Irritable Gastrointestinal Syndrome
Mehmet Rami Helvaci1*, Yasemin Kayabasi2, Ayse Ceylan2, Guner Dede3, Abdulrazak Abyad4 and Lesley Pocock5
1Specialist of Internal Medicine, Turkey
2Manager of Writing and Statistics, Turkey
3Ministry of Health of Turkey, Turkey
4Middle-East Academy for Medicine of Aging, Turkey
5Medi-World International, Turkey
Submission:January 11, 2023; Published:February 17, 2023
*Corresponding author:Mehmet Rami Helvaci, Specialist of Internal Medicine, 07400, Alanya, Turkey
How to cite this article:Mehmet Rami Helvaci, Yasemin Kayabasi, Ayse Ceylan, Guner Dede, Abdulrazak Abyad and Lesley Pocock. Irritable Gastrointestinal Syndrome. Adv Res Gastroentero Hepatol, 2023; 19(3): 556012. DOI: 10.19080/ARGH.2023.19.556012.
Abstract
Background: Recurrent upper abdominal discomfort may be the cause of nearly half of the applications to the Internal Medicine Clinics, and irritable bowel syndrome (IBS) and chronic gastritis (CG) may be the most commonly diagnosed disorders in such cases.
Method: Consecutive patients with the IBS and age and sex-matched controls were included.
Results: The study included 936 patients with the IBS (592 females) and 346 control cases, totally. Mean age of the patients was 41.0 years, and 63.2% of them were female. Although gastric sample biopsies were taken just in suspected cases, CG was diagnosed nearly in all of the patients with the IBS (80.4% versus 15.0%, p<0.001). Similarly, prevalence’s of antidepressants use (46.4% versus 16.1%, p<0.001), smoking (35.2% versus 20.8%, p<0.001), hemorrhoids (37.1% versus 7.2%, p<0.001), and urolithiasis (22.0% versus 9.5%, p<0.001) were all higher in the IBS patients, significantly. Beside that the mean values of fasting plasma glucose (FPG) (111.9 versus 105.4mg/dL, p= 0.002) and plasma triglycerides (167.0 versus 147.3 mg/dL, p= 0.013) were also higher in the IBS patients, significantly.
Conclusion: Because FPG and triglycerides are well-known acute phase reactants in the body, IBS and CG may be low-grade inflammatory processes initiated with anxiety, depression, infection, inflammation, trauma, and cancer fear-like stresses of the body, and eventually terminate with smoking, antidepressants use, hemorrhoids, and urolithiasis. Because of the highly significant association of the IBS and CG, they may actually be the two sides of the same paper and should be called irritable gastrointestinal syndrome.
Keywords: Irritable bowel syndrome; Chronic gastritis; Depression; Smoking, acute phase reactant; Fasting plasma glucose; Triglycerides
Abbreviations: IBS: Irritable Bowel Syndrome; CG: Chronic Gastritis; TC: Triglycerides; HDL: High Density Lipoproteins; ESR: Erythrocyte Sedimentation Rate; CRP: C-Reactive Protein; FPG: Fasting Plasma Glucose; BMI: Body Mass Index; BP: Blood Pressure; WCH: White Coat Hypertension; HT: Hypertension; COPD: Chronic Obstructive Pulmonary Disease; CHD: Coronary Heart Disease; CRD: Chronic Renal Disease; TNF: Tumor Necrosis Factor; ATP: Adult Treatment Panel; LDL: Low Density Lipoproteins; APRs: Acute Phase Reactants; AUD: Alcohol Use Disorder; NAD: Nicotinamide Adenine Dinucleotide; VLDL: Very Low Density Lipoproteins
Introduction
Recurrent upper abdominal discomfort may be the cause of nearly half of the applications to the Internal Medicine Clinics, and irritable bowel syndrome (IBS) and chronic gastritis (CG) may be the most commonly diagnosed disorders in such cases [1]. According to the literature, nearly 20% of general population have IBS, and it is more common in females [2]. Flatulence, periods of diarrhea and constipation, repeated toilet visits due to urgent evacuation or early filling sensation, excessive straining, feeling of incomplete evacuation, frequency, urgency, reduced feeling of well-being, and eventually disturbed social life are often reported with the IBS. A meaningful dietary role is doubtful, and psychological factors seem to precede onset and exacerbation of gut symptoms. Many potentially psychiatric disorders including anxiety, depression, sleep disorders, cancer fear, or death fear usually coexist with the IBS [3]. For example, thresholds for sensations of initial filling, evacuation, urgent evacuation, and utmost tolerance recorded via a rectal balloon decreased by focusing the examiners’ attention on gastrointestinal stimuli by reading pictures of gastrointestinal malignancies in the IBS [4]. In other words, although IBS is described as a physical disorder according to Rome II guidelines, psychological factors may be crucial for triggering of these physical changes. IBS may have a more complex mechanism by affecting various systems of the body with a low-grade inflammatory process [5]. Eventually, IBS may even terminate with CG, urolithiasis, and hemorrhoids [6-8].
