Unusual Case of Acute Recurrent Pancreatitis in an Adolescent; A Case Report
Khaled Matar1*, Iyad Abo Jazr1, Mohammed Hejazi1, Ibrahim AboZeid2, Salah Al Shami2, Mahmoud Al SheikhAli2, Hassan Rosros1, Rami Salut2, Iyad Khamaysi3, Marwan Matar4, Mousa Alnahhal4, Deema Naim5, Emad Al Hout6 and Ayman Abu Helal7
1Gastroenterology Department, European Gaza Hospital, Palestine
2Internal Medicine department, European Gaza Hospital, Palestine
3The Ruth and Bruce Rappaport Faculty of Medicine, Technion Institute of Technology, Israel
4Radiology and medical imaging Department, European Gaza Hospital, Palestine
5Palestine University, Al Azhar Medical faculty, Palestine
6Department of General Surgery, European Gaza Hospital, Palestine
7Jordan University Hospital-Rheumatology Department, Jordan
Submission:August 01, 2023; Published:August 22, 2023
*Corresponding author: Khaled Matar, Gastroenterology Department, European Gaza Hospital, Palestine, Email: aboayman2001@hotmail.com
How to cite this article: Khaled M, Iyad Abo J, Mohammed H, Ibrahim A, Salah Al Shami, et al. Unusual Case of Acute Recurrent Pancreatitis in an Adolescent; A Case Report. Adv Res Gastroentero Hepatol, 2023; 20(1): 556026. DOI: 10.19080/ARGH.2023.20.556026.
Abstract
Background: Ascariasis is the most common helminthic infection. It is most common in children of tropical and developing countries where the transmission is by contamination of soil by human feces or use of untreated feces as fertilizer. Transmission in most endemic areas is via person-to-person contact. We hereby present a case report of acute pancreatitis due to ascariasis. 17 years old male patient with no chronic medical illness presented to ER. complaining of epigastric pain, constant radiating to the back for 5 days duration associated with non-projectile non-bloody vomiting, gradual in onset and progressive in course. The laboratory investigation showed high amylase, Probable diagnosis of acute pancreatitis was made. He was managed symptomatically with intravenous fluids, analgesics, anti-emetics and enteral nutrition. However, the cause remained undetermined as we ruled out the possible etiologies of acute pancreatitis until MRCP was done and showed filling defect in distal pancreatic duct and dilated pancreatic duct. Repeated ultrasound was done which showed ascaris in pancreatic duct. This is one of the first few case reports of ascariasis-induced pancreatitis from Pakistan and the first one from Gaza strip of Palestine. Thus, it highlights ascariasis as possible etiology of acute pancreatitis in regions where ascariasis is geographically endemic.
Keywords: Ascariasis; Acute pancreatitis; Palestine; Ascariasis-induced pancreatitis
Introduction
Ascaris lumbricoides is the largest intestinal nematode (roundworm) parasitizing the human intestine and is one of the most common helminthic human infections worldwide [1]. Transmission of ascariasis occurs primarily via ingestion of water or food contaminated with Ascaris eggs. Most patients with A. lumbricoides infection are asymptomatic. When symptoms do occur, they occur most often during the adult worm intestinal stage (as intestinal, hepatobiliary, or pancreatic manifestations) but may also occur during the larval migration stage (as pulmonary manifestations) [2,3].
The helminthic illness known as Ascaris lumbricoides is quite widespread. An estimated 1.2–2 million instances of clinical illness and almost 20,000 fatalities occur year [1]. The global prevalence is 25%, with an estimated 1.4 billion persons affected. This is most common in the tropics and subtropics, where sanitation is inadequate, and temperatures and humidity levels are high. The peak age for infection is between 2 and 10 years old, and the rate of infection drops down significantly after the age of 15 years. Ingestion of eggs from tainted animal products, plant matter, or water initiates the life cycle. The liver receives nutrients through portal and systemic circulation from the duodenum, where the larvae hatch. Next, they go via the trachea and bronchi to the alveoli. Here they molt into adult worms after being ingested [1]. Specifically, the roundworms are actively motile, have wandering nature, and can migrate from their natural habitat in the duodenum and proximal jejunum into the ampulla of Vater and enter the bile duct or pancreatic duct, causing cholangitis or pancreatitis, respectively [2]. The severity of the clinical manifestations depends on the afflicted body part. Those with a high ascarides load may have “cough, ascariasis pneumonia, status asthmaticus requiring ICU admission, nausea, vomiting, hepatobiliary and intestinal obstruction, stunting of growth, cognitive dysfunction, and malnutrition” [1].
