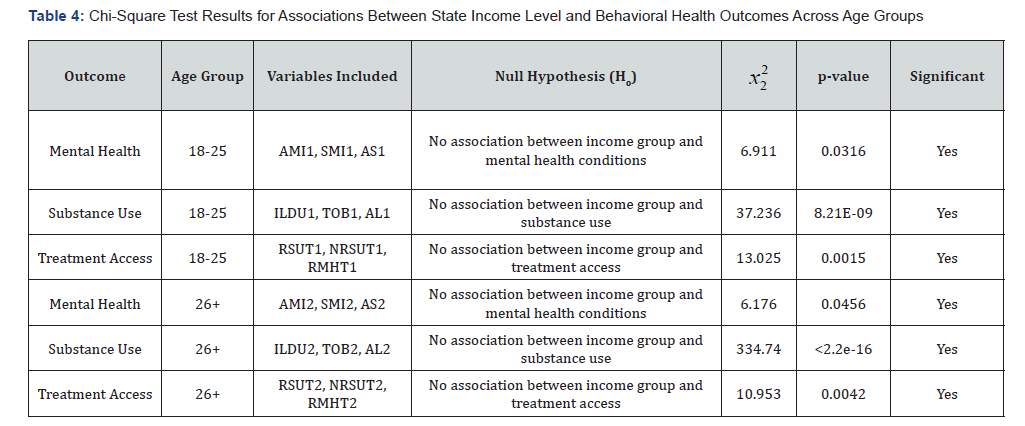
From Table 4, the Chi-square test results revealed statistically significant associations between state income levels and all behavioral health outcomes across both age groups. Among individuals aged 18-25, state-level income was significantly related to the prevalence of mental health conditions, substance use, and access to treatment (all p<0.05). Similar patterns were observed in the 26+ age group, with especially strong associations for substance use outcomes (χ²=334.74, p<2.2e-16). These results indicate that economic conditions at the state level are meaningfully linked to differences in mental health, substance use behaviors, and access to treatment across age groups.
Two-Proportion Z-Test: Comparing Mental Health, Substance Use, and Treatment Across Higher Income and Lower Income States
To evaluate whether behavioral health outcomes differ significantly between higher-income and lower-income states, we conducted two-proportion Z-tests. These tests compared the proportions of mental health conditions, substance use behaviors, and treatment access indicators across two age groups: 18-25 and 26 years or older. The null hypothesis assumed no difference in proportions between the two state income groups, while the alternative hypothesis posited a significant difference.
The analysis was performed using RStudio, with results summarized in (Table 5). For each variable, the test statistic, p-value, confidence interval, and group proportions are reported alongside interpretations of statistical significance.
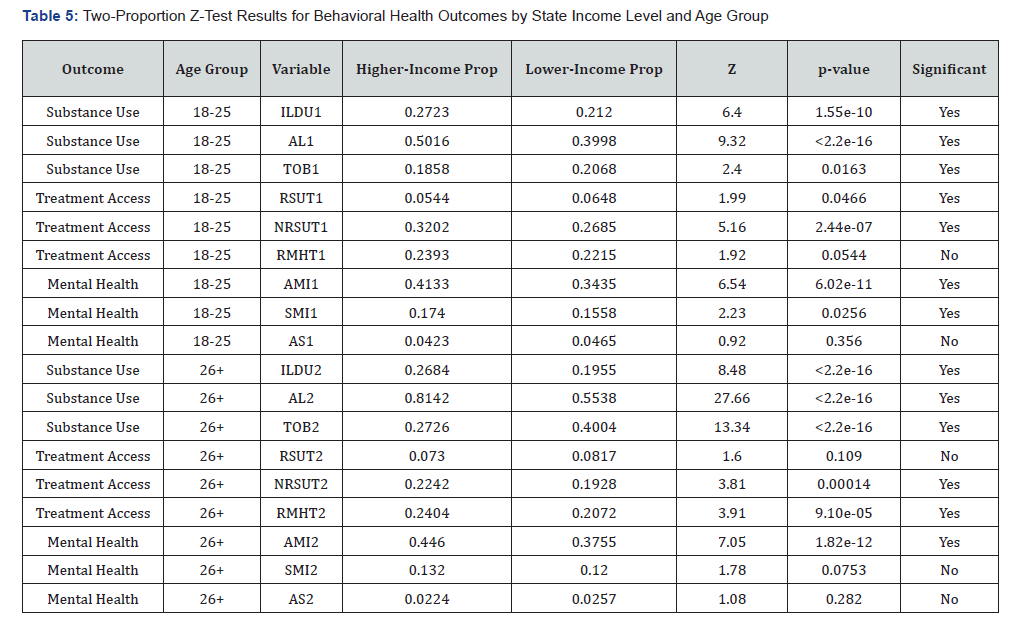
The two-proportion Z-tests reveal that higher-income states exhibit significantly greater proportions of any mental illness and serious mental illness across both age groups, indicating potential differences in diagnosis, reporting, or access to mental health services. Alcohol and illicit drug use rates are also significantly higher in higher-income states for both age groups, while tobacco use is consistently more prevalent in lower-income states, likely reflecting socioeconomic and cultural factors. Treatment access results indicate that higher-income states report greater mental health treatment utilization and higher unmet needs for substance use treatment. However, substance use treatment receipt was lower among young adults (18-25) in higher-income states, suggesting specific barriers within this subgroup. Attempted suicide rates did not differ significantly between the two state groups in either age cohort.
