The Feasibility of a Text-Delivered Intervention to Improve Dietary Habits, Stress Management Behaviors and Create Awareness of Food Assistance Resources Among College Students
Dorcas R Mukigi and Onikia Brown*
Department of Nutrition, Dietetics, & Hospitality Management, Auburn University, USA
Submission: November 13, 2019;Published: December 02, 2019
*Corresponding author: Onikia Brown, Department of Nutrition, Dietetics, & Hospitality Management, Auburn University, USA
How to cite this article: Dorcas R M, Onikia B. The Feasibility of a Text-Delivered Intervention to Improve Dietary Habits, Stress Management Behaviors and Create Awareness of Food Assistance Resources Among College Students. Ann Rev Resear. 2019; 5(3): 555665. DOI: 10.19080/ARR.2018.04.555665
Abstract
Food insecurity in college students is associated with lower self-reported health, poor dietary habits, inadequate sleep, mental health issues, and lower grade point average (GPA). This study aimed to evaluate the acceptance and effectiveness of health-related text messages on college students’ dietary habits, stress management behaviors and awareness of food assistance resources. Forty-six college students with mobile phones were recruited during the Spring semester 2018. The intervention group received 3 messages per week for 7 weeks and the control group received the same information in an email attachment at post-intervention. A pre and post online survey assessed the students’ fruit and vegetable intake, perceived stress, hours of sleep and awareness of food assistance resources. The intervention group significantly (p < 0.05) reduced perceived stress from baseline 27.71 ± 5.18 to 17.33 ± 5.20 and increased intake of fruit and vegetable by 0.5 cups/day at post-intervention. Text delivered messages appear to be acceptable and have the potential to promote positive dietary habits, stress management behaviors, and create awareness of food assistance resources among college students.
Keywords: Disaster; Urban area; Tannery industry; Environmental pollution; Bangladesh
JEL Classification: P23, Q52, Q54.
Abbreviations: FGD: Focused Group Discussion; KII: Key Informant Interview; ETP: Effluent Treatment Plant; BELA: Bangladesh Environment Lawyers Association
Introduction
College students, often referred to as emerging adults, experience transitions in health- related behaviors as they adapt to life in college [1]. This transitional period is characterized by changes in dietary habits, stress and mealtime behaviors [2-5]. Additionally, emerging adults often lack resources and skills required for food preparation. These factors contribute to their increased risk for food insecurity [6,7]. Dietary habits that are consistent with the national dietary guidelines have been found to promote health, but college students do not meet these guidelines [8-10]. Studies have reported that college students have poor dietary habits and they do not meet their recommended daily intake of fruit and vegetable [9,11,12]. One study that examined the relationship between food insecurity and fruit and vegetable intake among college students found that food insecure students ate significantly lower daily servings of fruit and vegetable as compared to students with high food security controlling for confounding factors such as car access, race/ethnicity and gender [13]. College students also skip meals, consume high amounts of snacks and high calorie food items such as sugar sweetened beverages (SSB) [14,15]. Furthermore, National Health and Nutrition Examination Survey (NHNES) data indicate that young adults - age category in which most college students fall under, have the highest mean percentage of daily calories from SSB [16].
College students are prone to stress due to the transitional nature of college life [17]. According to the American College Health Association (ACHA) national survey, 57% of college students report elevated levels of stress [18]. Stress among college students is caused by numerous factors including adjusting to life away from family, developing relationships, need to maintain high level of academic achievement, juggling time demands from school and work, and increased responsibilities [19]. These stressors bring about change in sleeping patterns and may influence sleep quality and quantity [4,17]. Studies have shown that a majority of college students do not meet the recommended 9 hours of sleep per night [4,17]. Sufficient sleep quality and quantity are critical determinants of health, and recently the US government added sleep as an objective in Healthy People 2020 [4,17,20]. There is need for campus administrators and researchers to come up with interventions and avail information on stress management to help students cope better with stress.