Acute pancreatitis may be caused by a number of different things, including alcoholism and gallstones, but also trauma, post-ERCP complications, certain drugs, hypercalcemia, hypertriglyceridemia, and viral causes [3]. Here, we report an unusual case of acute pancreatitis due to A. lumbricoides infestation.
Case Presentation
According to the patient, he developed pain in the epigastric region for 5 days. The pain was sudden in onset, sharp and severe in intensity, radiating towards the back, aggravated by taking meal and had no relieving factor. The pain was associated with vomiting since day one, sudden in onset, 4-5 episodes per day which were non-projectile, non-bilious, watery in consistency, and did not contain any blood. Vomiting was aggravated by taking meal.
There was not any history of associated sore throat, ear or nasal discharge, chest pain, cough, diarrhea, constipation, burning micturition, rashes, joint pain, weight loss, insect or mosquito bite. Review of the systems was thus non-significant. He had no past medical history of diabetes mellitus, ischemic heart disease, lipid profile abnormalities, tuberculosis or rheumatic disease. The patient had no blood transfusion history, no food or drug allergies. His family history was non-significant. His bowel habits were normal. He gave no history of smoking, alcohol intake, or drug addiction. He belonged to the lower socioeconomic class. On presentation, the patient was in pain, had no jaundice or pallor, well oriented to time, place, person, with normal range vital signs. Upon physical examination, abdomen had normal shape and symmetry, no scar marks, dilated veins, bruises or rashes. Upon palpation there was marked tenderness on superficial and deep palpation in the epigastric. No rigidity, shifting dullness, fluid thrill or visceromegaly were appreciated. Bowel sounds were audible in all four quadrants upon auscultation. Upon inspection, the chest was of normal shape and symmetry. No deformity, scar marks, bruises or rashes were observed. Chest expansion was normal and symmetrical bilaterally. There was no tenderness upon palpation and vocal fremitus was normal. Percussion was tympanic with no hyper resonance or dullness. Upon auscultation he had normal vesicular breathing, no wheeze or crepitations were heard. Cardio-vascular, neurological and musculoskeletal examinations were non-significant and revealed no abnormalities. No lymphadenopathy was appreciated. Probable differential diagnosis of gastritis, pancreatitis and cholecystitis was made.
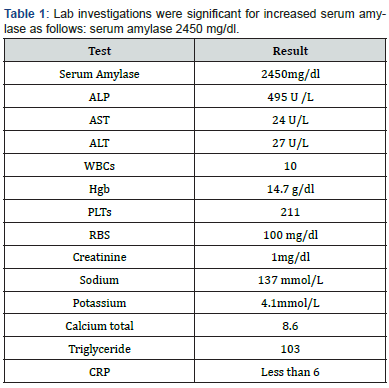
Lab investigations were significant for increased serum amylase as follows: serum amylase 2450 mg/dl; (Table 1). Abdominal ultrasound was done and showed normal study of liver, CBD diameter, gallbladder, kidneys, spleen, and urinary bladder, MRCP was done and showed filling defect in distal pancreatic duct measured about 1cm x 8cm and dilated pancreatic duct, Repeated ultrasound after MRCP showed hypoechoic tubular structure with well-defined echogenic walls (Figure 1).

The patient was managed in ward with fluids and analgesia then discharged 5 days after admission with resolution of all symptoms after receiving a single 400mg dose of albendazole orally. After 7 days of discharge, the patient returns to complain of severe epigastric pain, at this time amylase get back to increase and was 2500 mg/dl, and the pt diagnosed as a case of recurrent attack of pancreatitis induced by ascariasis, MRCP again was done and showed remnants of worm and pancreatic duct still dilated and admitted for ERCP.
