Alcohol Withdrawal Syndrome: A Guide to Diagnostic Approach and Inpatient Management
Sofia Flores1, Kevin Acevedo-Gomez2, Juan Ramon Ventura2, Bivek Khadka3, Sandhya Sharma4, Dilmareth Natera5, Edith Lissette Henriquez Romero2, Marcellina Nwosu6, María Isabel Murillo Pineda7, Alejandra María Aleman Reyes7, Felix Ricardo Bonilla Bonilla2, Rodrigo Antonio Bonilla Figueroa2, Jhon Navarro Gonzalez8, Estefany Díaz de Argueta2, and Maria Isabel Gomez9*
1Department of Psychiatry, University of Medicine and Health Sciences, Saint Kitts, USA
2University of El Salvador, El Salvador, USA
3Chitwan Medical College, Nepal
4College of Medical Sciences, Nepal
5Department of Neurosurgery, University of Minnesota, USA
6American University of Integrative Science School of Medicine and El Paso Pain Center, USA
7Catholic University of Honduras, Honduras, USA
8University of Zulia, Venezuela, USA
9Universidad del Valle, México
Submission: August 23, 2023; Published: September 01, 2023
*Corresponding author: Maria Isabel Gomez, Department of Psychiatry, University of Medicine and Health Sciences, Saint Kitts, USA. Email id: mariaisagcoral@gmail.com
How to cite this article: Sofia F, Kevin Acevedo-G, Juan Ramon V, Bivek K, Sandhya S, et al. Alcohol Withdrawal Syndrome: A Guide to Diagnostic Approach and Inpatient Management. Ann Rev Resear. 2023; 9(5): 555775. DOI: 10.19080/ARR.2023.09.555775
Abstract
Alcohol withdrawal syndrome (AWS) is a complex medical condition that arises from abrupt cessation of alcohol consumption in individuals with alcohol use disorder. It presents with a wide range of symptoms, varying from mild anxiety and tremors to severe manifestations such as hallucinations and delirium tremens. This review article aims to provide a comprehensive overview of AWS, covering its epidemiology, pathophysiology, clinical presentation, diagnosis, and treatment strategies. The prevalence of AWS is significant, highlighting the need for appropriate recognition and management. Chronic alcohol use leads to neuroadaptation and neurotransmitter imbalances, resulting in hyperexcitability upon alcohol cessation. A clinical assessment, supported by tools like the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) scale, assists in diagnosis. Management of AWS involves a multifaceted approach, including supportive care, pharmacotherapy, and monitoring. Benzodiazepines are the first-line treatment, but other agents like anticonvulsants, alpha-2 receptor agonists, propofol, and carbamazepine offer alternatives for refractory cases. Supportive care addresses electrolyte imbalances and complications, while outpatient treatment is effective for mild to moderate AWS cases, with Enhanced Telephone Monitoring (ETM) as a valuable follow-up strategy. In conclusion, understanding AWS’s complexities, early diagnosis, and tailored treatment plans are crucial for improving patient care and long-term abstinence outcomes. This review synthesizes existing knowledge, highlights gaps, and suggests future research directions to enhance clinical practices and patient outcomes in AWS management.
Keywords: Alcohol Withdrawal Syndrome; Alcohol Use Disorder; Benzodiazepines; Anticonvulsants; Clinical Institute Withdrawal Assessment for Alcohol Revised; Ciwa-Ar; Neuroadaptation; Neurotransmitter Imbalance
Abbreviations: AWS: Alcohol Withdrawal Syndrome; AUD: Alcohol Use Disorder; CNS: Central Nervous System; GABA: Gamma-Aminobutyric Acid; NMDA: N-Methyl-D-Aspartate; CIWA-Ar: Clinical Institute Withdrawal Assessment for Alcohol Revised; DT: Delirium Tremens; DSM-5: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; ED: Emergency Department; AH: Alcohol-Associated Hepatitis; ICU: Intensive Care Unit; BZDs: Benzodiazepines; FDA: Food and Drug Administration; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; ETM: Enhanced Telephone Monitoring.