Mobile phones have been used to provide widely accepted and inexpensive medium in which health related information can be communicated to the targeted populations [21,22]. In a study conducted by Pew Research Center, 94 % (n = 273, aged 18-26 years) of college aged students reported having mobile phones and 89% reported having their phones in near proximity all the time, including bedtime [23]. College students with mobile phones reported receiving and sending a mean of 119 text messages a day.24 With the incorporation of text messaging in the day-to-day lives of college students, it provides opportunities in which behavior change interventions can be delivered in a platform that is popular and easily accessed by the target population [23-25]. The time that students spend in college is critical for the development of lifelong habits. Therefore, researchers should be deliberate in evaluating health behaviors in this age group and in providing appropriate and directed health education and information to improve health behaviors for optimum health outcomes. The purpose of this study was to evaluate the effectiveness of using text delivered messages to improve college students’ dietary habits, stress management behaviors and create awareness of food assistance resources.
Methods
This study was approved by the University’s Institutional Review Board (IRB). An email was sent to conveniently selected professors in the college of human sciences requesting them to send a recruitment email with a link to the 6 item United States Department of Agriculture (USDA) food security survey to their classes. The same recruitment email was sent to on campus food pantry and Campus Kitchen mailing list. The Campus Kitchen is a student led program that fights hunger on campus and in the community by collecting unserved food from dining halls and redistributing it to those in need. To protect the identity of those who receive assistance from the food pantry and Campus Kitchens, the recruitment email was sent by the concerned staff and faculty. Inclusion criteria were age ≥ 18 years and regular access to a mobile phone with a texting plan. When 50% of the target population of either food secure or insecure was achieved, participation was closed for that category. The participants were randomly assigned to the control or intervention group based on their food security status in the order that they completed the online survey. The participants completed an online survey powered by Qualtrics survey Software (version 2018; Qualtrics Provo, Utah) at baseline and post-intervention.
The survey included a consent letter, demographic data form, food assistance resources awareness and utilization data collection tool [26], National Cancer Institute fruits and vegetables screener [27], sugar sweetened beverage screener [15], Cohen’s Perceived Stress screener [28], hours of sleep [29], and meal behavior data collection tool [5]. At post-intervention, the intervention group were asked to state the number of text messages they read during the intervention, what they liked most about the messages and to suggest their preferred medium for receiving health information. The intervention messages were developed from formative interview data, tested using cognitive interviews [30], and organized in 3 major themes: eating habits, stress management and food assistance resources awareness. The intervention group received 3 text messages per week for 7 consecutive weeks that contained information to encourage healthy dietary habits, stress management strategies and food assistance resources. The intervention participants were instructed during the consent process to text “STOP” if they no longer wished to receive text messages at any point in the study. The control group received an email attachment containing all the messages at the end of the study. The participants were compensated for completing surveys ($5 at baseline and $10 at post-intervention).
a. Scoping the target area was done by formation of Ward DMC/Ward level working group/committee, consensus building with CC/Ward DM, facilitator team formation & training, distribution of Roles and Responsibilities and orientation, and primary and Secondary data collection,
Measures
Demographics
Demographic information including age, classification, gender and race/ethnicity were assessed at baseline.
Anthropometrics
Participants reported their weight (pounds) and height (feet and inches) respectively. These measurements were then transformed to kilograms (kg) and meters (m) to calculate body mass index (BMI) by: (BMI = weight (kg)/ [height (m)]2. BMI of each participant was classified as either underweight (< 18.5), normal (18.5-24.9), overweight (25.0-29.9) and obese (≥ 30) [31]. Weight was a secondary study outcome.
Food Assistance Resource Awareness
Questions to assess awareness and utilization of food assistance resources were adapted from a similar study.26 Participants were asked, “Are you aware of places on campus where you can receive supplemental food if needed?”, and “Is there a food pantry on campus?” Those who answered “yes” were asked, “Have you ever used the on-campus food pantry or received free meals offered by the Campus Kitchens?”, if they answered “yes”, they were asked, “How times a semester do you get food from campus food pantry or Campus Kitchens?” Feelings towards utilizing the food pantry were also measured by asking the following question, “Please tell us how you may feel should you ever need to receive food from the food pantry or Campus Kitchens”. The participants were asked to rate each of the following feelings: encouraged, supported, satisfied, ashamed, embarrassed or loss of self-respect on a scale from 1 to 5; 1 = strongly disagree, 2 = agree, 3 = neither agree or disagree, 4 = disagree and 5 = strongly disagree. Participants likelihood to use food assistance resources were evaluated by asking the participants the following questions,
“Please tell us how likely you are to use the following resources:
i) Ask parents, friends, relatives, or partner to send money,
ii) Ask parents, friends, relatives, or partner to send/ purchase food,
iii) Attend events offering free food,
iv) Borrow money or
v) Dumpster dive to receive food assistance.