Similarly, some authors studied the role of inflammation in the IBS by means of colonic biopsies in 77 patients [9]. Although 38 patients had normal histology, 31 patients demonstrated microscopic inflammation, and eight patients fulfilled criteria for lymphocytic colitis. However, immunohistology revealed increased intraepithelial lymphocytes as well as increased CD3 and CD25 positive cells in lamina propria of the group with “normal” histology. These features were more evident in the microscopic inflammation group who additionally revealed increased neutrophils, mast cells, and natural killers. All of these immunopathological abnormalities were the most evident in the lymphocytic colitis group who also demonstrated HLA-DR staining in the crypts and increased CD8 positive cells in the lamina propria [9]. Some other authors demonstrated not only an increased mast cell degranulation in the colon but also a direct correlation between proximity of mast cells to neuronal elements and severity of pain in the IBS [10]. In addition to the above findings, there is some evidence for extension of the inflammatory process behind the mucosa. Some authors addressed this issue in ten patients with the severe IBS by examining full thickness of jejunal biopsies obtained, laparoscopically [11]. They detected a low-grade infiltration of lymphocytes into the myenteric plexus of nine patients, four of whom had an associated increase in intraepithelial lymphocytes and six demonstrated evidence of neuronal degeneration [11]. Nine patients had hypertrophy of longitudinal muscles, and seven had abnormalities in the number and size of interstitial cells of Cajal [11]. The finding of intraepithelial lymphocytosis was consistent with some other reports in the colon and duodenum, too [9,12]. We tried to understand whether or not there is a significant association between the IBS and CG in the human body.
Material and Methods
The study was performed in the Internal Medicine Clinic of the Dumlupinar University between August 2005 and March 2007. Consecutive patients with upper abdominal discomfort were taken into the study. Their medical histories including smoking, alcohol, urolithiasis, and already used medications including antidepressants at least for a period of six months were learned. Patients with devastating illnesses including eating disorders, malignancies, acute or chronic renal failure, cirrhosis, hyper- or hypothyroidism, or heart failure were excluded. Current daily smokers for at least for the last six months and cases with a history of five pack years were accepted as smokers. Patients with regular alcohol consumption (one drink a day) were accepted as drinkers. A routine checkup procedure including fasting plasma glucose (FPG), total cholesterol (TC), triglycerides, high density lipoproteins (HDL), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), albumin, creatinine, thyroid function tests, hepatic function tests, markers of hepatitis A, B, C, and human immunodeficiency viruses, a urinalysis, a posterior-anterior chest x-ray graphy, an electrocardiogram, a Doppler echocardiogram in case of requirement, an abdominal ultrasonography, an abdominal x-ray graph in supine position, a recto sigmoidoscopy just in patients symptomatic for hemorrhoids, and a questionnaire for the IBS was performed. IBS was diagnosed according to Rome II criteria in the absence of red flag symptoms including pain, nocturnal diarrhea, weight loss, fever, and any abnormal finding of the physical examination.