Introduction
Alcohol abuse disorder is characterized by excessive alcohol consumption that negatively affects an individual’s physical health, social relationships, and overall well-being. Alcohol withdrawal syndrome (AWS) is a potentially severe condition that occurs when individuals who are physically dependent on alcohol suddenly stop or reduce their alcohol intake [1]. AWS manifests as a range of autonomic and psychomotor symptoms, including anxiety, tremors, sweating, hallucinations, seizures, and delirium tremens in severe cases. Epidemiological studies have reported varying prevalence rates, highlighting the complexity of the condition’s assessment and diagnosis. AWS remains a significant medical challenge, necessitating appropriate recognition and management strategies. The etiology and pathogenesis are multifaceted. Chronic alcohol use leads to neuroadaptation, wherein the central nervous system adjusts to alcohol. Abrupt cessation disrupts this balance, triggering hyperexcitability and withdrawal symptoms. GABAergic neurotransmission alterations, glutamate rebound, and neuroinflammatory responses contribute to the clinical manifestations of AWS [1,2]. Clinical presentation of AWS varies widely, with mild cases characterized by anxiety, restlessness, and mild tremors, while severe instances can lead to hallucinations, seizures, and delirium tremens. Diagnosis is primarily clinical, relying on identifying characteristic symptoms in individuals with a history of heavy alcohol use. Clinical assessment tools, such as the Clinical Institute Withdrawal Assessment for Alcohol (CIWAAr), aid in evaluating the severity of AWS and guiding treatment decisions [2].
Treatment options encompass a comprehensive approach to managing withdrawal symptoms, preventing complications, and supporting long-term abstinence. Benzodiazepines are commonly used to alleviate anxiety and prevent seizures, while thiamine supplementation helps address potential nutritional deficiencies. Supportive care, monitoring, and addressing coexisting medical conditions are essential for AWS management [3,4]. This narrative review aims to provide a comprehensive overview of alcohol withdrawal syndrome, encompassing its definition, epidemiology, etiology, clinical presentation, diagnosis, and treatment options. By synthesizing existing research and clinical knowledge, this review aims to critically analyze the current literature, identify gaps in knowledge, and provide insights into future research directions.
Epidemiology & Pathophysiology
The importance of promptly identifying and addressing alcohol withdrawal syndrome (AWS), particularly severe forms like delirium tremens, is underscored by its epidemiology and pathophysiology. Effective communication among interprofessional teams is vital for coordinating care and enhancing patient outcomes in AWS cases [5]. Alcohol use disorder (AUD), as described in DSM-IV, is notably prevalent, especially in emergency department (ED) settings. Roughly 40% of ED patients exhibit AUD [5]. In ED patients admitted with trauma and assessed using the revised Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) score, 83% are male, and 43% are over 55. Among trauma patients showing AWS symptoms, more than 52% have a CIWA-Ar score >20, and 24% progress to delirium tremens (DT) [5,6]. AWS is particularly common among individuals hospitalized with alcohol-associated hepatitis (AH), affecting approximately 32% of these patients. Factors such as lower platelet levels, a history of prior AWS, and prophylactic measures are associated with AWS emergence in AH cases. This condition further complicates hospitalization, heightening infection vulnerability and necessitating interventions like mechanical ventilation and ICU admission [7].To comprehensively understand AWS pathophysiology, it’s crucial to begin by grasping the effects of ethanol, the primary alcohol consumed by chronic users. Ethanol acts as a depressant on the central nervous system (CNS). Prolonged exposure to ethanol leads to dependence as it inhibits CNS glutamate receptors (excitatory components) while enhancing gamma-aminobutyric acid (GABA) receptors (inhibitory components). When alcohol intake ceases, the CNS becomes overly stimulated due to removing inhibitory effects, resulting in withdrawal symptoms [5]. Ethanol affects the CNS through mechanisms involving N-methyl-D-aspartate (NMDA) and GABA receptors. Initially, it induces euphoria and behavioral excitation by increasing glutamate binding to NMDA receptors. At higher concentrations, it intensifies GABA effects, causing acute intoxication. Chronic alcohol use leads to tolerance and physical dependence, associated with GABA receptor downregulation and increased NMDA receptor expression [8].