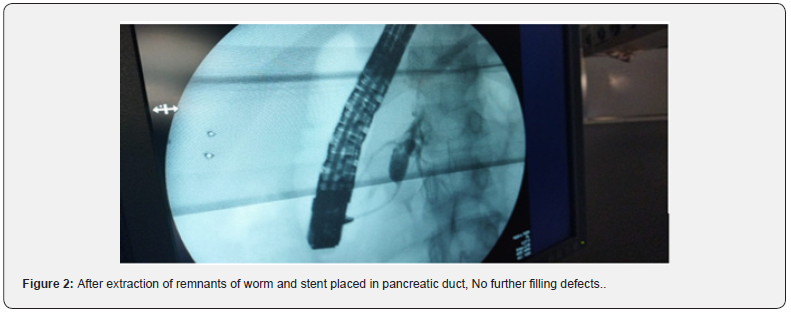
The patient underwent endoscopic retrograde cholangiopancreatography (ERCP), contrast injection into the common bile duct demonstrated normal biliary tree without filling defect. The duodenum and ampulla of vater were without any visualized pathology. While cannulating the papilla and contrast injection demonstrated a filling defect in pancreatic duct, papilloshincterotomy was done with extraction of remnants of ascaris and stent placed in the pancreatic duct. The patient was discharged 4 days after second admission with complete resolution of all symptoms with no complaints later on follow up. Subsequent contrasting showed no filling defects (Figure 2).
Discussion and Literature Review
Gallstones and excessive alcohol use [3] most often bring on acute pancreatitis. Usually, patient’s history, laboratory tests, and CT scan findings all pointed to pancreatitis. Two of the following three criteria must be met for the diagnosis of acute pancreatitis according to the revised Atlanta classification: (a) abdominal pain suggestive of pancreatitis; (b) serum amylase or lipase level greater than three times the upper normal value; or (c) characteristic imaging findings. The radiologic requirement is often met using contrast-enhanced CT, however MR imaging may also be employed in this situation [4]. Our patient fulfilled all of the diagnostic criteria for acute pancreatitis. In this context, it is important to emphasize that radiologists should be on the lookout for radiographic signs of round worm in the gastrointestinal tract, such as the echogenic tubular sign-strip sign on ultrasound, or relevant ERCP findings (smooth linear filling defect within the bile duct), or MRI findings (T2 linear filling defect with associated pancreatic duct dilation) [5].
Ascariasis is an uncommon cause of pancreatitis, and its symptoms differ depending on which part of the pancreas is afflicted. Patient history, physical exam, laboratory tests, and CT scan all came back negative, as stated in the case presentation. Idiopathic pancreatitis, for example, could not be entirely ruled out as a possible cause of the patient’s pancreatitis. In areas where helminthic infection is widespread, round worm may be a contributing factor. Worms may induce pancreatitis by blocking the pancreatic duct when they migrate from one location to another. According to one of Khuroo et al. [1,2] studies, they have a propensity to explore the orifices, and in the duodenum, the organism enters and exits the orifice of the ampulla of Vater on several occasions. The mature worm is responsible for blocking the ampullary aperture and the pancreatic and bile ducts. The worm’s writhing motions also significantly trigger sphincter spasm and dysmotility.
Klimovskij et al. [2] report that the most common presentations are biliary colic (56%), followed by acute cholangitis (25%), acute cholecystitis (13%), acute pancreatitis (6%), and, in very rare cases, hepatic abscess or haemobilia. In addition, ascariasis has been linked to duodenal perforation. It is fascinating to learn that the worm’s wandering and investigating habits may trigger a wide variety of other gastrointestinal symptoms. According to the research by Khuroo et al. [1] on ascariasis, the parasite may induce intestinal blockage, bowel infarction, and gangrene if it makes its way into the gut.