An upper gastrointestinal endoscopy was performed, and sample biopsies were taken just in cases with suspicion. CG is diagnosed histologically. Infiltrations of neutrophils and monocytes into the gastric mucosa is the hallmark of CG [13]. An additional intravenous pyelography was performed according to the results of the urinalysis and abdominal x-ray graphy. So, urolithiasis was diagnosed either by medical history or as a result of current clinical and laboratory findings. Body mass index (BMI) of each case was calculated by measurements of Same Physician instead of verbal expressions. Cases with an overnight FPG level of 126mg/dL or greater on two occasions or already using antidiabetic medications were defined as diabetics [14]. An oral glucose tolerance test with 75-gram glucose was performed in cases with FPG levels between 100 and 126mg/ dL, and diagnosis of cases with two-hour plasma glucose levels of 200mg/dL or greater is diabetes mellitus (DM) [14]. Office blood pressure (OBP) was checked after five minutes of rest in seated position with mercury sphygmomanometer on three visits, and no smoking was permitted during the previous two hours. Ten days twice daily measurements of blood pressure at home (HBP) were obtained in all cases, even in normotensives in the office due to the risk of masked hypertension after an education about proper blood pressure (BP) measurement techniques [15]. The education included recommend seated of upper arm devices, using a standard adult cuff with bladder sizes of 12 × 26cm for arm circumferences up to 33cm in length and a large adult cuff with bladder sizes of 12 × 40cm for arm circumferences up to 50cm in length, and taking a rest for a period of five minutes in seated position before measurements. An additional 24-hour ambulatory blood pressure monitoring was not required due to the equal efficacy of the HBP measurements to diagnose hypertension (HT) [16]. HT is defined as a mean BP of 140/90mmHg or greater on HBP measurements, and white coat hypertension (WCH) is defined as an OBP of 140/90mmHg or greater, but a mean HBP value of lower than 140/90mmHg [15]. Eventually, all patients with the IBS were collected into the first and age and sex-matched control cases were collected into the second groups and compared in between. Mann-Whitney U test, Independent-Samples T test, and comparison of proportions were used as the methods of statistical analyses.
Results
The study included 936 patients with the IBS (592 females) and 346 control cases, totally. Mean age of the patients was 41.0 years, and 63.2% of them were female. Although gastric tissue biopsies were taken just in suspected cases, CG was diagnosed nearly in all of the patients with the IBS (80.4% versus 15.0%, p<0.001). Similarly, prevalence’s of antidepressants use (46.4% versus 16.1%, p<0.001), smoking (35.2% versus 20.8%, p<0.001), hemorrhoids (37.1% versus 7.2%, p<0.001), and urolithiasis (22.0% versus 9.5%, p<0.001) were all higher in the IBS patients, significantly. Besides that, the mean values of FPG (111.9 versus 105.4mg/dL, p= 0.002) and plasma triglycerides (167.0 versus 147.3mg/dL, p= 0.013) were also significantly higher in the IBS patients (Table 1). Due to the limited number of cases with alcoholism among the study cases, regular alcohol consumption was not included in comparison.