Clinical Presentation
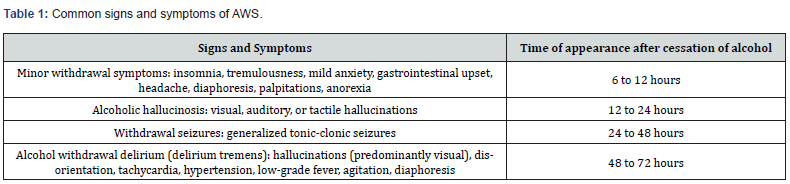
Alcohol withdrawal syndrome (AWS) presents a multifaceted medical challenge when individuals abruptly cease or decrease their prolonged alcohol consumption. This condition exhibits diverse clinical manifestations, with mild symptoms commonly emerging within hours after the last alcoholic drink. Notably, nearly half of individuals with a history of prolonged and heavy drinking may encounter some degree of AWS upon modifying or discontinuing their alcohol intake [9]. Within the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), two of the eleven defining characteristics of alcohol use disorder (AUD) encompass the presence of withdrawal symptoms and the physiological phenomenon known as tolerance [10].The DSM- 5 establishes specific diagnostic criteria for alcohol withdrawal, requiring individuals to have ceased or reduced their heavy and prolonged alcohol use. They should also experience two or more symptoms within hours to days after making these changes. These symptoms include autonomic hyperactivity, such as excessive sweating or a pulse rate exceeding 100 bpm, increased hand tremors, insomnia, nausea or vomiting, transient sensory hallucinations or illusions, psychomotor agitation, anxiety, and generalized tonic-clonic seizures. Importantly, these symptoms should result in significant distress or impairment in critical aspects of an individual’s life, such as social or occupational functioning. Moreover, the diagnostic process should exclude other medical conditions as the cause and rule out alternative mental disorders, including those related to intoxication or withdrawal from other substances [11] (Table 1). Alcohol withdrawal symptoms encompass a spectrum, ranging from mild tremors to the life-threatening condition known as delirium tremens (DT), characterized by convulsions and the potential for fatality if not promptly diagnosed and treated [12]. Delirium, a clinical syndrome, involves disturbances in attention, awareness, and cognition, manifesting as reduced ability to focus or shift attention, disorientation, memory deficits, and altered perceptual abilities. DT represents the most severe manifestation of alcohol withdrawal, marked by an altered state of consciousness, pronounced autonomic dysfunction, and abnormal vital signs. Symptoms include visual hallucinations, tachycardia, hypertension, hyperthermia, agitation, and excessive sweating. This severe condition can persist for up to a week after alcohol cessation and, in some cases, even longer. Alcohol-related hallucinosis is a distinct form of withdrawal-related psychosis that may begin during continued alcohol use or after its cessation [13].
For assessing the severity of alcohol withdrawal symptoms, the widely used Clinical Institute for Withdrawal Assessment for Alcohol Revised Scale (CIWA-Ar) provides a valuable tool. This scale evaluates ten withdrawal symptoms and assists healthcare professionals in tracking symptoms and determining the need for medical intervention. The CIWA-Ar categories, and associated score ranges, encompass various aspects of withdrawal symptoms, such as agitation, anxiety, auditory disturbances, clouding of the sensorium, headache, nausea/vomiting, paroxysmal sweats, tactile disturbances, tremors, and visual disturbances. Scores below 8 to 10 indicate minimal to mild withdrawal, scores between 8 and 15 indicate moderate withdrawal with significant autonomic arousal, and scores of 15 or higher suggest severe withdrawal, potentially leading to impending delirium tremens [14]. However, it’s important to differentiate alcohol withdrawal symptoms from similar manifestations caused by medical or psychiatric conditions and concurrent medications like beta blockers. In such instances, a comprehensive clinical patient assessment is necessary to ensure accurate diagnosis and appropriate management.
Diagnostic Approach
Diagnosing alcohol withdrawal syndrome (AWS) involves a comprehensive approach encompassing history-taking and thorough clinical examination [15]. Pertinent historical information includes details about alcohol intake, duration of use, time since the last drink, prior withdrawal episodes, coexisting medical or psychiatric conditions, and other substance abuse. Withdrawal symptoms usually initiate around 6 hours after alcohol cessation. However, if withdrawal symptoms or delirium onset occurs more than a week after complete alcohol cessation, an AWS diagnosis becomes less tenable, irrespective of alcohol dependence severity [15,16]. Conducting a physical examination and assessing vital signs is crucial, encompassing parameters like blood pressure, heart rate, body temperature, and blood glucose [17]. Additionally, it’s essential to consider potential complicating medical conditions such as arrhythmias, congestive heart failure, gastrointestinal bleeding, infections, liver disease, nervous system impairment, and pancreatitis. Routine laboratory investigations entail complete blood count, liver function tests, urine drug screening, and analysis of blood alcohol and electrolyte levels [18]. In some cases, more extensive testing like lumbar puncture and cranial computed tomography (CT) or magnetic resonance imaging (MRI) might be necessary to confidently exclude alternative diagnostic possibilities, particularly in instances involving altered mental status and fever [15,19].