Responses were;
i) Extremely likely
ii) Moderately likely
iii) Neither likely or unlikely
iv) Moderately unlikely
v) Extremely unlikely
Fruits and Vegetables Intake
The short form National Cancer Institute fruits and vegetables screener [27] was used to assess intake of fruit and vegetable as cups per day. This screener measures the frequency and average consumption of fruits and vegetables over the last one month. The variables data were transformed to cups per day before analysis.
Sugar Sweetened Beverage (SSB) Intake
An adapted 8 question instrument15 was used to assess the frequency and quantity intake of SSB in the previous month. The SSB queried included non-diet soda, fruit drinks, non-diet energy drinks and sweetened tea. The responses for frequency were never or less than 1 per month, 1-4 per month or 2-6 per week and the responses for quantity included none (all SSB), 12 oz can, restaurant glass/cup, 20 oz bottle (soda and fruit drinks), or 2 liter (soda) or 64 oz bottle (fruit drinks), 2 to16 oz energy drinks, and ≤ 12 oz, or ≥ 12 oz sweetened tea. The average number of kilocalories per day from SSB consumption were computed by converting amounts and frequency into ounces per day and multiplying by respective kilocalories per ounce.
Mealtime Behavior
An adapted instrument [5] for measuring healthful mealtime behavior was used to assess mealtime planned self-regulation and self-instruction.
For self-regulation, the participants were asked to specify how often in the last 3 months they had:
i) Purposely added vegetables to their meals and snacks,
ii) Planned quick, easy and healthy snacks,
iii) Selected beverages with health in mind,
iv) Been flexible and sensible in food choices.
To assess self-instruction for healthful mealtime behavior, participants were asked how often in the past 3 months they had:
i) Told myself to allow room for an occasional treat food or dessert for just plain enjoyment,
ii) Told myself fruits and vegetables should be included in every meal,
iii) Reminded myself to eat in moderation,
iv) Reminded myself that healthy meals do not require a lot of work,
v) Reminded myself that planning quick and simple meals is important,
vi) Reminded myself to think about my beverage choices”. The responses were on a 5-point Likert scale: 1 = never, 2 = sometimes, 3 = regularly, 4 = often and 5 = always. Higher scores indicate healthful mealtime behaviors.
Perceived Stress
Cohen’s Perceived Stress Scale (10-item) 28 was used to measure participants perceived stress. This scale appraises the degree to which individuals find situations in their lives as stressful. The scale asked how overloaded, unpredictable and uncontrollable the participants found their lives in the last one month. The responses were on a 5-point Likert scale with 0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, and 4 = very often. Questions 4,5, 7 and 8 were positively worded and therefore scores were reversed (0 = 4, 1 = 3, 2 = 2, 3 = 1 and 4 = 0). Higher scores indicate high perceived stress.
Hours of Sleep
Participants were asked to report the average number of hours they sleep in a 24-hour period. This question is drawn from the Behavior Risk Factor Survey [29].
Text Message Evaluation
During the study, the intervention group participants were asked to reply “yes” to text messages to indicate that they had received and read the intervention messages. Additionally, at post-intervention, intervention group participants were asked to report if they received and read the messages and indicate the number of messages they read. At post-intervention, the intervention participants were asked to suggest preferred medium (s) of message delivery and improvements for the intervention messages. The control participants were asked to suggest their preferred method of health information communication at post-intervention.