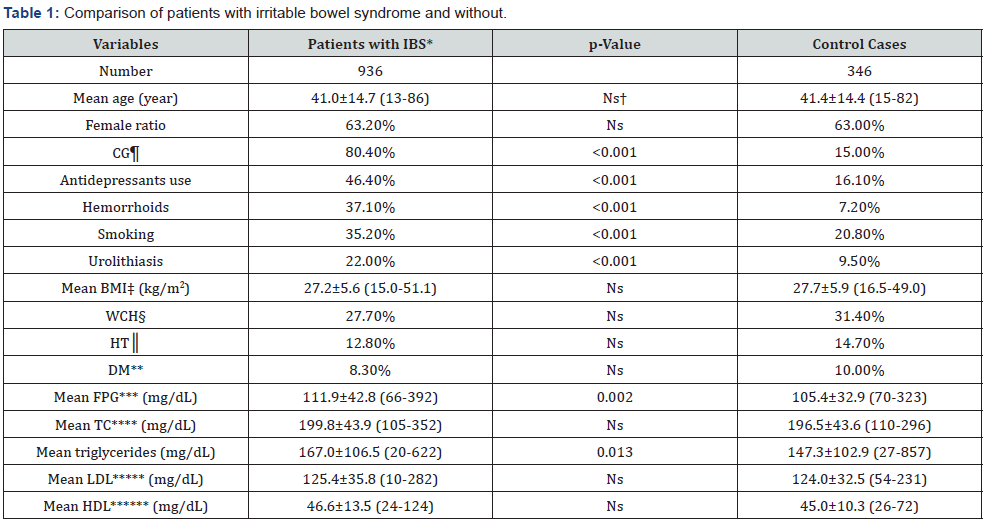
*Irritable bowel syndrome, †Nonsignificant (p>0.05), ¶Chronic gastritis, ‡Body mass index, §White coat hypertension, ║Hypertension, **Diabetes mellitus, ***Fasting plasma glucose, ****Total cholesterol, *****Low-density lipoprotein, ******High-density lipoprotein
Discussion
The monolayer of endothelial cells that forms the inner lining of arteries, veins, capillaries, and lymphatics is called endothelium. Probably, the whole endothelium all over the body may act as a separate organ that may be the largest organ of the body. It may contract vasculature of the peripheral organs while relaxing the internal ones during cold, anxiety, and depression-like stresses. Because we measure the systolic and diastolic BPs of the arms and legs, they may not show the actual BPs of the brain, heart, lung, liver, and kidney-like internal organs. The endothelium may be the main organ in the control of blood fluidity, platelets aggregation, and vascular tone all over the body. It may control vascular tone and blood flow by releasing nitric oxide, reactive oxygen species, and metabolites of arachidonic acid into the circulation. It may also be important for synthesizing of vasoactive hormones such as angiotensin II. An endothelial dysfunctioninduced accelerated atherosclerosis all over the body may be the main cause of end-organ insufficiencies, aging, and death. Such a dysfunction may also be important in the development of cancers by preventing clearance of malignant cells by the natural killers in terminal points of the circulation. Similarly, physical inactivity, animal-rich diet, excess weight, higher BP and glucose levels, chronic inflammations, prolonged infections, cancers, smoking, and alcohol may be accelerating factors of the chronic endothelial inflammation and dysfunction terminating with the accelerated atherosclerosis-induced end-organ insufficiencies [17]. The much higher BP of the afferent vasculature may be the major accelerating factor by inducing recurrent injuries on the vascular endothelium. Probably, whole afferent vasculature including capillaries are mainly involved in the process. Thus, the term Ven sclerosis is not as famous as atherosclerosis in the medical literature. Due to the chronic endothelial damage, inflammation, edema, fibrosis, and dysfunction, vascular walls thicken, their lumens narrow, and they lose their elastic natures, those eventually reduce blood flow to the terminal organs, and increase systolic and decrease diastolic BPs further. Some of the irreversible consequences of the systemic inflammatory process are obesity, HT, DM, cirrhosis, peripheric artery disease, chronic obstructive pulmonary disease (COPD), coronary heart disease (CHD), chronic renal disease (CRD), mesenteric ischemia, osteoporosis, stroke, dementia, early aging, and premature death [18]. Although early withdrawal of the accelerating factors may delay terminal consequences, endothelial changes cannot be reversed, completely after development of the irreversible end-points due to their fibrotic natures. The accelerating factors and irreversible consequences are researched under the titles of the metabolic syndrome, aging syndrome, and accelerated endothelial damage syndrome in the literature, extensively [19,20].