The diagnosis of AWS remains primarily clinical [19]. According to the DSM-5 criteria, AWS is diagnosed when patients display cessation or reduction of heavy and prolonged alcohol use (Criterion A) and two or more withdrawal symptoms develop within hours to days after this cessation (Criterion B). These symptoms include autonomic hyperactivity, tremors, insomnia, nausea, hallucinations, psychomotor agitation, anxiety, and seizures. The symptoms should cause significant distress or impairment (Criterion C), not be attributable to another condition, or be better explained by another mental disorder or substance withdrawal [16,18]. Blood ethanol measurement in suspected AWS cases should be correlated with the patient’s history, if possible, to assess the last ingestion and metabolic capacity for alcohol [18]. A serum glucose test is indicated, particularly for patients with alcoholrelated liver disease prone to hypoglycemia. Comprehensive metabolic panels help detect acidosis, dehydration, concurrent renal issues, and other abnormalities in chronic alcoholism. The patient’s clinical course determines imaging studies, with chest radiography, head CT, abdominal CT, and spinal MRI being considered based on specific indicators. Electrocardiography and additional tests might be necessary, as well as lumbar puncture and spinal-fluid analysis, to rule out conditions mimicking or coexisting with alcohol withdrawal [6]. Premature diagnosis of AWS can lead to inappropriate use of sedatives, potentially delaying accurate diagnosis [19,18]. The differential diagnosis for AWS involves considering conditions like hyponatremia, hepatic encephalopathy, pneumonia, encephalitis/meningitis, head injury, thyrotoxicosis, lithium intoxication, atropine/tricyclic intoxication, psychosis, antidepressant intoxication, and subacute encephalopathy with seizures in alcohol use disorder [20-23].
Treatment
Benzodiazepines & Anti-convulsants
Patients experiencing moderate to severe alcohol withdrawal syndrome face hyperexcitability characterized by tremors, tachycardia, confusion, and seizures, which are crucial for risk assessment and severity classification [24]. This syndrome arises from the abrupt discontinuation of exogenous alcohol, leading to an imbalance in glutamatergic and GABAergic neurotransmission. This imbalance heightens the risk of withdrawal seizures due to excessive excitatory neurotransmission [25]. In managing alcohol dependence, particularly in the context of withdrawal and relapse prevention, nonbenzodiazepine anticonvulsants play a significant role due to their influence on glutamatergic and GABAergic neurotransmission [26]. Phenytoin, however, has demonstrated ineffectiveness in preventing alcohol withdrawal seizures [27]. Conversely, studies have explored the utility of anticonvulsants like carbamazepine and oxcarbazepine in severe alcohol withdrawal cases. These studies indicated safety with an initial dose of 800 mg/day for carbamazepine and 900 mg/ day for oxcarbazepine, followed by tapering doses over several days. Notably, these anticonvulsants showed promise in reducing withdrawal symptoms, convulsions, and delirium tremens. Gabapentin, examined in moderate to severe withdrawal, displayed symptom reduction based on observer reports, with an initial safe dosage of 600 to 600 mg/day. However, evidence remains limited for Valproic Acid, topiramate, zonisamide, levetiracetam, and pregabalin in managing severe alcohol withdrawal [28]. Incorporating these anticonvulsants into the treatment of alcohol withdrawal syndrome offers a broader therapeutic approach that targets the intricate neurochemical imbalances of alcohol cessation. Alongside supportive care and behavioral interventions, such pharmacological strategies could contribute to improved outcomes in individuals grappling with alcohol dependence.