Chi-Square Tests Between Age Groups (18-25 and 26+) and Mental Health, Substance Use, and Access to Treatment
To assess whether age group (18-25 vs. 26 or older) is significantly associated with key behavioral health outcomes, Chi-square tests of independence were conducted. These outcomes included mental health conditions, substance use behaviors and access to treatment. This analysis aimed to determine whether behavioral health outcomes differ by age, shedding light on age-related disparities in mental health burden, substance use patterns, and treatment access.
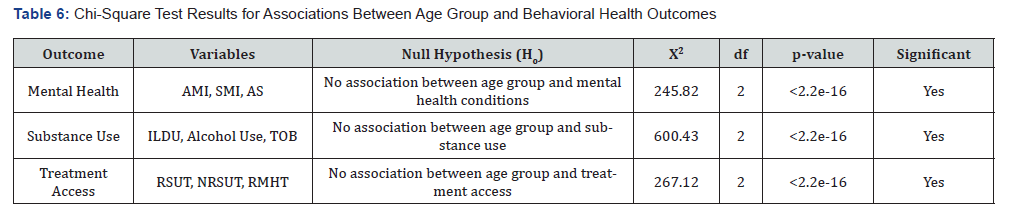
Using RStudio (R software), we applied Chi-square tests of independence to the data for each outcome category. Table 6. summarizes the results, including the hypotheses, test statistics, degrees of freedom, p-values, and whether the associations were statistically significant at the 0.05 level.
The Chi-square test results indicate statistically significant differences in mental health, substance use, and treatment access between the two age groups. Individuals aged 18-25 reported higher rates of any mental illness (AMI), serious mental illness (SMI), and attempted suicide (AS) compared to the 26+ age group. Younger adults (18-25) had higher prevalence of illicit drug use (ILDU), while alcohol and tobacco use were more common among adults aged 26 and older. Older individuals (26+) were more likely to have received substance use treatment (RSUT), while younger individuals (18-25) reported higher rates of unmet treatment needs (NRSUT) and mental health service use (RMHT).
These findings highlight significant behavioral health disparities between younger and older adults, suggesting that targeted interventions may be needed to address the unique needs of each age group.
Two-Proportion Z-Test: Comparing Mental Health, Substance Use, and Treatment Across Age Groups (18-25 and 26+)
To examine whether behavioral health outcomes differ significantly between two age groups 18-25 (younger) and 26+ (older) two-proportion Z-tests were conducted. These tests compared proportions of mental health conditions, substance use behaviors, and treatment access indicators. The null hypothesis stated no significant difference in proportions between the two age groups, while the alternative hypothesis proposed a significant difference. The analysis was performed using RStudio.
Table 7 summarizes the test statistics, p-values, confidence intervals, and group proportions, alongside interpretations of statistical significance.
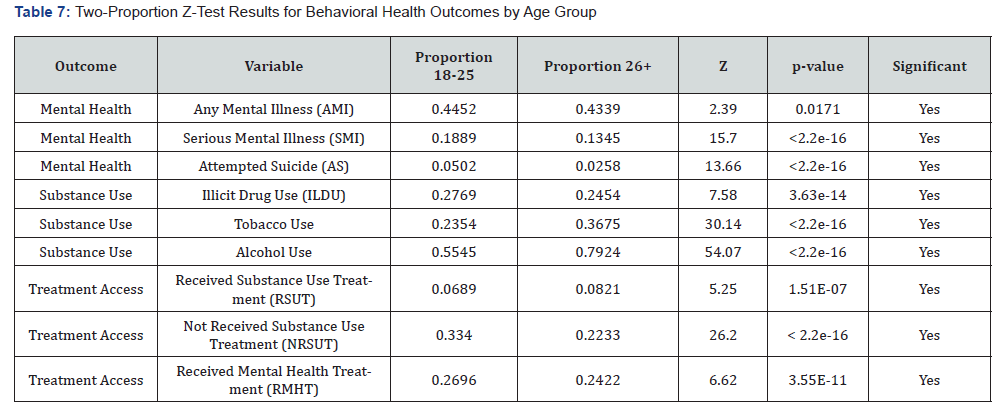
The two-proportion Z-tests demonstrate statistically significant differences across age groups in mental health conditions, substance use behaviors, and treatment access. Younger adults (18-25) tend to have higher rates of mental health challenges and illicit drug use, with a greater unmet need for substance use treatment. Older adults (26+) report higher rates of alcohol and tobacco use and higher receipt of substance use treatment. These findings emphasize the importance of age-specific behavioral health interventions and the need to improve treatment access tailored to the unique needs of younger and older populations.