Appendicular ascariasis is characterized by the obstruction of the appendix opening, which results in appendicitis, gangrene, and appendicular colic. Perforation, peritonitis, and septic shock are all symptoms of peritoneal ascariasis. Pyloric blockage, nighttime choking due to Ascaris migrating into the gullet, and a distinctive retrosternal itch are all symptoms of ascariasis of the stomach and esophagus. In the case of hepatobiliary and pancreatic ascariasis, symptoms include biliary colic, acute cholangitis, acalculous cholecystitis (choledochal or gall bladder ascariasis; ascarides in the gall bladder may induce gall bladder gangrene), and hepatic abscess (hepatic ascariasis). Hepatolithiasis (dead ascarides in hepatic ducts generating nidus of sludge/stones) and acute pancreatitis (duodenal ascariasis or pancreatic ascariasis; ascaride in pancreatic duct may induce necrotizing pancreatitis) are additional symptoms.
Ascariasis was recognized as the etiologic agent in five (6%) of 84 hospitalized patients with ascariasis-induced pancreatitis [6]. Hepatobiliary and pancreatic ascariasis is endemic in several parts of the globe, as stated in a recent paper by Khuroo et al. [7] Several large series of patients from endemic regions, including Kashmir, Kolkata, Assam, Saudi Arabia, Syria, the Philippines, and South Africa, have been reported in medical journals. However, in Gaza Strip, there have not been any documented cases as of yet. In Gaza Strip, Palestine, this is the first case report of its kind. Consequently, it is suspected that it may be underdiagnosed.
conservative treatment can be used alone without further invasion procedures [8,9]. First choice drugs used for eradication of helminths are albendazole and mebendazole, and, alternatively, levamisole [9,10]. In our case, invasive methods were essential because of recurrent attack of pancreatitis occur. However, dead ascarides can induce chronic inflammation processes in the ductal mucosa, leading to strictures. Moreover, remnants of the dead worm can play the role of nuclei in biliary stone formation [11,12].
Ascariasis is one of the rare causes of acute pancreatitis. It should be considered as one of the etiologies in geographical regions where ascariasis is common, or sanitation and hygiene is poor. It is also recommended that the radiologist in the ascariasis endemic regions should be vigilant for radiographic signs of roundworm presence in the gastrointestinal tract.
References
- Khuroo MS, Rather AA, Khuroo NS, Khuroo MS (2016) Hepatobiliary and pancreatic ascariasis. World J Gastroenterol 22: 7507-7517.
- Klimovskij M, Dulskas A, Kraulyte Z, Mikalauskas S (2015) Ascariasis of the pancreatic duct. BMJ Case Rep.
- Wang GJ, Gao CF, Wei D, Wang C, Ding SQ (2009) Acute pancreatitis: etiology and common pathogenesis. World J Gastroenterol. 15(12): 1427-1430.
- Foster BR, Jensen KK, Bakis G, Shaaban AM, Coakley FV (2016) Revised Atlanta classification for acute pancreatitis: a pictorial essay. RadioGraphics 36: 675-687.
- (2020) Ascaris-induced pancreatitis. https://radiopaedia.org/articles/ascaris-induced-pancreatitis-1.
- Leung JW, Mok SD, Metreweli C (1987) Ascaris-induced pancreatitis. Am J Roentgenol 149: 511-512.
- Khuroo MS, Zargar SA (1985) Biliary ascariasis. A common cause of biliary and pancreatic disease in an endemic area. Gastroenterology 88(2): 418-423.
- Gonen KA, Mete R (2010) A rare case of ascariasis in the gallbladder, choledochus and pancreatic duct. Turk J Gastroenterol 21(4): 454-457.
- Gonzalez AH, Regalado VC, Van den Ende J (2001) Non-invasive management of Ascaris lumbricoides biliary tact migration: a prospective study in 69 patients from Ecuador. Trop Med Int Health 6(2): 146-150.
- Leder K, Weller PF, Ryan ET Ascariasis.
- Phisalprapa P, Prachayakul V (2013) Ascariasis as an unexpected cause of acute pancreatitis with cholangitis: a rare case report from urban area. JOP 14: 88-91.
- Alam S, Mustafa G, Rahman S (2010) Comparative study on presentation of biliary ascariasis with dead and living worms. Saudi J Gastroenterol 16(3): 203-206.






