Data Analysis
The data were analyzed using SPSS statistical software program (version 23; IBM SPSS, Armonk, New York). Descriptive statistics were used to analyze baseline demographic, food security status and anthropometric characteristics (BMI) and were expressed in frequencies and percentages. Chi square analysis were used to analyze differences in categorical data. Oneway analyses of variance (ANOVA) was used to assess bivariate associations between food security status and fruit and vegetable intake, calories from sugar sweetened beverages, perceived stress scores, hours of sleep and weight of all participants at baseline. To determine differences between intervention and control group outcome variables, repeated measures ANOVA were performed. Significance was reported for time, group and group x time. Data from participants who did not complete postintervention survey were excluded in the final analysis. P values ≤ 0.05 were considered as statistically significant.
Results
Participants

Eating Behavior
At post-intervention, although not statistically significant, the intervention participants increased their daily fruit and vegetable intake by half a cup whereas the control group intake remained essentially the same as measured by the National Cancer Institute fruits and vegetables [27]. The intervention and control group reduced the calories from the intake of SSB by 19 and 30 calories, respectively. Planned self-regulation and reported self-instruction scores for healthful mealtime behavior at baseline and post-intervention were approximately 3 on a scale of 1 to 5 for both groups, with higher score indicating greater intention for behavior change or current behavior (Table 2).
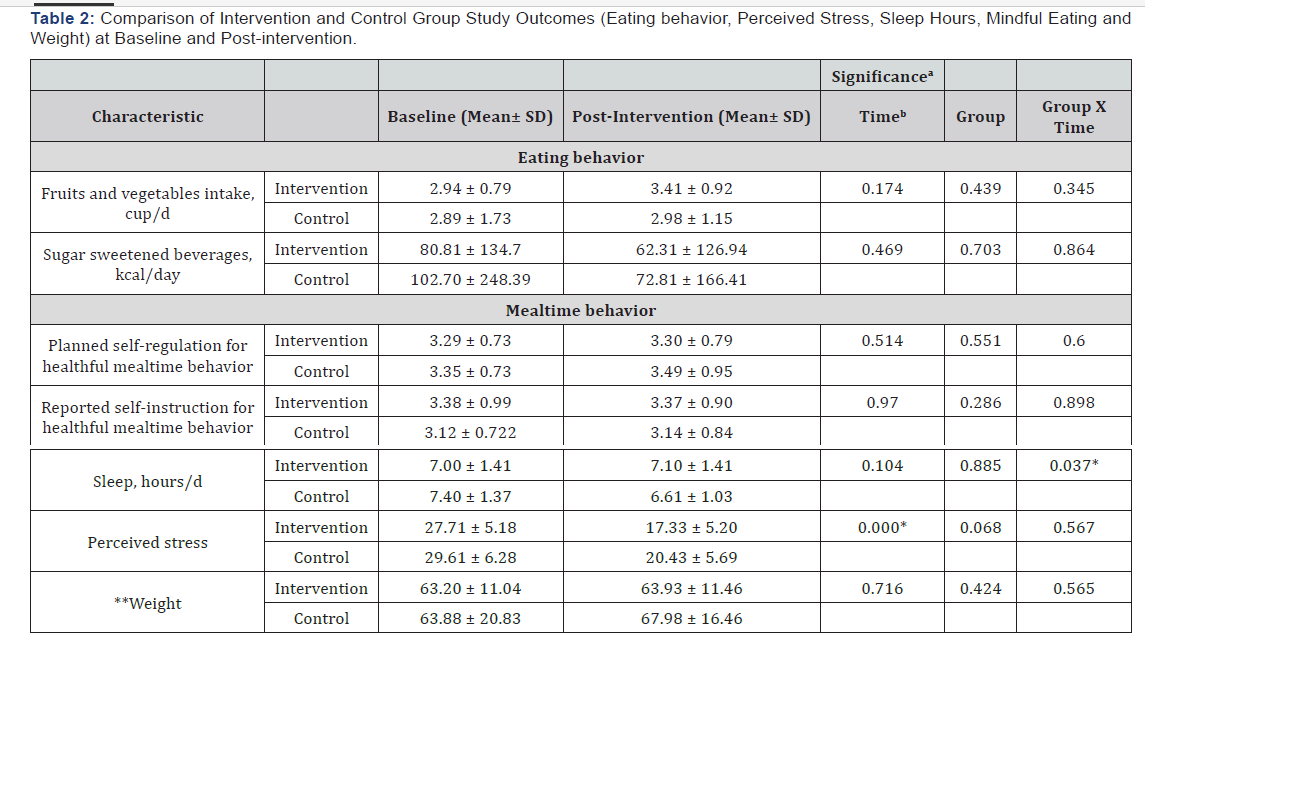
Hours of Sleep and Perceived Stress
At baseline, the food secure students had more hours of sleep than the food insecure students (7.90 ± 1.29 vs 6.68 ± 1.22, respectively; p < 0.05), Figure 1. There was significant group x time interaction for sleep; the intervention group reported a higher number of sleep hours (7.40 ± 1.37) compared to the control group (6.61 ± 1.03) at post-intervention (Table 2). There was significant time interaction for perceived stress; the intervention and control groups significantly reduced perceived stress at when within group baseline and post-intervention scores were compared; 27.71 ± 5.18 to 17.33 ± 5.20 and 29.61 ± 6.28 to 20.43 ± 5.69; p < 0.05), respectively (Table 2). For the secondary outcome of weight, there were no statistically significant differences when baseline and post-intervention measurements were compared for both groups (Table 2). However, food insecure students weighed significantly more than the food secure students at baseline and post-intervention (60.93 ± 14.76 vs 69.94 ± 12.86, respectively; p < 0.05), Figure 2.

Food Assistance Resource Awareness and Utilization
At baseline, 39% of the participants agreed that using the food pantry to get food assistance would make them feel encouraged, supported and satisfied (Figure 3). Also, the participants reported that they utilized the food pantry at least 4 times per semester. There was significant increase in the percentage of intervention participants who knew places on campus that provide supplemental food assistance and where the food pantry is located on campus (Table 3).

Note: Results are presented based on percent affirmative answers given by participants. Chi square analysis were used to analyze the responses.
*Significant difference in the change in food assistance resources awareness between control and intervention group, p <0.05.
