Initial Clinical Experience with a Photodynamic Polymeric Nail (Illuminoss) for Upper Extremity Metastatic Lesions and Trauma
Ajibola B Oladiran1, Raviv Allon2*, Utai Rudich3, Doron Norman3 and Yaniv Keren3
1Orthopaedic Surgery Unit, Department of Surgery, State Specialist Hospital, Akure, Ondo State, Nigeria
2Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Israel
3Orthopaedic Surgery Division, Rambam Health Care Campus, Haifa, Israel
Submission: August 05, 2022; Published: August 17, 2022
*Corresponding author: Raviv Allon, Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Israel
How to cite this article: Ajibola B O, Raviv A, Utai R, Doron N, Yaniv K. Initial Clinical Experience with a Photodynamic Polymeric Nail (Illuminoss) for Upper Extremity Metastatic Lesions and Trauma. Ann Rev Resear. 2022; 7(5): 555721. DOI: 10.19080/ARR.2022.07.555721
Abstract
Intramedullary devices for long bones fixation are an important tool in the arsenal of the orthopaedic surgeon. Understanding of the importance of soft tissue envelope in fracture healing as well as the benefits of limited soft tissue dissection, has given rise to the constant evolution of new methods for intramedullary fixation, whether for trauma or pathologic conditions. This is a report of our early experience with the IlluminOss PhotoDynamic Balloon (IlluminOss Medical, Inc., East Providence, RI, USA) for intramedullary fixation of non-weight-bearing long bones metastatic disease and fracture. We report a short series of five cases, of upper limb, long bone fixation, of which the characteristics of the condition challenged the common practice used today for fixation of long bones. Hence they were fixed with a novel polymeric balloon, which enables the surgeon to rapidly fix fractures with a method that minimises soft tissue injury, eliminates the need for proximal and distal locking, and potentially lowers complication rates, as well as limiting the interference with further imaging investigations.
Keywords: Intramedullary nail; polymeric balloon; Pathological fracture; Upper extremity trauma; Illuminoss
Introduction
The traditional intramedullary nail is a versatile and dynamic tool that has become a major option for fixation of various configurations of long bone fractures, whether traumatic or pathologic. The stability of the device depends on mechanisms that “lock” the nail in place to provide longitudinal and rotational stability. The various designs of intramedullary nails have evolved through the early unlocked metal Kunstcher nail to the modern precurved titanium locked nails [1]. The need for preservation of the soft tissue envelope in order not to interfere with bone healing, and to minimize risk to important anatomical structures, makes the use of minimally invasive techniques very attractive to the trauma surgeon. The Illuminoss photodynamic polymeric nail represents a recent development that enables bone stabilization using a light-curable polymer contained within an inflateable balloon catheter [2]. Vegt published a series of 41 osteoporotic long bones fixation using the Illuminoss system, including distal radius fractures and one case of humeral metastatic disease [2]. The radiolucent nature of the PhotoDynamic Balloon is of particular advantage especially in cases of pathological fractures as it avoids the production of artefacts on radiological investigations and allows for proper evaluation of recurrence or lesion expansion on follow-up. Earlier radiolucent intramedullary fixation methods have utilized these advantages [3].
In this novel polymeric balloon, after it’s insertion into the medullary canal, a polymeric liquid is injected along the balloon. This “ballooning” fills the medulla and follows its internal uneven diameters. Since proximal and distal canal diameters are greater than the mid-shaft isthmic portion of the canal, a rotation and longitudinal stability is achieved after the process of polymerization. This process facilitates another advantage of the illuminoss system, since interlocking screw are usually not necessary. Pathological humeral fractures constitute a particular challenge to the Orthopaedic surgeon [4]. Not uncommonly, fixation of a pathologic fracture in the humerus is made in order to improve overall quality of life (pain relief, better nursing, improved hygiene) rather than curing, since patient’s life span is often expected to be short due to the underlying disease and spread of metastasis. For this reason, a short rehabilitation period is more than desirable [5]. This is a report of our early experience with patients who had intramedullary fixation of upper limb long bone metastasis or fractures with the IlluminOss PhotoDynamic Balloon. Three cases are of pathological humeral fracture fixation due to metastasis. Two are of upper extremity fractures which exhibited special considerations that made the authors think “out of the box” in order to facilitate better care for the patient with lower rate of complications as expected by using a traditional surgical approach and fixation.
