Evaluating the Clinical Utility of Testing for Autoimmune Disorders in the Setting of Leukopenia/Neutropenia in an Ambulatory Hematology Clinic
Devin Malik1*, Joyce Philip2, Amal Hejab2, Alexander Horbal2, Vivek Mendiratta2 and Philip Kuriakose1
1Division of Hematology and Oncology, Henry Ford Hospital & Wayne State University, USA
2Department of Internal Medicine, Henry Ford Hospital & Wayne State University, USA
Submission: June 14, 2018; Published: August 27, 2018
*Corresponding author: Devin Malik, Division of Hematology and Oncology, Henry Ford Hospital & Wayne State University, 2799 W Grand Blvd, Detroit MI 48202, USA, Tel: 313-850-9337; Email: dmalik1@hfhs.org
How to cite this article: Devin M, Joyce P, Amal H, Alexander H, Vivek M, et.al. Evaluating the Clinical Utility of Testing for Autoimmune Disorders in the Setting of Leukopenia/Neutropenia in an Ambulatory Hematology Clinic. Ann Rev Resear. 2018; 3(2): 555610. DOI: 10.19080/ARR.2018.03.555610
Abstract
Purpose: To determine how many patients seen in our hematology clinic for leukopenia and screened for autoimmunity are being diagnosed with autoimmune conditions.
Methods:This was a retrospective, single institution study done in an ambulatory clinic setting. Data was collected from 2005-2015. Inclusion criteria were having a white blood cell count of less than 3.8K/uL or neutrophil count less than 1.8K/ul and positive antinuclear antibody (ANA) or rheumatoid factor antibody (RF) of greater than 1:80 or 14IU/mL, respectively (institutional cutoffs). Exclusion criteria were a known hematologic disorder, rheumatologic disorder or active chemotherapy
Results:One hundred and ninety-one patients were reviewed for data analysis. Eleven patients were diagnosed with rheumatologic conditions (6%). The majority of these patients had associated findings suggestive of an underlying autoimmune disease.
Conclusions:This study shows that testing for ANA and RF in patients with leukopenia/neutropenia is of limited clinical utility in asymptomatic patients with no other lab abnormalities, and as such it should not be part of a routine work up, unless directed by symptoms.
Keywords: Hematologic disorder; Rheumatologic conditions; Active chemotherapy; Autoimmune disease; Leukopenia; Neutropenia
Introduction
Leukopenia (WBC count of <3.8K/uL) and/or neutropenia (<1.8K/uL, both institutional lab cutoffs), are commonly encountered by physicians on routine blood testing in otherwise healthy patients. This finding, whether incidental or not, often leads to hematology referrals. A broad work up may be pursued in an attempt to find a definitive diagnosis. We conducted this study to assess the utility of testing for anti-nuclear antibody (ANA) as well rheumatoid factor (RF) in patients with leukopenia/neutropenia, and whether or not a positive serology led to a rheumatologic diagnosis.
Methods
After obtaining institutional review board approval, we searched for outpatient hematology consults with a diagnosis of leukopenia and/or neutropenia using ICD-9 and ICD-10 diagnostic codes between 2005-2015 at Henry Ford Hospital. Data points included demographics and antibody serology. Physician documentation was reviewed for additional symptoms such as joint/muscle pain. Patients were excluded if they had a known hematologic disorder, known rheumatologic disorder or were on active chemotherapy. A positive ANA or RF were considered if titers were >1:80 or >14IU/mL (institutional cutoffs). Complete blood counts were reviewed for patients who were not excluded based on above criteria.
Results
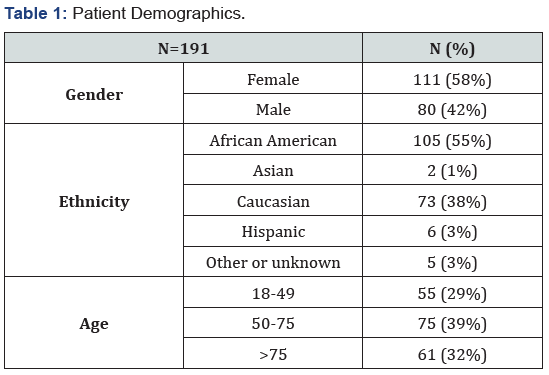
A total of 561 patients were seen in our outpatient clinic during the 10-year interval with an associated diagnostic code for leukopenia/neutropenia. One hundred and ninety-nine were excluded due to incomplete data or inadequate follow up period, 35 patients for known malignancy, 14 for known rheumatologic disorder, and 122 for being on active chemotherapy. The remaining 191 patients were reviewed for data analysis. Patient demographics are summarized in Table 1.
A total of 116 patients (61%) were tested for ANA, of which 27 (23%) were positive. Twenty two of those 27 (81%) patients were referred to rheumatology, 6 of whom were diagnosed with rheumatologic diseases (22%). RF was tested in 110 patients (58%), of which 15 were positive (14%); all were referred to rheumatology, with 5(42%) being diagnosed with rheumatologic diseases. Test results, referral rate and rheumatologic diagnosis are listed in Table 2.
