A Rare Case of Pediatric Gallbladder Volvulus
Bisma Badr MD*, Katherine Davenport MD, Jamie Golden MD, Atay Orhan MD and Sameer Lapsia MD
Department of Pediatrics, Children’s Hospital of the Kings Daughters, 601, Children’s Lane, Norfolk, Virginia, USA
Submission:April 10, 2024;Published:April 22, 2024
*Corresponding author:Bisma Badr, Department of Pediatrics, Children’s Hospital of the Kings Daughters, 601, Children’s Lane, Norfolk, Virginia, USA
How to cite this article:Bisma Badr MD*, Katherine Davenport MD, Jamie Golden MD, Atay Orhan MD and Sameer Lapsia MD. A Rare Case of Pediatric Gallbladder Volvulus. Adv Res Gastroentero Hepatol, 2024; 20(3): 556040.DOI:10.19080/ARGH.2024.20.556040.
Abstract
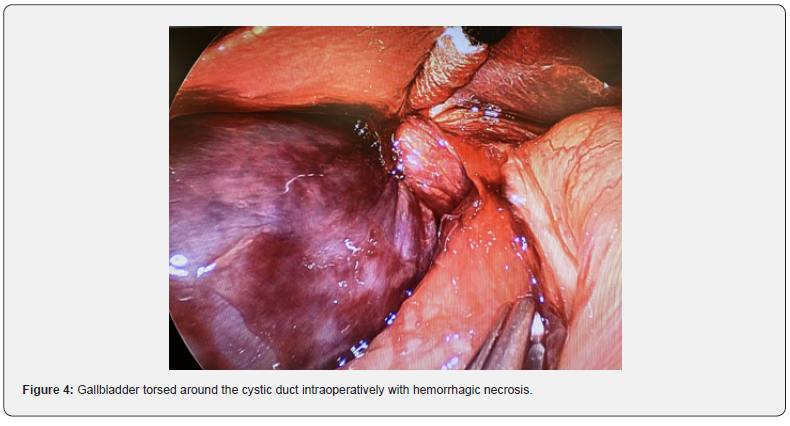
Gallbladder torsion is a rare, acute abdominal disease first reported by Wendell in 1898 [1] which predominantly affects women, with the median age of presentation being 77 years [2]. It occurs as a result of rotation of the gallbladder along the axis of the cystic duct and its vascular pedicle. In this case, we describe a 16-year old male who was diagnosed with acalculous cholecystitis on the basis of clinical history, labs, and radiographic findings but was found to have acute gallbladder volvulus requiring cholecystectomy. Lab findings were remarkable for elevated total bilirubin and CRP, while exam findings were notable for fever, scleral icterus, and RUQ pain. Radiological exams prompting the diagnosis included Abdominal X-ray, CT Chest/abdomen/ pelvis, RUQ ultrasound, and HIDA scan. Patient was taken to the OR where an ischemic, torsed gallbladder was identified and removed. Pathology report of the gallbladder tissue showed diffuse hemorrhagic necrosis, consistent with the clinical history of gallbladder torsion. This case highlights the importance of including gallbladder torsion in the differential diagnosis for a patient with uncertain clinical, lab and radiographic findings. Even though the diagnosis of gallbladder torsion is extremely rare in the pediatric population, delay in diagnosis and treatment can lead to morbidity and mortality in this population. Radiographic findings most specific to gallbladder volvulus include ultrasonography or CT showing a markedly enlarged “floating” gallbladder with a continuous hypoechoic line indicating edematous change in the wall. The diagnosis is usually confirmed intraoperatively, and laparoscopic cholecystectomy is the gold standard treatment.
Keywords: Pediatric Gallbladder Volvulus; Ultrasonography; Cholecystectomy; Acalculous cholecystitis
Abbreviations:RUQ: Right upper quadrant; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; MRCP: Magnetic Resonance Cholangio Pancreatography; HIDA: Hepatobiliary Iminodiacetic Acid; NPO: Nothing Per Oral
Introduction
Gallbladder volvulus is an extremely rare disease, with the peak incidence being one in every 350, 000 hospital admissions [1]. It peaks in two age groups, an elderly patient group aged > 70 years old and a pediatric patient group aged <18 years old, with a higher incidence in the older population [2, 3]. Among the older population, females are more predominant with a 3:1 ratio whereas in the pediatric population, males are more predominant with a 9:1 ratio [2,3]. The etiology of gallbladder torsion is complex and thought to be related to an abnormally long mesentery or a loss of visceral fat with both resulting in twisting along the axis of the cystic duct and artery [4,5]. Signs and symptoms are nonspecific and resemble cholecystitis but can be present without gallstone disease and does not respond to antibiotics [3,6]. With the exception of MRCP, imaging studies can also be nonspecific making the preoperative diagnosis of gallbladder volvulus difficult [7]. Despite these challenges, the gold standard for treatment of gallbladder volvulus is urgent laparoscopic cholecystectomy. Delay in the treatment can increase morbidity and mortality due to infarction, necrosis, perforation, and bilious peritonitis. The overall morbidity and mortality rate of gallbladder volvulus is reported to be 16% and 6% respectively [3].