Text Message Evaluation
One hundred percent of the intervention participants reported that they received and read the messages and there was 100% retention of participants. Fifty-seven percent of the intervention participants read 15-21 intervention text messages. Most of the control (70%) and 38% of intervention participants reported that email is their most preferred method to receive health information. Some of the suggestions for improvements include: “start an Instagram page to post healthy (food) pictures and ideas”, “make messages participant specific” and “reduce the length of some of the messages.” Two participants felt that the messages were “great”.
Discussion
College students often have unhealthy dietary habits that include low intake of fruits and vegetables [3], and increased intake of fast foods and SSB [14,15]. Due to busy schedules and increased responsibility, college students have increased levels of stress and inadequate sleep [17,18]. Additionally, studies have shown that college students have increased risk of food insecurity due to increasing cost of attending college, developing food and financial management skills and limited income [7,32]. For these reasons, we assessed the effects of a 7-week text delivered intervention on eating habits (intake of fruit and vegetable, sugar sweetened beverages and mealtime behavior), perceived stress, and awareness of food assistance resources in a random sample of college students in a public university in southeast United States. As expected, at baseline, the intake of fruit and vegetable for both the intervention and control groups were consistent with that of other US college students and did not meet the recommended 5 or more daily servings of fruits and vegetables [33,34]. Although not statistically significant, the intervention group participants reported an increase in the intake of fruit and vegetable at post-intervention, whereas the control participants maintained their intake. Other studies reported similar outcomes in that there were small increases in fruit and vegetable intake at post-intervention [35-37].
These trends point to the existence of barriers to college students’ intake of fruit and vegetable that includes access, costs and time constraints [13,38]. College students report that lack of grocery stores and transportation to access off campus stores as major environmental barriers to consumption of fruit and vegetable [38]. Furthermore, college students often have busy schedules and are on limited budgets and report not having time to purchase fruit and vegetable regularly and find their cost to be expensive, respectively [13,38]. Given the benefits of fruits and vegetables in health promotion, there should be continued interventions and campaigns to promote intake of fruit and vegetable intake among college students. Although there wasn’t a significant difference in the calories from SSB between and within the intervention and control groups at baseline and at post-intervention, all the participants in this study reported lower intakes of sugar sweetened beverages compared to other young adults (20-34 years) in the US [39]. Similar findings were reported in two studies that evaluated the effectiveness of webbased and multi-modal interventions to modify dietary habits of college students in that they found no significant reduction in energy intake from SSB [2,35]. Increased intake of sugar sweetened beverages is positively associated with increased body weight and risk of obesity across all groups [40].