Supportive Care
General supportive care is essential to treating alcohol withdrawal syndrome, from preventing complications to treating it in a calm environment. Patients feel better in a quiet environment that avoids loud sounds and other strong stimuli, such as excessively bright lights or dark shadows [29]. Initial management includes preventing seizures, avoiding self-injury during agitation, adequate fluid resuscitation, electrolyte replacement, and providing timely antibiotic treatment in case of bronchial aspiration. Initial management for any patient suspected of alcohol withdrawal should begin with adequate fluid resuscitation to restore the water deficit caused by osmotic diuresis and low fluid intake [30]. Although there is no consensus on the amount and speed of fluid replacement, symptom-guided therapy is recommended; this involves restoring fluids based on the clinical evaluation of dehydration to ensure sufficient tissue perfusion. Patients undergoing alcohol withdrawal experience a loss of electrolytes. The most common hydro electrolytic imbalances observed in such patients are hyponatremia, hypokalemia, hypomagnesemia, and hypophosphatemia. Thiamine and magnesium administration have not been shown to have any beneficial effect on AWS symptoms to decrease the incidence of delirium tremens and seizures [31]. However, thiamine deficiency is frequent among patients with AWS, so systematic administration is recommended to prevent the development of Wernicke-Korsakoff encephalopathy due to glucose intake can trigger or worsen this complication, whose mortality reaches 20%. Magnesium sulfate has not been shown to prevent seizures and is only recommended in cases where its deficiency is proven [32,33]. In extreme agitation or aggressiveness, mechanical restraint can be applied briefly [34].
Other Medications/Treatments
Alcohol withdrawal syndrome (AWS) is typically managed with benzodiazepines (BZDs) as the first-line treatment. However, the current literature doesn’t indicate one specific BZD as more efficacious than another, considering differences in pharmacokinetic properties as a guide for selection [35]. In situations where standard sedative therapy using BZDs proves insufficient, additional management strategies become necessary due to the complexities of AWS symptoms. Chronic alcohol withdrawal induces changes in the central nervous system catecholamines. Activation of alpha 2-adrenergic receptors leads to neuron hyperpolarization and the inhibition of neurotransmitter release, explaining the neuroprotective role of alpha 2 adrenergic receptor agonists in AWS management. Among these, three such agents have been studied: lofexidine, clonidine, and dexmedetomidine. Clonidine has demonstrated efficacy in addressing acute withdrawal symptoms that do not respond adequately to conventional sedative therapy, presenting a notable reduction in withdrawal scores, systolic blood pressure, and heart rate. Patients treated with clonidine also experienced decreased anxiety and improved cognitive recovery, thus enhancing the management of symptoms like anxiety, irritability, agitation, and excitement.
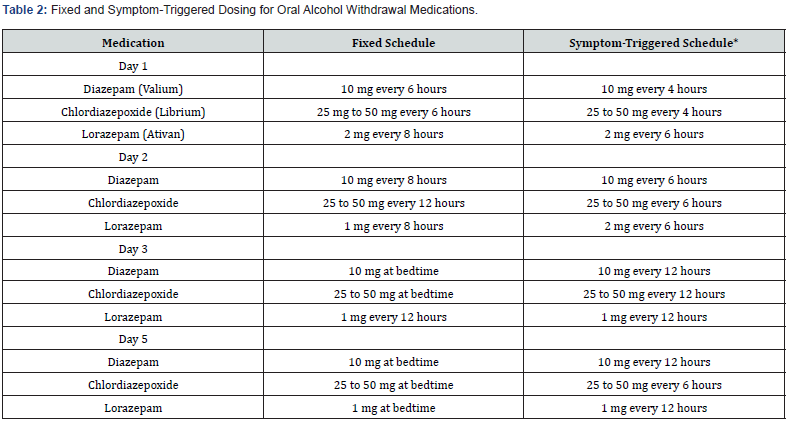
Dexmedetomidine, a selective alpha-2 receptor-targeting medication, provides sedative, analgesic, anxiolytic, and sympatholytic effects, focusing on patient safety regarding respiratory depression. Its alpha-2 receptor specificity is significantly higher than that of clonidine. Recent FDA approval for dexmedetomidine’s use in sedation without intubation provides clinicians with an additional tool for managing alcohol withdrawal in ICU patients [36]. Propofol, an intravenous anesthesia agent, has effectively alleviated AWS symptoms due to its interaction with GABA-mediated receptor function, leading to GABA channel activation and antagonism of excitatory amino acids like NMDA. Its rapid onset and short duration of action make it an appealing option for benzodiazepine-refractory cases [37,38]. Carbamazepine has shown promise in AWS treatment, comparable to oxazepam and lorazepam in managing withdrawal symptoms. Additionally, evidence suggests it may reduce alcohol consumption in alcohol-dependent outpatients post-withdrawal period [39]. Barbiturates, specifically phenobarbital, enhance GABA-A chloride channel opening, leading to potentiated effects. Phenobarbital’s quick onset and prolonged effects have been shown to decrease benzodiazepine use when applied early in AWS treatment. However, the dosing methods for phenobarbital vary, and concerns about respiratory failure have been raised, with lowintermittent dosing being a commonly reported approach [40]. The collective use of these agents provides a multifaceted strategy for addressing the complexities of alcohol withdrawal syndrome, improving patient care and outcomes (Table 2).
