Causes of Death of Patients Living with HIV in the Section of Infectious Diseases at the University Hospital of Brazzaville
Ossibi Ibara BR*, Bemba ELP, Okemba Okombi FH, Adoua Doukaga Tatia, Sekangué Obili G, Angonga Ellenga Mbolla BF and Ikama MS
Faculty of Health Sciences, Marien Ngouabi University, Brazzaville,Congo
Department of Infectious Diseases, Brazzaville University Hospital
Department of Pneumology, University Hospital of Brazzaville
Department Cardiology Brazzaville University Hospital
Submission: August 28, 2018;Published: October 16, 2018
*Corresponding author: Ossibi Ibara Bienvenu Roland, Infectious Disease Unit, Brazzaville CHU, BP: 1846 Brazzaville, DR Congo
How to cite this article: Ossibi I B, Bemba E, Okemba O F, Adoua D T, Aloumba A, Ontsira N G, Sekangué O G, Angonga E M B, Ikama M . Causes of Death of Patients Living with HIV in the Section of Infectious Diseases at the University Hospital of Brazzaville. Ann Rev Resear. 2018; 4(1): 555630. DOI: 10.19080/ARR.2018.04.555630
Abstract
Goal
The purpose of the study is to describe the distribution of the causes of death of HIV-infected patients in the Infectious Diseases section at Brazzaville University Hospital.
Method
To carry out this study, we rely on retrospective and descriptive study on the causes of death of patients living with HIV admitted to the service between February 1 and July 31, 2017.
Results
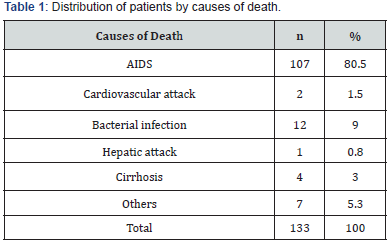
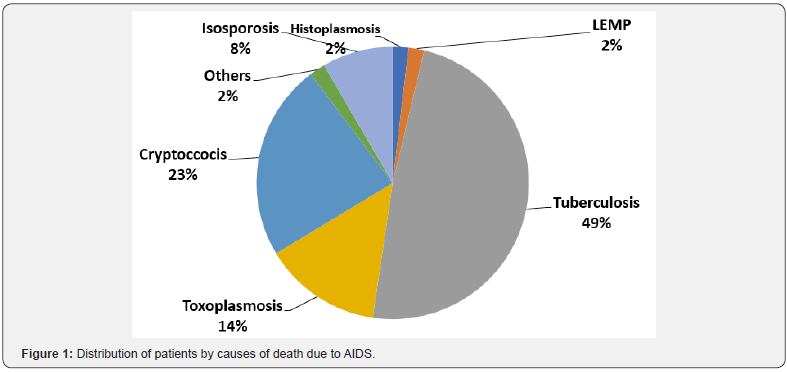
It comes out from analysis that the deceased were 40.2 ± 11.22 years old on average, mostly female (65.9%); 94% had been infected heterosexually, 53% were socio-economically vulnerable. The diagnosis of HIV infection was made within 46.1 ± 28.7 days on average and 25.6% had not received antiretroviral therapy. One hundred and thirty-three deaths have been reported. The leading causes of death were: AIDS (80.5%), bacterial infection (9.0%), cirrhosis (3.0%), cardiovascular disease (1.5%), liver injury (0.8%) and other causes (5.5%). For patients who died of AIDS, the most common pathologies involved were tuberculosis (48.6%), cryptococcosis (23.4%), toxoplasmosis (14.0%), isosporosis (8.4%), Histoplasmosis (1.9%), Leuco progressive multifocal encephalopathy (1.9%) and others (1.9%).
Conclusion
AIDS is the main cause of death of PLHIV in the Infectious Diseases section at the University Hospital of Brazzaville. In addition, there are socio-economic precariousness and the late detection of this affection. This is to say the interest of early detection and adequate and free care of opportunistic infections.