Case Report
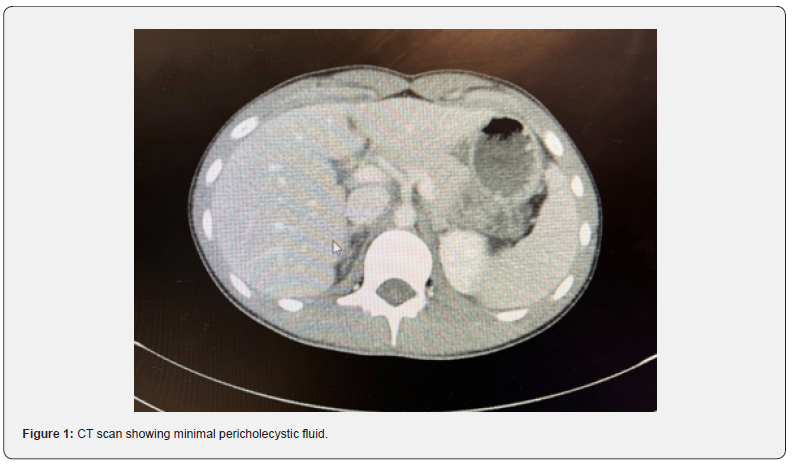
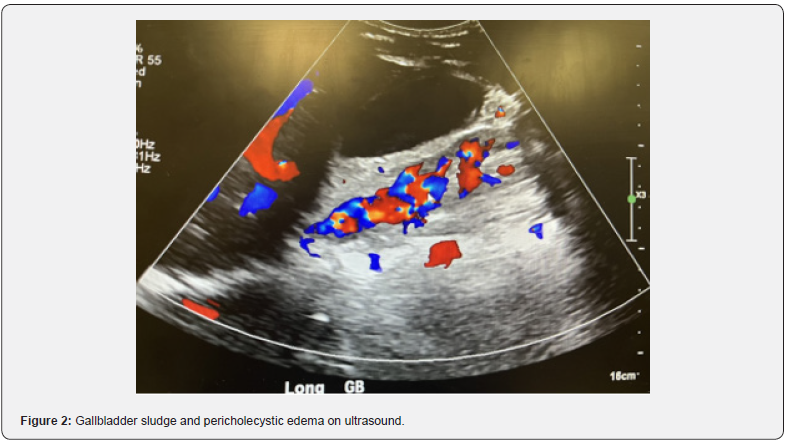
A 15-year-old male with no significant past medical history presented to the Emergency Department (ED) with right upper quadrant pain, nausea, vomiting, and decreased appetite evolving over a duration of 48 hours. On initial presentation, his work-up was remarkable for an elevated total bilirubin of 1.9, unremarkable CBC, and an x-ray showing subtle nodularity in the right colon indicative of possible colitis. Ultrasound was performed and the appendix was not visualized. He was discharged home from the ED with Toradol and Zofran for pain and nausea. He returned the next day with worsening right upper quadrant pain and fever (103 Fahrenheit). His nausea and vomiting had improved, but he continued to have a decrease in appetite. On examination, he was febrile, tachycardic, tachypneic, tender to palpation in the right upper quadrant area, had a negative Murphy’s sign and was jaundiced. Laboratory testing was repeated which showed an increasing total bilirubin from 1.9 to 3.7, mildly elevated ALT of 35, and elevated CRP of 8.5. CBC was unremarkable for leukocytosis, anemia or thrombocytosis. Computed Tomography (CT scan) of the abdomen and pelvis was performed which showed a normal appendix, massive stool burden in the cecum, possible sludge/ stones in the gallbladder with minimal pericholecystic fluid around the tip of the fundus and tip of the liver, with an inability to rule out cholecystitis and a horseshoe kidney with a dilated left renal pelvis (Figure 1). He was given 2 bisacodyl enemas which did improve his pain. A right upper quadrant ultrasound (RUQ) was performed showing gallbladder sludge and pericholecystic edema concerning for acalculous cholecystitis (Figure 2).