Monitoring & Follow-up
Outpatient treatment for mild to moderate alcohol withdrawal syndrome (AWS) is often a safe and effective option that minimizes disruption to work and family life. However, individuals with severe psychiatric issues or medical conditions should be considered for inpatient treatment. Indicators for inpatient detoxification include a history of severe withdrawal symptoms, withdrawal seizures, previous detoxifications, coexisting psychiatric or medical conditions, recent heavy alcohol consumption, pregnancy, and a lack of reliable support [41]. Significant laboratory abnormalities may necessitate inpatient treatment, whereas routine laboratory tests are generally unnecessary for mild AWS [41,42]. In outpatient treatment, patients and their support network should receive clear instructions regarding withdrawal medication administration, potential side effects, expected symptoms, and steps to take if symptoms worsen. At each visit, small amounts of medication, along with thiamine and multivitamins, should be prescribed. Family support can significantly influence outpatient treatment success, although dysfunctional family dynamics or home triggers for alcohol consumption might hinder progress [42]. Monitoring during outpatient treatment should be tailored to symptom severity and patient characteristics. Daily evaluation is joint until symptoms diminish and medication doses can be reduced. Blood pressure and pulse checks are essential, and alcohol breath analysis might be utilized intermittently. The severity of AWS symptoms should be reassessed using the same measurement tool used during the initial assessment. When the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) score falls below a certain threshold, medication dosages can be tapered and eventually discontinued. Symptoms should generally resolve within a week of alcohol abstinence. Patients who don’t respond well to benzodiazepine therapy, miss appointments, or resume drinking should be referred to specialists or inpatient programs [41].
Benzodiazepines can be administered either through fixed or symptom-triggered schedules, with the latter showing potential benefits in motivating patients to alcohol treatment enrollment [43]. Additionally, intravenous fluids, magnesium supplementation, and thiamine administration are essential aspects of AWS treatment to rectify fluid, electrolyte, and dietary imbalances [41]. Follow-up services are crucial to prevent relapses and repeat detoxification, with Enhanced Telephone Monitoring (ETM) as a viable option. ETM involves a combination of in-person appointments and regular phone calls to support patients in continued care and engagement in treatment programs [42,43]. The Clinical Institute Withdrawal Assessment for Alcohol (CIWAAr) scale is a valuable tool for AWS management, helping to assess withdrawal severity, administer benzodiazepines appropriately, and monitor patients for follow-up [44]. Integrating an individualized and comprehensive treatment program alongside AWS management is essential for better outcomes and sustained abstinence [41].
Conclusion
In conclusion, alcohol withdrawal syndrome (AWS) presents a significant medical challenge characterized by a range of symptoms arising from abrupt alcohol cessation. The condition’s prevalence highlights the complexity of assessment and diagnosis, necessitating appropriate recognition and management strategies. AWS arises from chronic alcohol use, leading to neuroadaptation and imbalances in neurotransmission, resulting in hyperexcitability upon cessation. The clinical presentation of AWS is diverse, varying from mild symptoms such as anxiety and tremors to severe manifestations like hallucinations and delirium tremens. Diagnosis relies primarily on clinical assessment, with tools like the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) scale aiding in symptom severity evaluation.
The management of AWS requires a comprehensive approach, including supportive care, pharmacotherapy, and monitoring. Benzodiazepines are the first-line treatment for AWS, but additional agents like anticonvulsants, alpha-2 receptor agonists, propofol, and carbamazepine offer alternative strategies for refractory cases. Supportive care addresses electrolyte imbalances and complications, and monitoring aids in adjusting treatment based on symptom severity. Outpatient treatment is effective for mild to moderate AWS cases, supported by clear instructions, medication administration, and monitoring. Enhanced Telephone Monitoring (ETM) serves as a valuable follow-up strategy. A comprehensive treatment program combined with AWS management is crucial for successful outcomes. In conclusion, understanding AWS’s intricacies, early diagnosis, and tailored treatment plans are crucial in improving patient care and longterm abstinence outcomes. This review provides a comprehensive overview of AWS, synthesizing existing knowledge and paving the way for future research directions and improved clinical practices.