In the current study, a majority of study participants had normal BMI at baseline and at post-intervention. This can conservatively indicate that their normal BMI is linked with their low intake of calories from SSB. Although the intervention participants did not report significant changes in planned selfregulation and self-instruction for healthful mealtime behavior, their mealtime behavior scores at post-intervention were similar to those reported by other student samples [2]. Due to busy class schedules and assignments, college students often develop poor eating habits such as snacking on unhealthy food items and skipping meals [3]. Healthful mealtime behavior such as budgeting and shopping for food, planning regular meals and healthy snacks have been associated with healthy dietary habits and weight maintenance by college students [41]. Additionally, planning and tracking snacks and meals have been associated with reduced intake of SSB and greater intakes of fruit and vegetable [5]. It is important that healthful mealtime knowledge and skills are imparted on students early in their Freshmen years and continued throughout their college years. Increased levels of stress are positively associated with reduced hours of sleep [4].In the current study, participants in the intervention and control group had less than the 9 recommended hours of sleep per day [5] and less than amounts (8.4 hours) reported in another study [4].
The intervention group participants maintained their hours of sleep while the control group significantly reduced their sleep time when baseline and post-intervention hours of sleep were compared. Perceived stress among the intervention group participants significantly reduced at post-intervention. These results indicate that the text delivered messages encouraging positive stress management behaviors and thus were successful in reducing the intervention participants perceived stress. Our study found that food insecure students utilize the oncampus food pantry at least 4 times a semester, this is twice the amount reported in a study that investigated predictors of food assistance resource use [26]. A recent study found that 30.8% of food insecure students were not aware of the existence of a food pantry on their campus [26]. Additionally, researchers reported that although 6.6% of food insecure students were aware of food assistance resources, only 2.3% utilized them [32]. As an increasing number of universities establish food pantries [42], it is important to make students aware of the existence of such resources and to initiate conversations with students in order to identify barriers and facilitators of resource use. Promising outcomes were observed in our study that used text delivered messages among college students.
The100% retention of the intervention participants may be attributed to the fact that text messaging is widely accepted and fully integrated into the lives of college students, and that text messages are not invasive. Also, the majority (57%) of the intervention participants reported reading 15-21 intervention messages. At the end of the study, one participant stated, “I thought they (messages) were great” this indicates acceptability of receiving health related information via text in this population. This study supports other evidence of acceptability of textmessage based health information intervention [38]. This study had a few limitations, all measures were self-reported and therefore the responses were dependent on the participants’ honesty and memory in answering the study questions. The sample was small, and the participants were not balanced in gender, student’s classification and race/ethnicity. Future studies should consider using multiple recruitment approaches to attract a more balanced group of participants. The intervention focused on three broad topics and this may explain the modest results in this study. Lastly, since there was no long-term follow-up for this study, there is no way of measuring if the observed behavior changes had long lasting effects or if they occurred during the intervention period only. Future research should be longitudinal in nature to examine the long-term effect of text delivered messages on dietary habits, perceived stress and awareness of food assistance resources among college students.
Conclusion
The current study proved that text delivered messages were effective in reducing perceived stress scores, reducing calories from SSB, increasing the intake of fruit and vegetable, and increasing awareness of food assistance resources among college students. Based on these changes, retention and positive evaluation comments made by study participants, text delivered messages were acceptable and effective for this audience. We recommend that future studies use repetitive text messages that include visual aids, as well as have long-term follow-ups to determine long-term behavior change. We also recommend that future studies evaluate diet quality of study participants using 24-hour dietary recall.
References
- Rodrigues AMS, Scatena LM, Vendramini SHF, Canini SRMS, Villa TCS, et al. (2012) Avaliação do acesso ao tratamento de tuberculose por coinfectados ou não pelo vírus da imunodeficiência humana. Rev Esc Enferm USP 45(5): 1163-1169.