Conclusions, limitations and Future Directions
Conclusion
This study identified significant disparities in mental health, substance use, and treatment access across U.S. states based on income levels and age groups. Individuals in higher-income states reported higher rates of mental illness, alcohol use, and illicit drug use, along with greater access to mental health treatment but also greater unmet need for substance use treatment. In contrast, tobacco use was more prevalent in lower-income states.
Age-related differences were also notable. Younger individuals (ages 18-25) had higher reported rates of mental illness, serious mental illness, and suicide attempts, while older individuals (26 and above) showed greater prevalence of alcohol and tobacco use. These findings underscore the complex interplay between socioeconomic status, age, and behavioral health outcomes.
To build upon these findings, future research should incorporate a broader range of social determinants, including community engagement, social support networks, access to specialized care, and healthcare provider availability. Including these variables may provide a more comprehensive picture of the factors influencing behavioral health.
Longitudinal studies are also essential to better understand causal pathways and evaluate how socioeconomic and behavioral factors influence mental health outcomes over time. Additionally, exploring differences between rural and urban populations, as well as regional variations, can help refine strategies for targeted interventions. Future research should also examine how political and cultural contexts shape mental health policies and service delivery across states.
Limitations
This study presents several limitations that should be acknowledged. First, the use of data from multiple sources introduces potential inconsistencies in methodology, definitions, and measurement standards. The integration of two different datasets also made data processing less efficient and more complex. Additionally, the broad categorization of variables such as condensing age into just two groups may oversimplify nuanced patterns and obscure critical subgroup variations.
The reliance on a one-year snapshot of median household income limits the ability to evaluate long-term socioeconomic effects or establish temporal sequences. Due to incomplete data, individuals under the age of 17 had to be excluded, which narrows the generalizability of findings. Moreover, the use of model-based estimates inherently carries statistical uncertainty, and the study did not fully account for potential confounding variables, including state-level policies, cultural differences, and healthcare infrastructure. Finally, because this was not an experimental, observational, or clinical trial, the analysis cannot establish direct cause-and-effect relationships. The findings should be interpreted as associations rather than definitive causal links.
Future Directions
This study offers valuable insights into how economic conditions, treatment access, and substance use patterns influence mental health across different populations in the United States. The results emphasize the urgent need for integrated strategies that address economic disparities, expand access to behavioral health services, and implement age-specific and regionally sensitive interventions. These findings lay the groundwork for future research and inform policy efforts aimed at improving public health outcomes across diverse demographic and socioeconomic groups.
References
- Clinton B (1999) Remarks by the President at White House Conference on Mental Health. The American Presidency Project.
- Close G (2015) Glenn Close: The stigma of mental illness. TIME.
- National Institute of Mental Health (2023) Mental illness.
- World Health Organization. Health and well-being.
- McLaughlin KA, Costello EJ, Leblanc W, Sampson NA, Kessler RC (2012) Socioeconomic status and adolescent mental disorders. American Journal of Public Health 102(9): 1742-1750.
- Sareen J, Afifi TO, McMillan KA, Asmundson GJG (2011) Relationship between household income and mental disorders: Findings from a population-based longitudinal study. Archives of General Psychiatry 68(4): 419-427.
- American Psychological Association (2023) Stress in America™ 2023: A Work in America™ survey Workplaces as engines of psychological health & well-being.
- Lee SY, Park CL (2021) Performance pressure and mental health problems among finance workers: A cross-sectional study. International Journal of Environmental Research and Public Health 18(17).
- World Health Organization (2022) Mental health and work: Impact, issues and good practices.
- Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, et al. (2010) Mental disorders as risk factors for substance use, abuse and dependence: Results from the 10-year follow-up of the National Comorbidity Survey. Addiction 105(6): 1117-1128.
- Boden J M, Fergusson DM (2011) Alcohol and depression. Addiction 106(5): 906-914.
- Castillo G, Gulati S, Kibria BMG (2023) Analysis of mental health and drug use in the top 21 most populated U.S. states. Journal of Biostatistics and Epidemiology 9(3): 351-362.
- Gloria Guzman, Melissa Kollar (2023) United States Census Bureau Income in the United States: 2022.
- Substance Abuse and Mental Health Services Administration (2023) 2021-2022 National Survey on Drug Use and Health: Estimated totals by state.