Anesthetic Management for an Anterior Mediastinal Teratoma Resection
Rivas-Velasquez M*, Deras B and Hernández M
Holistic Center, 13 Haupt St., Abtwil 9030, Switzerland
Submission: June 26, 2024; Published: July 01, 2024
*Corresponding author: Rivas-Velasquez M, Hospital Nacional Rosales, El Salvador – Universidad de El Salvador
How to cite this article: Rivas-Velasquez M, Deras B and Hernández M. Anesthetic Management for an Anterior Mediastinal Teratoma Resection. Ann Rev Resear. 2024; 11(3): 555812. DOI: 10.19080/ARR.2024.11.555812
Keywords: Anesthetic management; Mediastinal Teratoma; Double-lumen intubation; epidural analgesia; Chest surgery
Introduction
Teratomas can appear in the ovaries, testicles, retroperitoneum, sacrococcygeal region, and mediastinum, embryologically originates from the three germ layers [1]. Mature mediastinal teratomas account for between 1% and 24% of all mediastinal tumors [2,3]. They are more common in young female patients and during puberty [4]. The multidisciplinary approach to this type of tumor represents an Anesthetic challenge, the main factor is the anatomical location, which foresee several catastrophic scenarios such as the compression of the airway (trachea or bronchi), compression of the Venus return system and hemodynamic collapse, including the risk of mediastinal rupture, the skills required for single-lung intubation, and the ventilation physiological changes this entails, and the postoperative pain management [5,6].
Methods:
A 23-year-old woman went to a primary care center with history of two weeks of intermittent diffuse abdominal pain that irradiates to right hemithorax. No nausea, no vomiting no dyspnea, no cough, no wheezing, denied other respiratory symptoms. Physical examination was negative. Analgesics were prescribed and the pain ceased, and she was discharge.
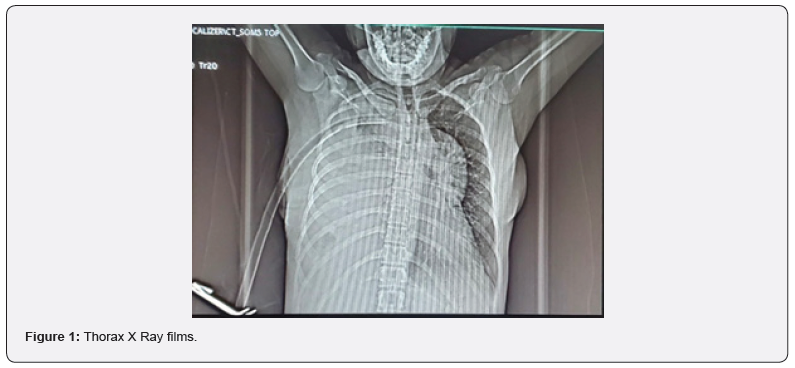
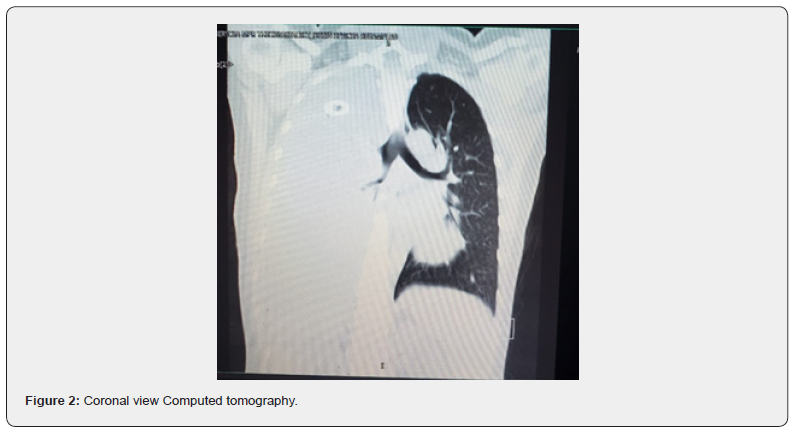
One month later she came to ED in the same health center with the same symptoms, on physical examination there is dullness on percussion on the right hemithorax. The attending physician order an X Ray, and a pleural effusion vs empyema is suspected, a chest tube is placed on the right hemithorax but there is not exudate drain (Figure 1). A CT scan without contrast report liquid density of 100% of right hemithorax UH between 2-38 multiples loculations and septum that produced atelectasis and displaced mediastinal structures. It was not possible to determine the size of the anterior mediastinal mass (Figure 2).
The patient is referred to our medical center for a consultation with a thoracic surgeon, that found dyspnea, general weakness and malaise. A diagnostic and therapeutic emergency open thoracotomy is indicated.
On the emergency anesthesia evaluation, reviewing the images it was determined that the trachea is displaced at principal bronchi level, and unipulmonar ventilation will be necessary, but there is not a direct compromised of the airway.
The patient is classified as intermediate risk according to the Risk Classification and categories of mediastinal mass patients proposed by Tan and Col. [7]. According to the symptoms and imaging that she presented. At the operation room, it was placed standard monitorization according to the American Society of Anesthesiology.
For postoperative pain management, an epidural catheter was inserted at T4 - T5 with Tuohy # 18 needle with Gutiérrez technique, it was completed without complications, subsequently Double-lumen intubation 35 Fr was performed, with induction with total intravenous anesthesia with target-controlled infusion equipment with Remifentanil and Propofol and neuromuscular relaxation with cisatracurium at 0.2mg/kg until reaching a bispectral (BIS) between 37-40 and an electromyography less than 30, cisatracurium was reinforced at 30mcg/kg every 25 to 30 minutes and doses of Propofol and remifentanil were adjusted to maintain index (BIS) between 30 and 60.