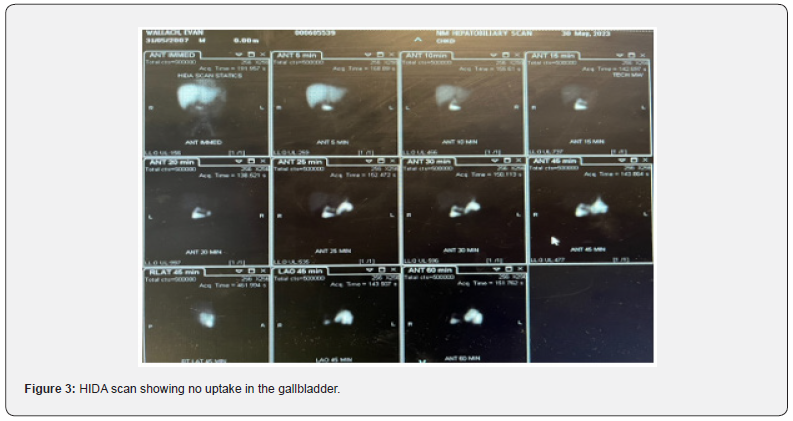
He was admitted, made nothing per oral (NPO), started on IV piperacillin-tazobactam and IV Tylenol. Hepatobiliary Iminodiacetic Acid (HIDA) Scan was performed demonstrating no filling of the gallbladder with patent common bile duct and normal liver function, concerning for cystic duct obstruction (Figure 3). His labs showed a downward trend in the total bilirubin with insignificant direct bilirubin of 0.0, and an upward trend in CRP, with the highest CRP being reported at 16.8 (on the day of surgery). He was not improving on antibiotics so on hospital day 4, he was taken to the operating room for laparoscopic cholecystectomy where the gallbladder was found to be torsed along the cystic duct (Figure 4). The gallbladder appeared distended with hemorrhagic necrosis. It was needle aspirated, detorsed, and removed. Pathology was consistent with ischemia and hemorrhagic necrosis. Postoperatively, he remained afebrile and was eating well without pain. He was discharged home on post-operative day [1].
Discussion
Gallbladder volvulus is an extremely rare diagnosis, with only around 300 cases reported to date, with 50 reported in the pediatric population [8]. Discovered first by Wendell in 1898, gallbladder volvulus remains one of the most challenging preoperative diagnoses [9]. Only 10% of the patients with gallbladder volvulus have the correct preoperative diagnosis, with the vast majority being diagnosed during cholecystectomy. The etiology of gallbladder torsion is complex and difficult to ascertain. Different hypotheses have been proposed for different population groups. Among the pediatric population, gallbladder torsion is most likely to be a result of an abnormally long mesentery extending from the gallbladder to the liver bed or a result of an anatomic abnormality of the vascular pedicle making the gallbladder float and susceptible to torsion along the axis of the cystic duct and artery. On the other hand, among the elderly population, the loss of visceral fat associated with the process of aging could be a contributing factor predisposing the elderly population to gallbladder torsion [5, 6]. Gallbladder volvulus is a life-threatening condition with most cases diagnosed intraoperatively only. Diagnostic signs and symptoms of gallbladder volvulus are very nonspecific. Right upper quadrant abdominal pain, nausea and vomiting, symptoms resembling cholecystitis, along with a palpable abdominal mass in right upper quadrant are some of the signs and symptoms commonly reported by patients [9, 10]. Index of suspicion is high in those cases of presumed cholecystitis, not responding to antibiotics, specifically in the absence of gallstone disease [3].
Because these symptoms resemble cholecystitis, gallbladder volvulus is often misdiagnosed. RUQ ultrasound, CT scan of the abdomen, Magnetic Resonance Imaging (MRI), Magnetic Resonance Cholangio Pancreatography (MRCP) and HIDA scan are some forms of radiological imaging used to help diagnose gallbladder volvulus, with MRCP taking precedence over the others due to its ability to visualize the cystic duct [11]. MRCP findings that are characteristic of gallbladder volvulus include tapering and twisting interruption of the cystic duct, V shaped distortion of the extrahepatic bile duct, a distended gallbladder and representation of different intensities in extrahepatic bile ducts, cystic duct, and the gallbladder [3]. MRI can be diagnostic of necrosis and hemorrhage, with the presence of high signal intensity within the gallbladder wall [4]. Abdominal ultrasound is remarkable for gallbladder wall thickening, similar in presentation to acute cholecystitis, along with positioning of the gallbladder outside the fossa, inferior to the liver with attachment to the liver via a conical structure consistent with the twisted pedicle [3]. CT scan findings are also nonspecific, showing gallbladder wall inflammation, abrupt tapering of the cystic duct, collection in the gallbladder fossa, positioning of the gallbladder outside of its fossa, vertical to horizontal rotation of the gallbladder’s axis, and a twist along the gallbladder’s vascular pedicle with swirled appearance [12]. HIDA scan can sometimes show radioactive tracer deposition within the gallbladder, mimicking a bull’s-eye appearance [13].