Patients and Methods
All patients were treated in our department. Two of the patients were males after trauma to their upper limb, mean age 68.5. Three females with humerus metastatic disease, mean age of 67.3.
Here are the details of each case and the rationale behind using this novel intramedullary device:
Case 1
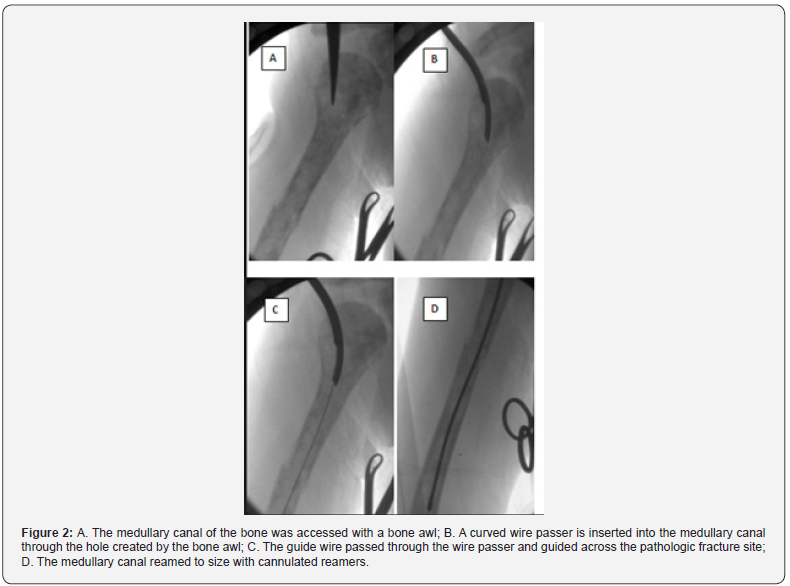
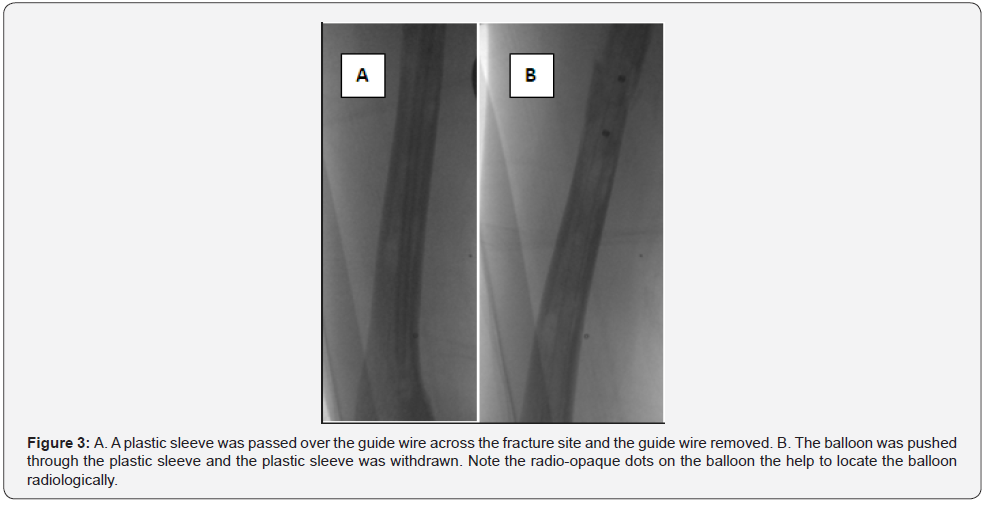
44 year old female with pathological midshaft right humeral fracture in end stage breast carcinoma with cervical spine and lung metastasis. The aim of fracture fixation was to stabilise the humeral shaft fracture in order to limit pain, allow better hygiene, and facilitate nursing care. Regional anaesthesia was administered via interscalene brachial plexus block on account of concerns of neurological injury from neck extension due to cervical involvement of the disease and difficulty with weaning off the ventilator on account of the lung metastasis. The patient was positioned supine and a single small skin incision was made over the greater tuberosity (Figure 1). The humeral medullary canal entered with a bone awl (Figure 2A). Following this a curved wire passer was introduced into the hole created by the awl (Figure 2B). A flexible guide wire was passed into the medullary canal (Figure 2C). Then cannulated reamers were passed over the wire to ream the canal to width (Figure 2D). Then a plastic sleeve was inserted into the medullary canal and the wire is pulled out (Figure 3A). The plastic sleeve helps prevent the Dacron balloon from being perforated or torn while being inserted into the canal.