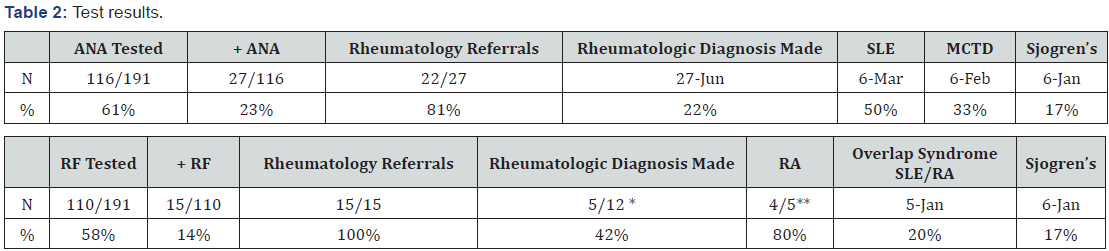
*3 patients were no shows. ** 1 patient developed T-LGL
SLE-systemic lupus erythematosus, MCTD-mixed connective tissue disease.
The majority of patients who were diagnosed with rheumatologic disorders had associated findings suggestive of underlying disease - 3 patients with systemic lupus erythematosus (SLE) had mild thrombocytopenia (100-150K/uL), 1 patient with mixed connective tissue disease had Raynaud’s phenomenon, 3 patients with rheumatoid arthritis (RA) had arthralgias and 1 had myalgias, all with correlating physical exam or radiographic findings.
Other alternative diagnoses for leukopenia/neutropenia included drug induced, viral and bacterial infections, hematologic malignancies, ethnic neutropenia, transient leukopenia, and idiopathic.
Discussion
Leukopenia can be the result of a primary bone marrow disorder (myelodysplastic syndrome, myelofibrosis, leukemia) or a secondary phenomenon as a result of drugs, infection, and autoimmunity, amongst others. Autoimmune neutropenia can be primary, occurring in infancy, or secondary in the context of an autoimmune disorder which usually manifests in adulthood [1]. The strongest autoimmune association can be made for large granular lymphocytic leukemia (LGL) and Felty’s syndrome with rheumatoid arthritis. While the former’s mechanism in causing neutropenia is unclear, the latter is related to humoral immunity with antineutrophilic antibodies, although testing for these antibodies may be unhelpful in diagnosis [2,3]. The treatment of neutropenia in LGL is with low doses of methotrexate or cyclophosphamide [4,5], while in Felty’s syndrome treatment of the underlying RA is often sufficient [6].
The mechanism of neutropenia in SLE is multifactorial, including increased neutrophil apoptosis, antineutrophilic antibodies, and bone marrow dysfunction from antibodies towards hematopoietic stem cells [7-10]. The degree of neutropenia often mirrors disease activity and most often responds to immune suppression. Other connective tissue diseases have a similar pathophysiology to SLE.
Conclusion
Ambulatory hematology consults for leukopenia/neutropenia are a common occurrence in practice. Our study showed that 11 patients out of 191 (6%) were found to have an associated rheumatologic disorder, with the majority having other signs/ symptoms or associated lab abnormalities suggestive of autoimmune disease. This study shows that testing for ANA and RF in patients with leukopenia/neutropenia is of limited clinical utility in asymptomatic patients with no other lab abnormalities, and it should not be part of a routine work up, unless directed by symptoms. Primary care providers need to screen for other abnormalities (symptoms/clinical findings) in order to identify patients that would benefit most from subspecialty referral.
References
- Bux J, Behrens G, Jaeger G, Welte K (1998) Diagnosis and clinical course of autoimmune neutropenia in infancy: analysis of 240 cases. Blood 91(1): 181-186.
- Breedveld FC, Lafeber GJ, de Vries E, van Krieken JH, Cats A (1986) Immune complexes and the pathogenesis of neutropenia in Felty’s syndrome. Ann Rheum Dis 45(8): 696-702.
- Starkebaum G, Loughran TP Jr, Gaur LK, Davies P, Nepom BS (1997) Immunogenetic similarities between patients with Felty’s syndrome and those with clonal expansions of large granular lymphocytes in rheumatoid arthritis. Arthritis Rheum 40(4): 624-626.
- Loughran TP, Kidd PG, Starkebaum G (1994) Treatment of large granular lymphocyte leukemia with oral low-dose methotrexate. Blood 84(7): 2164-2170.
- Moignet A, Hasanali Z, Zambello R, Pavan L, Bareau B, et al. (2014) Cyclophosphamide as a first-line therapy in LGL leukemia. Leukemia 28(5): 1134-1136.
- Narvaez J, Domingo-Domenech E, Gomez-Vaquero C, López-Vives L, Estrada P, et al. (2012) Biological agents in the management of Felty’s syndrome: a systematic review. Seminars in arthritis and rheumatism 41(5): 658-668.
- Starkebaum G (2002) Chronic neutropenia associated with autoimmune disease. Semin Hematol 39(2): 121-127.
- Starkebaum G, Arend WP (1979) Neutrophil-binding immunoglobulin G in systemic lupus erythematosus. J Clin Invest 64(4): 902-912.
- Courtney PA, Crockard AD, Williamson K, Irvine AE, Kennedy RJ, et al. (1999) Increased apoptotic peripheral blood neutrophils in systemic lupus erythematosus: Relations with disease activity, antibodies to double stranded DNA, and neutropenia. Ann Rheum Dis 58(5): 309- 314.
- Liu H, Ozaki K, Matsuzaki Y, Abe M, Kosaka M, et al. (1995) Suppression of haematopoiesis by IgG autoantibodies from patients with systemic lupus erythematosus (SLE). Clin Exp Immunol 100(3): 480-485.






