References
- Babel K (1997) Treating acute alcohol withdrawal. Am J Nur’s 97(1): 22-3.
- Badawy AA (1984) Alcohol intoxication and withdrawal. Contempt Issues Clin Biochem 1: 95-116.
- (2003) Alcohol withdrawal. Nur’s Times 99(23):31.
- Satel SL, Kosten TR, Schuck it MA & Fischman MW (1993) Should protracted withdrawal from drugs be included in DSM-IV? Am J Psychiatry 150(5): 695-704.
- Goodson CM, Clark BJ, Douglas IS (2014) Predictors of severe alcohol withdrawal syndrome: a systematic review and meta-analysis. Alcohol Clin Exp Res 38(10): 2664-2677.
- Saltillo K, McGuire E, Mains CW, van Doorn EC, Bar D (2017) Occurrence, Predictors, and Prognosis of Alcohol Withdrawal Syndrome and Delirium Tremens Following Traumatic Injury. Crit Care Med 45(5): 867-874.
- Marti Aguado, Googol A, Gomez Medina, Jamali A, Abo Zed A, et al. (2023) Prevalence and clinical impact of alcohol withdrawal syndrome in alcohol-associated hepatitis and the potential role of prophylaxis: a multinational, retrospective cohort study. eClinicalMedicine 61: 102046.
- Jesse S, Bråthen G, Ferrara M, Keindl M, Ben Menachem E, et al. (2017) Alcohol withdrawal syndrome: mechanisms, manifestations, and management. Acta Neurologica Scandinavica 135(1): 4-16.
- Day E, Daly C (2022) Clinical management of alcohol withdrawal syndrome. Addiction 117(3): 804-814.
- American Psychiatric Association, AP & American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders: DSM-IV Washington DC: American psychiatric association.
- Alcohol Withdrawal Diagnostic Criteria.
- Bayard M, Mcintyre J, Hill KR, Jack Woodside J (2004) Alcohol withdrawal syndrome. American Family Physician 69(6): 1443-1450.
- Jesse S, Bråthen G, Ferrara M, Keindl M, Ben Menachem E, et al (2017) Alcohol withdrawal syndrome: Mechanisms, manifestations, and management. Acta Neurologica Scandinavica 135(1): 4-16.
- Sullivan J T, Sykora K, Schneiderman J, Naranjo CA & Sellers E M (1989) Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA‐Ar) British journal of addiction 84(11): 1353-1357.
- Sachdeva A, Choudhary M, Chandra M (2015) Alcohol Withdrawal Syndrome: Benzodiazepines and Beyond. J Clin Diagn Res 9(9): VE01-VE07.
- Samuel M Tiglao, Erica S, Meisenheimer, Robert C OH (2021) Alcohol Withdrawal Syndrome: Outpatient Management. Am Fam Physician 104(2): 253-262
- Kattimani S, Bharadwaj B (2013) Clinical management of alcohol withdrawal: A systematic review. Ind Psychiatry J 22(2):100-108.
- Max Bayard, Jonah Mcintyre, Keith R Hill, Jack Woodise, et al. (2004) Alcohol Withdrawal Syndrome Am Fam Physician 69(6): 1443-1450.
- Fabio Atilia, Roberta Perciballi, Claudia Rotondo (2018) Alcohol withdrawal syndrome: diagnostic and therapeutic methods Riv Psichiatr 53(3): 118-122.
- Robert S Hoffman, Gerald L (2023) Weinhouse. Management of moderate and severe alcohol withdrawal syndrome.
- Nathanael J McKeown DO (2022) Withdrawal Syndromes Workup. Medscape.
- Jesse S, Bråthen G, Ferrara M, Keindl M, Ben Menachem E, et al. (2017) Alcohol withdrawal syndrome: mechanisms, manifestations, and management. Acta Neurologica Scandinavica 135(1): 4-16.
- Hosh S, Jain R, Jhanjee S, Rao R, Mishra AK (2019) Alcohol Biomarkers and their Relevance in Detection of Alcohol Consumption in Clinical Settings. Int Arch Subst Abuse Rehabil 1(1): 002.
- Benzer DG (1994) Principles of Addiction Medicine. American Society of Addiction Medicine, Chevy Chase: Management of alcohol intoxication and withdrawal. American Society of Addiction Medicine.