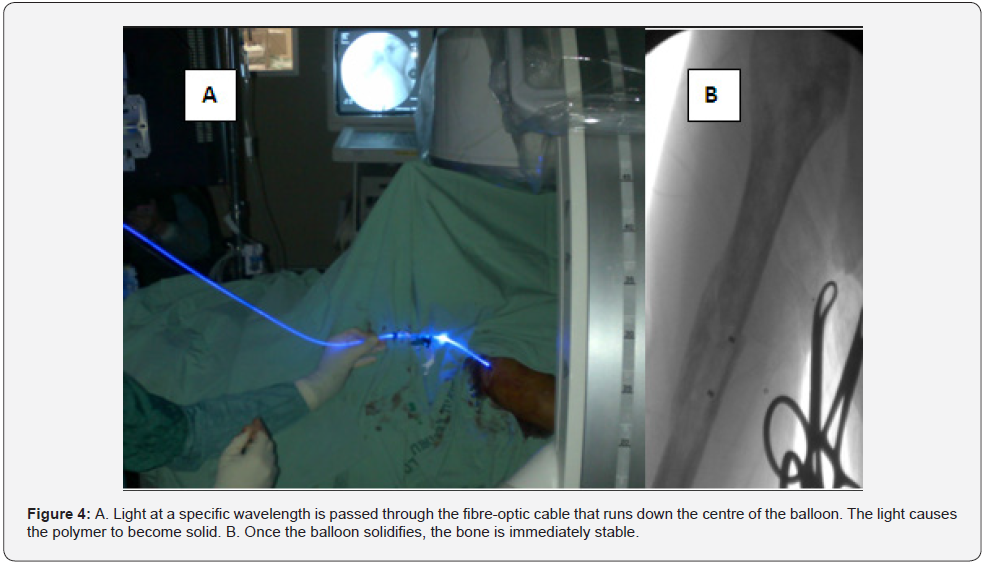
The balloon was pushed through the plastic sleeve, the plastic sleeve withdrawn (Figure 3A). The balloon has radio-opaque dots to enable it to be visualised radiologically. The balloon is then filled with the appropriate volume of polymer for the size of the balloon. After the balloon is filled, the light source is connected with the appropriate connectors and light at specific wavelength passed through a fibre-optic cable within the balloon (Figure 4A). The liquid polymer within the balloon solidifies on timely exposure to the light and the humerus is immediately stable (Figure 4B). The skin incision was closed with staples after suturing the supraspinatous tendon, and the patient was taken to the intensive care unit for post-operative care. At follow up on 29.9.2014, 18 days after her surgery, the patient was pain free and had no need for any form of external support such as a sling or a Miami brace. Unfortunately, the patient died two months after surgery on 14.11.2014, due to the progression of the primary disease. Even though, family and patient satisfaction from the procedure was high.