Keywords: HIV; Cause of death; AIDS; CHU and Brazzaville
Introduction
HIV infection is still a real public health problem because of its high morbidity and mortality especially in Africa [1]. The World Health Organization (WHO) estimated that there were 20 million people living with HIV (PLHIV) worldwide in 1995. Most PLHIV live in sub-Saharan Africa (22.4 million) [1]. Multiple antiretroviral therapies have significantly modified the prognosis of HIV since 1996 by a dramatic reduction in morbidity and mortality related to this epidemic [2]. These results were also found in sub-Saharan Africa, where the various series report a decrease in morbidity and mortality [3]. The number of PLHIV treated has been growing in sub-Saharan Africa since 2003 [3,4]. By the end of 2008, nearly 3 million people were on antiretrovirals in sub-Saharan Africa. Despite these advances, practitioners face several challenges in managing this condition, and among them: Late diagnosis of HIV infection and late initiation of treatment result in significant morbidity in the first 6-12months of treatment with the occurrence of AIDS-defining opportunistic infections [3,5].
In Congo Brazzaville, the prevalence of HIV infection increased from 4.1% in 2003 to 3.1% in 2009 [6,7] however, no data are available on the causes of death of PLHIV in the era of highly active antiretroviral therapy. This justifies the feasibility of this study whose general objective is the description of the distribution of causes of death among adults infected with HIV in the Infectious Diseases section at the Brazzaville University Hospital. As specific objectives, this study aims to describe the socio-demographic, clinical, and biological characteristics of hospitalized HIV-infected patients and compare patients on ARVs and non-ARVs; and finally estimate the hospital mortality rate, the factors associated with death.
Patients and Method
Type, period, setting
A retrospective and descriptive study of the causes of death of patients living with HIV admitted to the Infectious Diseases section between 1 February and 31 July 2017. Patients: Patients were at least 17 years old, HIV infected, regardless of type, admitted to hospital during the study period, diagnosed with HIV positive before or during hospitalization, whether or not receiving treatment were included ART. Study variables were epidemiological (age, sex, socio-occupational status, marital status, antecedents, risk factors for HIV infection), clinical (reason for consultation or admission, consultation time (time elapsed between the onset of illness and admission to hospital, WHO classification); paraclinical, namely CSF analysis (cytochemistry, direct examination after staining with Indian ink, cryptococcal antigen test, culture), Cryptococcal antigenemia, Sputum-BAAR, blood count, serum creatinine, HIV serology, LTCD4 level, load plasma viral and cerebral CT, Pulmonary X-ray.
Other variables were therapeutic (type of specific treatment and antiretroviral treatment) and progressive (length of hospital stay, initial causes of death and factors associated with death). Statistical analysis: the data were processed with the software EPI info 3.3.2 (CDC Atlanta, USA). Quantitative variables were represented in terms of mean ± standard deviation, and extremes in parentheses. The qualitative variables were represented in numbers and percentages. Comparisons of the qualitative variables used the chi-2 test, and for the quantitative variables the Student’s test. The significance level for comparisons was <0.05.
Results
Descriptive study
Fifty-seven patients were included (1.2% of admissions), with 87 women (69.5%). The sex ratio (M/F) was 1.93 (one man for every two women). The mean age was 40.2 ± 11.22 years (range 17 -72 years).
According to marital status, married couples were the most numerous (n = 84, 67.03%); 63 (29.58%) patients were single. The socio-professional status was represented by the unemployed (n = 25, 43.9%), the workers or craftsmen (n = 15, 26.3%), the traders (n = 14, 24.6%), the civil servants (n = 2, 3.5%) and retired (n = 1). The mode of transmission of HIV was heterosexual in 94%. The diagnosis of HIV infection was made within an average of 46.1 ± 28.7 days delay means of consultation was 29 days (extreme 3 and 60 days). The average CD4 count was 171.79 ± 88.93/mm3 (range: 1-459/mm3). The mean duration of hospitalization was 20.37 ± 11.8 days. Fifty-three percent (53%) of the deceased patients were socio-economically precarious and 25.6% of the deceased patients had not received antiretroviral therapy.
Causes of death
The cause of death was AIDS in 80.5% of cases (Table 1). Other causes of death were bacterial infection (n = 12, 9.0%), cirrhosis (n = 4, 3.0%), cardiovascular disease (n = 2, 1.5%), liver injury (n = 1, 0.8%) and other causes (n = 7, 5.5%). For patients who died of AIDS (n = 107), the most common pathologies involved were tuberculosis (49%), cryptococcosis (23%) toxoplasmosis (14%) isosporosis (8%), histoplasmosis (2%), Leuco progressive multifocal encephalopathy (2%) and others (1.9%) (Figure 1).