- Hermann D, Weber Fahr W, Sartorius A, Hoerst M, Frischknecht U, et al. (2012) Translational magnetic resonance spectroscopy reveals excessive central glutamate levels during alcohol withdrawal in humans and rats. Biol Psychiatry 71(11): 1015-1021.
- Book SW, Myrick H (2005) Novel anticonvulsants in the treatment of alcoholism. Expert Opin Investig Drugs 14(4): 371-376.
- Rathlev NK, D'Onofrio G, Fish SS, Harrison PM, Bernstein E, et al. (1994) The lack of efficacy of phenytoin in the prevention of recurrent alcohol-related seizures. Ann Emerg Med 23(3): 513-518.
- Hammond CJ, Niciu MJ, Drew S, Arias AJ (2016) Anticonvulsants for the treatment of alcohol withdrawal syndrome and alcohol use disorders. CNS Drugs 29(4): 293-311.
- Richard d. Blondell (2005) Ambulatory Detoxification of Patients with Alcohol Dependence - American Family Physician.
- Long D, Long B, Koyfman A (2011) The emergency medicine management of severe alcohol withdrawal. American Journal of Emergency Medicine. W.B. Saunders 35(7): 1005-1011.
- Monte Secades R, Rabuñal Rey R, Guerrero Sande H (2015) Síndrome de abstinencia alcohólica en pacientes hospitalizados. Rev Clin Esp 215(2): 107-116.
- Rubin BK (1998) Thiamine Before Glucose to Prevent Wernicke Encephalopathy: Examining Conventional Wisdom. Jama 279(8): 583-584.
- Mayo Smith MF Pharmacological Management of Alcohol Withdrawal A Meta-analysis and Evidence-Based Practice Guideline Working Group on Pharmacological Management of Alcohol Withdrawal. Jama 278(2): 144-151.
- Mainerova B, Praskoa J, Latalova K, Axmann K, Cerna M, et al. (2015) Alcohol withdrawal delirium - diagnosis, course and treatment. Biomedical Papers 159(1): 44-52.
- Jesse S, Bråthen G, Ferrara M, Keindl M, Ben Menachem E, et al. (2017) Alcohol withdrawal syndrome: mechanisms, manifestations, and management. Acta Neurologica Scandinavic 135(1): 4-16.
- Maldonado JR (2017) Novel Algorithms for the Prophylaxis and Management of Alcohol Withdrawal Syndromes-Beyond Benzodiazepines. Critical Care Clinics 33(3): 559-599.
- Coomes TR, Smith SW (1997) Successful Use of Propofol in Refractory Delirium Tremens. Ann Emerg Med 30(6): 825-828.
- Hughes DW, Vanwert E, Lepori L, Adams BD (2013) Propofol for benzodiazepine-refractory alcohol withdrawal in a non-mechanically ventilated patient. American Journal of Emergency Medicine 32(1): 112.e3-112.e4.
- Malcolm R, Myrick H, Roberts J, Wang W, Anton RF, Ballenger JC (2002) The Effects of Carbamazepine and Lorazepam on Single versus Multiple Previous Alcohol Withdrawals in an Outpatient Randomized Trial. J Gen Intern Med 17(5): 349-355.
- Shah P, Stegner Smith KL, Rachid M, Hanif T, Dodd KW (2022) Front-Loaded Versus Low-Intermittent Phenobarbital Dosing for Benzodiazepine-Resistant Severe Alcohol Withdrawal Syndrome. Journal of Medical Toxicology 18(3): 198-204.
- Muncie HL, Yasinian Y, Oge L (2013) Outpatient management of alcohol withdrawal syndrome. Am Fam Physician 88(9): 589-595.
- Bayard M, McIntyre J, Hill KR, Woodside J (2004) Alcohol withdrawal syndrome. Am Fam Physician 69(6): 1443-1450.
- Elholm B, Larsen K, Hornnes N, Zierau F & Becker U (2011). Alcohol Withdrawal Syndrome: Symptom-Triggered versus Fixed-Schedule Treatment in an Outpatient Setting. Alcohol and Alcoholism 46(3): 318-323.
- Pribek IK, Kovacs I, Kadar BK, Kovacs CS, Richman MJ, et al. (2021) Evaluation of the course and treatment of Alcohol Withdrawal Syndrome with the Clinical Institute Withdrawal Assessment for Alcohol-Revised: A systematic review-based meta-analysis. Drug and Alcohol Dependence 220: 108536.






