Case 2
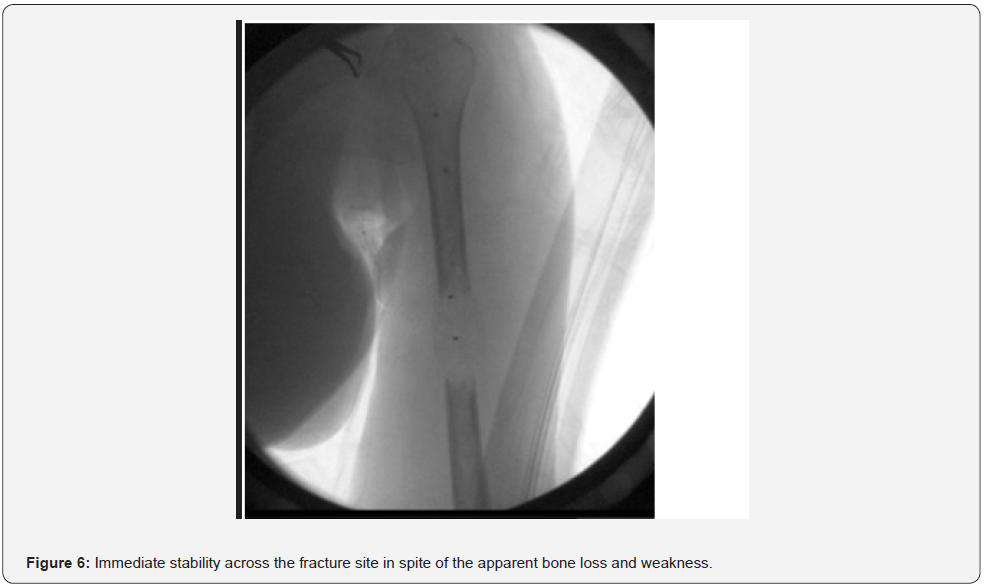
79-year-old female admitted on account of pain in the right arm. She had no prior history of trauma. Xray showed a lytic lesion in the midshaft of the left humerus (Figure 5). It was decided to fix her humerus while simultaneously having a metastatic workout. Histopathology from tissue derived from intramedullary reaming revealed cells indicative of a neuroendocrine carcinoma with lung or gastric carcinomas considered as differential diagnosis. She had her pathologic fracture fixed on 3.12.2014 (Figure 6). She was pain free and had a stable fixation post operatively, but she defaulted from clinic follow up. However, contact was made by the operating surgeon via phone six months after surgery and she reports excellent satisfaction from the surgery, complete relief of pain, satisfactory function of the left upper limb and no need for any form of external support.

Case 3
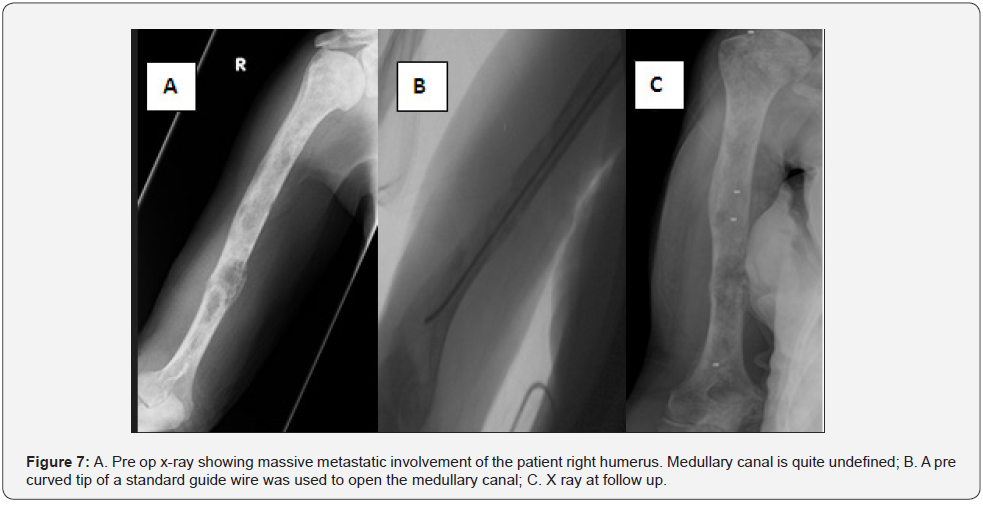
A 79 female with known disseminated metastatic breast cancer, was electively admitted due to massive involvement of her right humerus (Figure 7A). Having thrombocytopenia we decided to have the minimal surgery possible. After platelets infusion, she underwent insertion of an Illuminoss balloon under regional anesthesia as previously explained. Since her massive involvement, we were technically challenged by the inability to pass the Illuminoss super thin guide wire through the canal and lesion for reaming. Hence, we used a standard intramedullary guide which we bent a little at the far end (Figure 7B). This enabled us to create a new canal by finding our way under fluoroscopy. Every advancement along the canal was documented on two views (Antero posterior and lateral) to avoid cortex penetration. An orthopaedic chuck was used to rotate the guide wire when an undesired route was documented. Finally, a new canal was established and an Illuminus ballon was passed and inflated after appropriate reaming (Figure 7C).