Analytical study
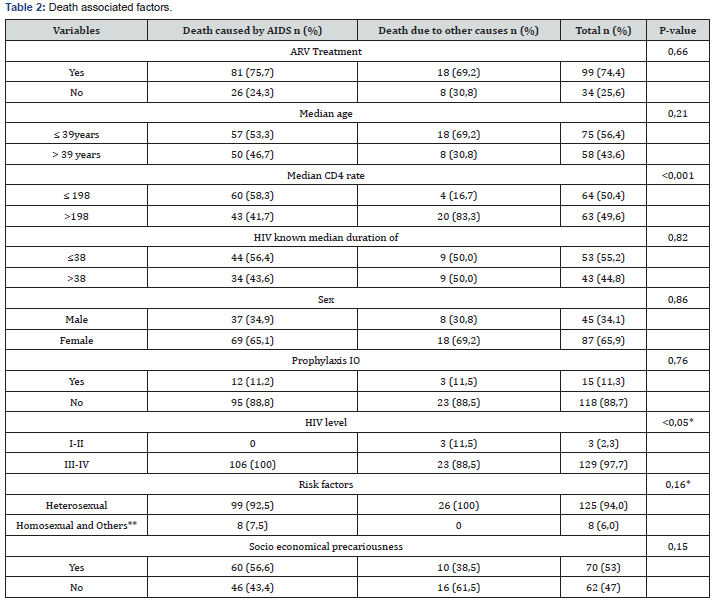
The lethality was 61.29%. It correlated with advanced immunosuppression with CD4 counts below 200/mm3 (Table 2).
Discussion
Young age subjects are the most affected in our study. They are mostly female and unemployed. This vulnerable population affected by HIV infection is the most sexually active and the heterosexual infection in sub-Saharan Africa is a reflection of the characteristics of the epidemic in this region. Several authors admit this [8]. The more or less long delay in the diagnosis of HIV infection in our patients is similar to what was found in the literature. The late diagnosis of HIV infection is also found in AIDS surveillance data in France where, in 2001, a new AIDS diagnosis was made simultaneously with the diagnosis of HIV status in half of the cases [9,10]. This is partly justified by the denial of the disease specific to the populations studied. Strategies for early detection of HIV infection as a complementary preventative measure should be emphasized in the response to this epidemic [10]. The majority of patients consulted late for advanced immunosuppression. More than half of the deceased patients were in socio-economic precarious situations as found in the African and European series [11]. It is therefore important to take this situation into account in the global care strategies of these poor patients, particularly in clinical services and in programs to fight against this condition. The long hospital stay in our patients as observed in the literature is due mainly to the fact that patients consult at an advanced stage of immunosuppression; this prolongs the duration of care, including that of opportunistic infections [12,13]. It is therefore necessary to promote the information, education and communication sessions related to this disease among the populations as a control strategy. More than a quarter of HIV-infected patients who died did not benefit from antiretroviral therapy. This finding corroborates that of several African authors [10]. The reasons for the lack of treatment are to be evaluated partly in the light of the sociocultural characteristics specific to the populations studied. AIDS remains the leading cause of most deaths of HIV-infected patients in our series. This finding, similar to that found in several African and Western series, suggests several reasons, including late detection of HIV infection, discovery at an advanced stage of the disease, resulting in the occurrence of opportunistic infections, poverty, and adequate management of this condition [10,13,14]. The advanced immunosuppression correlated with the numbers of T. CD4 lymphocytes had a statistically significant influence on the occurrence of death in our patients. This observation is similar to that of most African and Western authors [8,10,15]. High lethality is similar to that of low-income countries [10].