- Global tuberculosis report 2014. World Health Organization.
- San Pedro A, Oliveira RM (2013) Tuberculose e indicadores socioeconômicos: revisão sistemática da literatura. Rev Panam Salud Publica 33(4): 294-301.
- Secretaria de Vigilância em Saúde-Ministério da Saúde (2015) Detectar, tratar e curar: desafios e estratégias brasileiras frente à Boletim Epidemiológico 46(9): 1-17.
- Secretaria de Saúde do Estado do Ceará (2015): Tuberculose. Fortaleza, Boletim epidemiológico, p. 6.
- Secretaria de Vigilância em Saúde-Ministério da Saúde (2014)O controle da tuberculose no Brasil: avanços, inovações e desafios. Boletim Epidemiológico 45(2): 1-13.
- Rodrigues júnior AL, Ruffino-netto A, Castilho EA (2014) Distribuição espacial do índice de desenvolvimento humano, da infecção pelo HIV e da comorbidade AIDS-tuberculose: Brasil, 1982 - 2007. Rev Bras Epidemiol 17(2): 204-215.
- Barbosa IR, Pereira LMS, Medeiros PFM, Valentim RS, Brito JM, et al. (2013) Análise da distribuição espacial da tuberculose na região Nordeste do Brasil, 2005-2010. Epidemiol Serv Saúde 22(4): 687-695.
- Ceará em mapas (2007) Fortaleza: Instituto de Pesquisa e Estratégia Econômica do Ceará.
- Estados (2016) Instituto Brasileiro de Geografia e Estatística-IBGE, Brazil.
- Santos SM, Souza WV (2007) Introdução à estatística espacial para a Saúde Pú Ministério da Saúde, Brasília.
- TERRAVIEW 4.2.2 (2016) São José dos Campos, SP: INPE, Brazil.
- Druck S, Carvalho MS, Câmara G, Monteiro AMV (2004) Análise espacial de dados geográ Planaltina: Empresa Brasileira de Pesquisa Agropecuária.
- Coordenadorias regionais de saúde (2010). Fortaleza: Secretaria Estadual de Saúde do Ceará.
- Viana PVS (2014) Tuberculose no Brasil: Uma análise dos dados de notificação, segundo macrorregião e raça/cor, para o período 2008-2011. Fundação Oswaldo Cruz, Escola Nacional de Saúde Pública Sergio Arouca, Brasil.
- Perfil Básico Municipal (2014) Fortaleza: Instituto de Pesquisa e Estratégia Econômica do Ceará.
- Farias EJS, Albuquerque IMN, Araújo RA, Soares JSA, Linhares MSC (2013) Análise epidemiológica dos casos de tuberculose notificados no município de Sobral- CE no período de 2007 a 2011. Sanare 12(1): 33-39.
- Costa MCL, Pequeno R (2015) Fortaleza: transformações na ordem urbana. Observatório das metró
- Pinto ML, Silva TC, Gomes LCF, Bertolozzi MR, Villavicencio LMM, et al. (2015) Ocorrência de casos de tuberculose em Crato, Ceará, no período de 2002 a 2011: uma análise espacial de padrões pontuais. Rev Bras Epidemiol 18(2): 313-325.
- Santos NSGM, Santos MLSG, Vendramini SHF, Villa TCS, Ruffino-netto A, et al. (2014) Tuberculose e análise espacial: revisão da literatura.Cienc Enferm 20(2): 117-129.
- Paiva SS (2013) Distribuição espacial e determinantes sociais de saúde na população com Aids no Ceará [Tese]. Fortaleza: Universidade Federal do Ceará, Faculdade de Farmácia, Odontologia e Enfermagem, Departamento de Enfermagem, Programa de Pós-Graduação em Enfermagem, Doutorado em Enfermagem.
- Lopes EM, Pedrosa NL, Holanda ER, Almeida RLF, Kerr LRFS, et al. (2015) Aids em crianças: a influência dos diferenciais socioeconômicos no município de Fortaleza, Ceará, Brasil. Cadernos de Saúde Pública 31(9): 2005-2016.






