Unfortunately, the patient died 39 days after the procedure due to liver cirrhosis.
Case 4
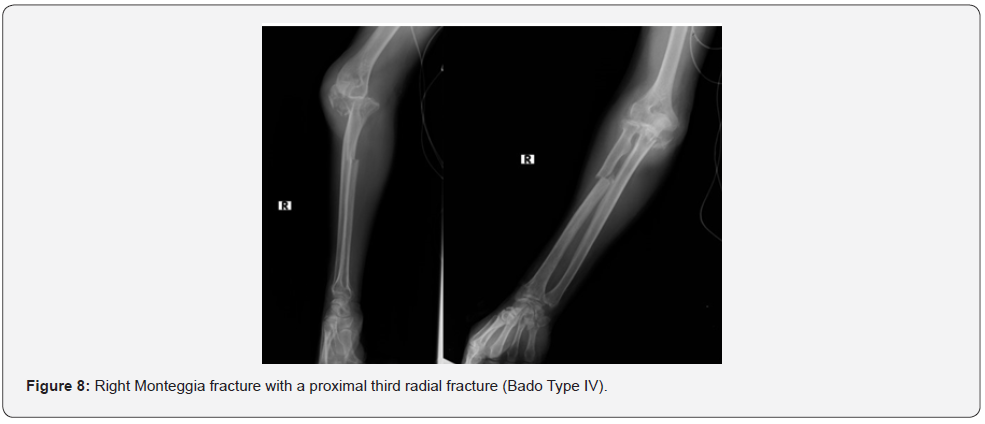
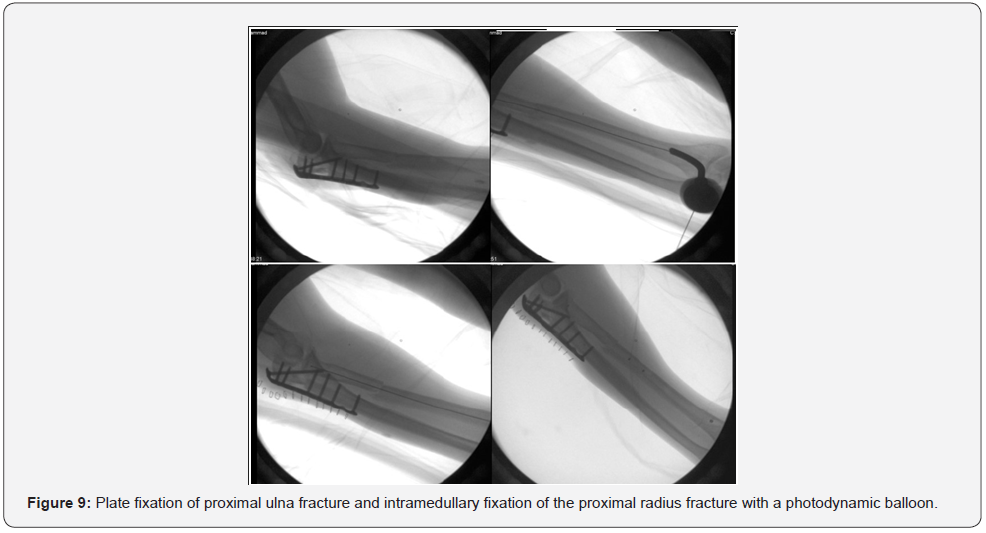
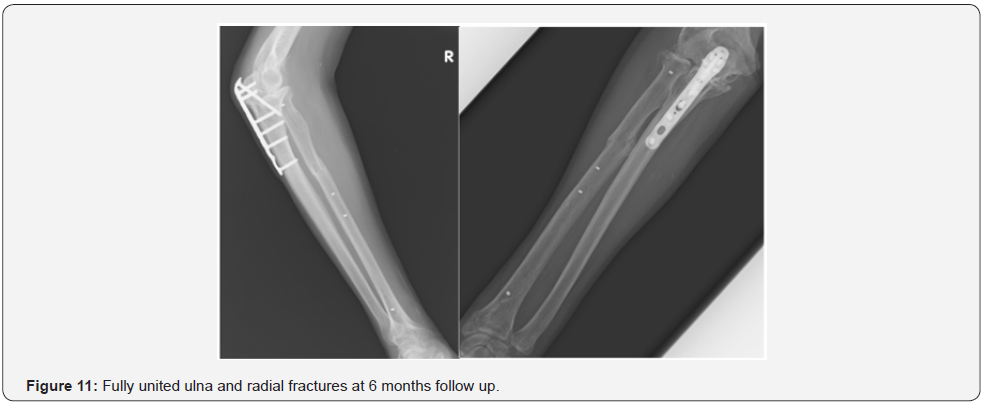
68-year-old male victim of a motorcycle accident. He sustained a right Monteggia fracture with a proximal third radial fracture (Bado Type IV) (Figure 8). The challenge with management of Monteggia fractures is well illustrated by Watson-Jones in his 1943 text. He stated that “no fracture presents so many problems; no injury is beset with greater difficulty; no treatment is characterised by more general failure” [6]. While improvements in surgical diagnosis and care have greatly improved management, Monteggia fractures are still a challenge to manage. Radial head dislocations may lead to injury of the radial nerve. The posterior interosseous branch of the radial nerve, which courses around the proximal third of the radius, is especially at risk from operative dissection and placement of retractors and implants used in the process of plating proximal third radius fractures [7]. Although plate fixation is well established as the standard of care for most radius and ulna shaft fractures, the option of a minimally invasive intra medullary fixation for proximal radial fracture can greatly reduce the risk of iatrogenic injury to the posterior interosseous nerve (Figure 8). The patient had surgery done on 3.12.2014 with plate fixation of the proximal ulna fracture (Figure 9-10). It was decided to fix the proximal third radius fracture with the illuminoss system, using a radial styloid entry point. At follow up 6 months after surgery, he had full range of motion at the elbow with fully united fractures of both the ulna and the radius (Figure 11).


Case 5
A 59-year-old male victim of a motorcycle accident. In his right forearm he sustained an open (gustilo 3c) segmental radius shaft and ulna midshaft fracture and radial head dislocation (Monteggia fx , Bado Classification Type IV) (Figure 12). He was admitted to our hospital one-month post injury after being treated previously at another hospital where he had open reduction and internal fixation to his ulna shaft open fracture only. On arrival to our institution he exhibited vast skin loss, elbow and forearm instability, and partial ulnar motor and sensory loss.