During the operation, certain significant changes in blood pressure occurred (systolic blood pressure less than 90 mmHG), a blood loss of between 1000 and 1500 ml was estimated. Crystalloid (1000 ml), ephedrine (20 mg) and 2 units of packed red blood cells were transfused.
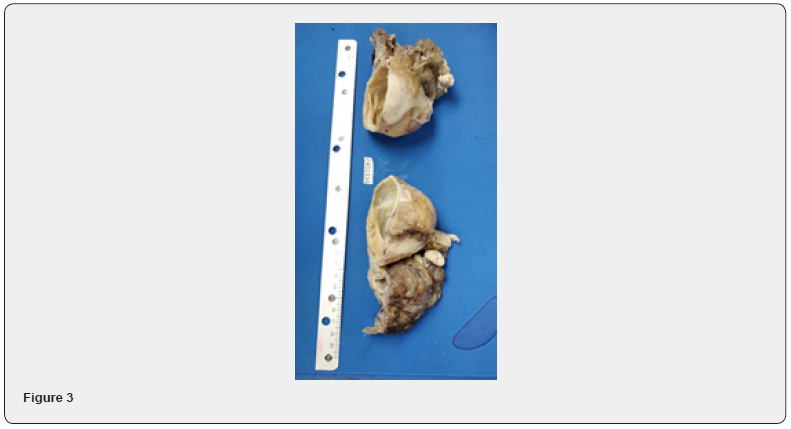
Intravenous analgesia was administered with Morphine 10 mg, Ketorolac 60 mg and Paracetamol 1 g. In the postoperative period, elective extubation was performed without presenting a decrease in pulse oximetry or hypercapnia. Supplementary oxygen was administered with a nasal cannula at 2 liters/ min. She was transferred to the intensive care unit with reinforcement of thoracic epidural anesthesia with 0.125% bupivacaine and 100 mcg fentanyl with a volume of 250 ml at an infusion rate of 6 ml/hr, the same dose was administered for 24 hours and overlapped analgesia. intravenous and then oral, he was discharged on the fourth day postoperatively. The pathologist’s report was mature teratoma (Figure 3).
Conclusions
Chest surgery ranks as one of the most painful surgical procedures; pain after these procedures can be debilitating for the patient, leading to worse outcomes and significant pulmonary complications such as atelectasis and pneumonia [8]. In a systematic review and meta-analysis Balzani and colleagues publishing than there is no consensus on which block is the most effective, the extent of the effect has a medium-large value for each of the blocks realized for thoracic analgesia [9]. Thoracic epidural anesthesia has been shown to be one of the potent measures to attenuate surgical stress and postoperative pain by reducing systemic inflammatory responses during major surgery. In a randomized clinical trial of 60 patients, Okuda et al proposed that thoracic epidural anesthesia under general anesthesia in thoracic surgery could attenuate the inflammatory response associated with pain [10]. A multimodal pharmacologic approach combined with regional anesthesia optimizes analgesia is recommended, the decision regarding which nerve block is most appropriate for the patient depends on the patient’s medical history and comorbidities, and the physician’s expertise [11].
References
- Aguilar-AK, Salazar-HI, Ferreyro-EK, Monterrubio-AKP, Flores-CO, et al. (2024) Mediastinal teratoma: A case report. Cir Card Mex 8(2): 48-50.
- Ota E, Kudo Y, Maehara S, Furumoto H, Matsubayashi J, et al. (2021) Ruptured mediastinal mature teratoma causing severe mediastinitis: report of a surgically resected case and a literature review. Surg Case Rep 7(1): 48.
- Pham LH, Trinh DK, Nguyen AV, Nguyen LS, Le DT, et al. (2024) Thoracoscopic surgery approach to mediastinal mature teratomas: a single-center experience. J Cardiothorac Surg 15(1): 35.
- Zm EZ, Jy R (2024) Mediastinal Germ Cell Tumors: A Review and Update on Pathologic, Clinical, and Molecular Features. Adv Anat Pathol28(5): 335-350.
- Azevedo ASN de, Leal ALB, Ferrari DR, Ferreira LF, Pasolini KR (2024) Anestesia em paciente portador de Volumoso Teratoma Mediastinal: relato de caso. Brazil J Health Rev 7(1): 1741-1753.
- Leivaditis V, Pavlakou A, Grapatsas K, Mulita F, Koletsis E, et al. (2024) Challenges and pitfalls in the perioperative management of mediastinal mass syndrome: an up-to-date review. Kardiochirurgia i Torakochirurgia 21(1): 47-54.
- Tan JC, Lin PS, He LX, Lin Y, Yao YT (2022) Anesthetic management of patients undergoing mediastinal mass operation. Front Surg 9: 1033349.
- Jie-Chao T, Pei-Shuang L, Li-Xian H, Yong L, Yun-Tai Y, et al. (2022) Anesthetic management of patients undergoing mediastinal mass operation. Front Surg 9: 1033349.
- Eleonora B, Giulio Luca R, Edoardo C, Paraskevas L, Claudia F, et al. (2023) The effect of peripheral regional analgesia in thoracic surgery: a systematic review and a meta-analysis of randomized-controlled trials. Tumori 109(1): 6-18.
- Okuda J, Suzuki T, Wakaizumi K, Kato J, Yamada T, et al. (2022) Effects of Thoracic Epidural Anesthesia on Systemic and Local Inflammatory Responses in Patients Undergoing Lung Cancer Surgery: A Randomized Controlled Trial. J Cardiothorac Vasc Anesth 36(5): 1380-1386.
- Marshall K, McLaughlin K (2020) Pain Management in Thoracic Surgery. Thorac Surg Clin 30(3): 339-346.






