Tuberculosis was the leading cause of death in HIV patients followed by neuromeningeal cryptococcosis (Figure 1). In Congo, tuberculosis remains a major public health problem with an estimated prevalence of all cases at 449 per 100,000 population, the specific mortality rate is 69 per 100,000, and HIV seroprevalence among tuberculosis in 25% in 2005 [16]. Tuberculosis is responsible for more than 21% of deaths 30% of people living with HIV and 30% of tuberculosis HIV co-infections die [15]. We are reintroducing into the scientific field a therapeutic debate on the discussion of the interest of the introduction of the primary prophylaxis of tuberculosis in very immunocompromised patients [8]. The high prevalence of cryptococcosis is due in part to the exposure of immunocompromised patients to the predisposing factors found in our series such as house dust, pigeon droppings and even bat guanos [17- 19].
Conclusion
Our study confirms the idea that AIDS remains the leading cause of death of PLHIV in patients with socio-economic insecurity. In this regards, it is worthwhile strengthening the strategies for the prevention and management of opportunistic infections.
References
- UNAIDS WHO AIDS epidemic update (2009).
- CASCADE collaboration. Determinants of survival following HIV- 1 seroconversion after the introduction of HAART. Lancet 2003 362(9392): 1267-1274.
- Braitstein P, Brinkhof MW, Dabis F, Schechter M, Boulle A, et al. (2006) Mortality of HIV-1 infected patients in the first year of antiretroviral therapy: Comparison between low-income and high-income countries. Lancet 367(9513): 817-824.
- Seyler C, Messou E, Gabillard D, Inwoley A, Alioum A, et al. (2007) Morbidity before and after HAART initiation in sub-Saharan African HIV-infected adults: a recurrent event analysis. AIDS Res Hum Retroviruses 23(11): 1338-1347.
- Moh R, Danel C, Messou E, Ouassa T, Gabillard D, et al. (2007) Incidence and determinants of mortality and morbidity following early antiretroviral therapy initiation in HIV-infected adults in west Africa. AIDS 21(18): 2483-2491.
- National Center for Statistics and Economic Studies (CNSEE) and Center for Research and Study in Development in Public Health (CREDES) 2004. National Assessment of the Seroprevalence of HIV Infections and Syphilis. Paris: CREDES.
- National Center for Statistics and Economic Studies (CNSEE) and ICF Macro (2009) Seroprevalence and Indicators Survey of AIDS-Congo.
- Lewdnen C, Sobesky M, Cabio A Causes of death of HIV-infected adults in the French departments of America in the era of highly active antiretroviral therapy.
- Institute of Health Watch (2002) Surveillance of AIDS in France as of March 31, 2002. Bull epidemiol Hebd pp. 133-139.
- Manga NM, Diop SA, Dour CTN (1993) Late detection of HIV infection at the Fann Infectious Disease Clinic, Dakar: Diagnosis Circumstances, Therapeutic Patient Route and Determinants. Bulletin of the exotic pathology society 86(5): 351-357.
- Zaba B, Whiteside A, Boerma JT (2004) Demographic and socioeconomic impact of AIDS: taking stock of the empirical evidence. Aids 18(2): S1-S7.
- Oumar AA, Dao S, Diallo S et al. (2008) Prevalence of opportunistic infections during AIDS in hospital in Bamako, Mali. Louvain Med 127(1): 12-17.
- Ouedraogo SM, Ouedraogo M, Dagnan NS, Adom AH (2007) Opportunistic infection during AIDS at the CHU Treichville. Mali Med 22(1): 26-8.
- Okome Nkoumou M, Boguikouma JB, Kombila M (2006) Opportunistic diseases of HIV infection at the Jeanne Ebori Foundation Hospital in Libreville, Gabon. Med Trop 66(2): 167-171.
- Lawn SD, Harries AD, Anglarete X, Myer L, Wood R (2008) Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS 2008 22(15): 1897-1908.
- WHO (2007) Global Tuberculosis Control: Surveillance, Planing, Financing.
- Bissagnené E, Ouhon J, Kra O, Kadio A (1994) Current aspects of neuromeningeal cryptococcosis in Abidjan. Med Mal Infect 24: S580-S585.
- Aoussi EF, Ehui E, Dembélé JP (2012) Cryptococcal neuro-meningeal and HIV the era of antiretrovirals in Ivory Coast. Med Mal 33: 1-6.
- Soumare M, Seydi M, Ndour CT (2005) Current aspects of neuromeningeal cryptococcosis in Dakar. Med Trop 65: 559-562.






