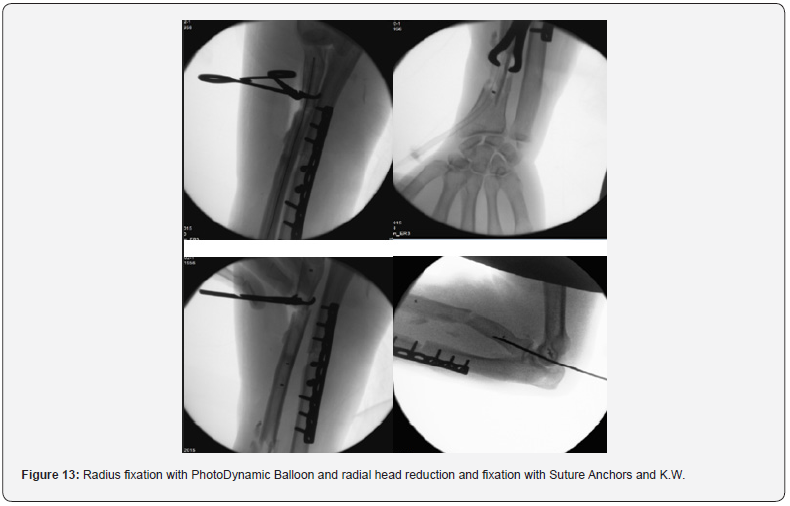
Since we were reluctant to make skin incisions through the damaged skin for fear of infection and wound dehiscence, we decided to try and achieve as good as alignment that can be achieved by closed means, and stabilize the radius fractures using the Illuminoss balloon. Due to radial head dislocation, further reduction and fixation were achived with suture anchors. Since his radial head could not be relocated in front of the capitellum, and formal reconstruction was out of the question, the joint was reduced and fixed with a trans joint Kirschner wire (K.W) and a bone anchor. The surgery was done with minimal soft tissue striping and minimal skin incision to avoid additional neurologic damage and interfering with the contaminated area (Figure 13).
Later on he had plastic surgery for skin graft.
The K.W was withdrawn after 3 weeks. At follow up at 5 weeks post op he had slight neurological improvement, good skin healing and started elbow motion (Figure 14). No apparent bone healing was noted at the ulnar side, but callus formation was apparent at the radius.
Discussion
The IlluminOss PhotoDynamic Balloon gives a fast, versatile, minimally invasive mode of fixation of non-weight-bearing long bone fractures. Thus, it is suitable for use in fractures involving the clavicle, humerus, radius, and ulna. By design the system requires minimal soft tissue dissection, as the balloon is introduced through the end of the bone into the intramedullary canal. Advantages of the system include the use of a single small incision and the minimally invasive nature of the procedure. These confer the advantages of less post-operative pain, reduced post-operative analgesia requirements, shorter hospital stay and shorter rehabilitation time. The lack of necessity for locking screws significantly shortens the operating time. Additional fixation devices e.g. plates and screws can also be used to achieve extra stability in addition to the balloon if need be. The balloon is radiolucent and allows proper visualisation of the fracture site which is particularly important for follow up of pathological fractures. Disadvantages include the high cost of the equipments and implants. Also, the removal of the implants is difficult in cases when this is required like in the rare occasion of implant failure.

Conclusion
Fracture management is best done with a means of rapid and stable fixation with a short period of rehabilitation. A mean of fixation that allows minimal tissue dissection, immediate stability post operatively and proper visualisation of the bone and fracture site for follow-up purposes is a major advantage. The Photo Dynamic Balloon is a versatile method providing these benefits and should be considered in unique cases of non-weight bearing long bones fractures whether traumatic or pathologic.
References
- Bong MR, Koval KJ, Egol KA (2006) The history of intramedullary nailing. Bull NYU Hosp Jt Dis 64(3-4): 94-97.
- Vegt P, Muir JM, Block JE (2014) The Photodynamic Bone Stabilization System: a minimally invasive, percutaneous intramedullary polymeric osteosynthesis for simple and complex long bone fractures. Med Devices (Auckl) 7: 453-461.
- Collis PN, Clegg TE, Seligson D (2011) The invisible nail: a technique report of treatment of a pathological humerus fracture with a radiolucent intramedullary nail. Injury 42(4): 424-426.
- Franco P (2014) Minimizing a tricky situation in breast irradiation with helical tomotherapy. Tumori 100(2): e35-40.
- Laitinen M, Nieminen J Pakarinen TK (2011) Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 131(4): 503-508.
- Watson-Jones R (1943) Fracture and Joint injuries, 3rd, Editor. Williams and Wilkins: Baltimore.
- Ruchelsman DE (2009) Persistent posterior interosseous nerve palsy associated with a chronic type I Monteggia fracture-dislocation in a child: a case report and review of the literature. Hand (N Y) 4(2): 167-172.






