In our case, the patient had all the signs and symptoms listed above except a positive Murphy’s sign and palpable RUQ abdominal mass. Moreover, MRCP was not performed prior to cholecystectomy and the patient was taken to the operating room with a presumed diagnosis of cholecystitis based on his failure to improve on antibiotics. Interestingly, clinical presentation of gallbladder volvulus can be divided into 3 triads: a triad of symptoms consisting of short history, early, acute onset of vomiting, and typical abdominal pain; a triad of physical signs consisting of palpation of an abdominal mass, absence of toxemia/jaundice and disparity between pulse and temperature; and a triad of patient’s characteristics consisting of a thin, older patient, patient with chronic chest disease, or a patient with spinal deformities [14]. In the presence of such nonspecific signs, symptoms and radiological findings, preoperative diagnosis of gallbladder volvulus is difficult and occurs in 25% of the patients eventually diagnosed with gallbladder volvulus on laparoscopic cholecystectomy [3]. With most gallbladder volvulus cases misdiagnosed as cholecystitis, the major dilemma occurs when its treatment is delayed. Ischemia and necrosis of the gallbladder, if not treated emergently can lead to gangrene, perforation, biliary peritonitis, multiorgan failure, and death [3,14]. Prompt diagnosis and treatment of gallbladder volvulus is difficult but critical and should remain in the differential to avoid delay of potentially lifesaving treatment [15,16].
Conclusion
In conclusion, gallbladder volvulus is an extremely rare condition, especially in pediatric patients. In light of non-specific signs, symptoms and radiological findings, preoperative diagnosis becomes a challenge. However, due to the high morbidity and mortality associated with delayed diagnosis and misdiagnosis, index of suspicion should be high in all cases of acalculous cholecystitis which do not respond to antibiotics and conventional treatment. MRCP is the best diagnostic tool, so far, which can aid in the diagnosis of gallbladder volvulus. Once diagnosis is made, measures should be taken to perform laparoscopic cholecystectomy urgently to prevent clinical complications of gangrene, perforation, peritonitis, and death.
References
- Moser L, Joliat GR, Tabrizian P (2021) Gallbladder volvulus. Hepatobiliary Surg Nutr 10(2): 249-253.
- Gupta V, Singh V, Sewkani A, Purohit D, Varshney R (2009) Torsion of gall bladder, a rare entity: a case report and review article. Cases J 2(1): 1-3
- Keeratibharat N, Chansangrat J (2022) Gallbladder Volvulus: A Review. Cureus 14(3): e23362.
- Abadía-Barnó P, Coll-Sastre M, Picón-Serrano C, Sanjuanbenito-Dehesa A, Cabañas-Montero J (2016) Gallbladder volvulus: Diagnostic and surgical challenges. Cir cir 10(85): 89-92.
- Musthafa S, Aftab Z, Ali SM, Khanna M (2018) Gallbladder volvulus with segmental right liver lobe hypoplasia/atrophy: a preoperative diagnostic dilemma. BMJ Case Rep.
- Nho WY, Kim JK, Kee SK (2021) A comparative analysis of gallbladder torsion and acute gallbladder disease without torsion: a single-center retrospective case series study. Annals of Translational Medicine 9(18).
- Matsuhashi N, Satake S, Yawata K, Asakawa E, Mizoguchi T, et al. (2006) Volvulus of the gall bladder diagnosed by ultrasonography, computed tomography, coronal magnetic resonance imaging and magnetic resonance cholangio-pancreatography. World journal of gastroenterology: World JGastroenterol 12(28): 4599.
- Daly T, Byrne J, Aftab F (2023) Gallbladder torsion with gangrenous cholecystitis: a case report. Journal of Surgical Case Reports (5): rjad252.
- Kashyap S, Mathew G, Abdul W, Ahmad H (2020) Gallbladder volvulus. StatPearls.
- Abou Sleiman C, Terro JJ, Semaan DB (2019) Gallbladder Volvulus: An Unusual Presentation. Am J Case Rep 20: 1879-1882.
- Beatty AS, Kulendran K, Iswariah H, Chandrasegaram MD (2023) Gallbladder volvulus with preoperative and intraoperative imaging. J Surg Case Rep 2: rjad048.
- Layton B, Rudralingam V, Lamb R (2016) Gallbladder volvulus: it’sa small whirl. BJR| case rep 23: 20150360.
- Baig Z, Ljubojevic V, Christian F (2021) The diagnostic dilemma of a gallbladder volvulus: an unusual case report and review of the literature. Int J Surg Case Rep 80: 105614.
- Kavina S, Doruk S, Crawford M, Watson G (2023) Gallbladder Volvulus in an Elderly Female With Severe Kyphoscoliosis. Cureus 15(3): e36256.
- Borde P, Vilgrain V (2021) Gallbladder volvulus. Radiology 301(1): 43.
- Abdelrahman ZA, Omar RM, Mirza S, Türkmen S (2022) Gallbladder volvulus. Clinical Case Reports 10(4): e05549.






