Obesity may be one of the irreversible endpoints of the metabolic syndrome. Although some transient successes can be achieved, nonpharmaceutical approaches provide limited benefit to reverse obesity, permanently. Due to the excess weight-induced chronic low-grade inflammation on the vascular endothelium, the risk of death from all causes including cardiovascular diseases and cancers increases parallel to the range of excess weight in all age groups [21]. The chronic low-grade inflammation may even cause genetic changes of the endothelial cells, and systemic atherosclerosis may prevent clearance of malignant cells, effectively. Similarly, the effects of excess weight on the BP were shown in the literature, extensively [22]. For example, prevalence’s of sustained normotension (NT) were higher in the underweight than the normal weight (80.3% versus 64.0%, p<0.05) and overweight groups (80.3% versus 31.5%, p<0.001) [22], and 52.8% of patients with HT had obesity against 14.5% of patients with the sustained NT (p<0.001) [23]. So, the major underlying cause of the metabolic syndrome appears to be weight gain that may be the main cause of insulin resistance, hyperlipoproteinemia’s, impaired fasting glucose, impaired glucose tolerance, and WCH [24]. Interestingly, weight gain before the development of an obvious overweight or obesity may even cause development of several components of the metabolic syndrome. For example, WCH alone may be a strong indicator of weight gain even before the development of excess weight [22,23]. On the other hand, prevention of weight gain with physical activity even in the absence of a prominent weight loss usually results with resolution of many parameters of the syndrome [25]. According to our experiences, excess weight may actually be a result of physical inactivity instead of an excessive eating habit. In another words, there is a problem with burning calories instead of getting them. Therefore, prevention of weight gain cannot be achieved by diet, alone [26]. On the other hand, limitation of excess weight as an excessive fat tissue around abdomen under the heading of abdominal obesity may be meaningless, instead it should be defined as overweight or obesity by means of the BMI. Because adipocytes function as an endocrine organ, and they release leptin, tumor necrosis factor (TNF)-alpha, plasminogen activator inhibitor-1, and adiponectin-like cytokines into the plasma [27]. Eventual hyperactivities of sympathetic nervous system and renin-angiotensin-aldosterone system are probably associated with insulin resistance, elevated BP, and chronic endothelial inflammation and dysfunction. Similarly, the Adult Treatment Panel (ATP) III reported that although some people classified just as overweight with larger muscular masses, most of them also have excess fat tissue predisposing to the irreversible endpoints of the metabolic syndrome [14].
Smoking may be the second common cause of systemic vasculitis in the world. It is one of the major risk factors for atherosclerotic end-organ insufficiencies [28]. Its atherosclerotic effect is the most obvious in Buerger’s disease. Buerger’s disease is an obliterative vasculitis characterized by inflammatory changes in the small and medium-sized arteries and veins, and it has never been reported in the absence of smoking in the literature. Smoking may cause a low-grade systemic inflammation on vascular endothelium terminating with an accelerated atherosclerosis-induced end-organ insufficiencies all over the body. Plasma triglycerides, low density lipoproteins (LDL), ESR, and CRP may be positive whereas HDL and FPG may be negative acute phase reactants (APRs) indicating such inflammatory effects in the body [29]. Besides the obvious atherosclerotic effects of smoking, some studies reported that smoking in human beings and nicotine administration in animals are associated with the lower values of BMI [30]. Some evidence revealed an increased energy expenditure during smoking both on rest and light physical activity [31]. Nicotine supplied by patch after smoking cessation decreased caloric intake in a dose-related manner [32]. According to an animal study, nicotine may lengthen inter mealtime, and decrease amount of meal eaten [33]. Smoking may be associated with a post cessation weight gain, but the risk is the highest during the first year and decreases with the following years [34]. As the opposite findings to the above studies, the mean weight and BMI were similar both in the smokers and non-smokers in the other study [29].
Similarly, prevalence’s of smoking were similar in the normal weight (35.9%), overweight (32.9%), and obesity groups (33.7%, p>0.05 between all) in another study [35]. On the other hand, although the CHD was detected with similar prevalence’s in both genders, prevalence’s of smoking and COPD were higher in males against the higher BMI, LDL, triglycerides, WCH, HT, and DM in females [36]. Beside that the prevalence of myocardial infarctions is increased three-fold in men and six-fold in women who smoked at least 20 cigarettes per day [37]. In another words, smoking may be more dangerous for women about the atherosclerotic endpoints probably due to the higher BMI and its consequences in them. Several toxic substances found in the cigarette smoke get into the circulation and cause a vascular endothelial inflammation in all organ systems of the body. For example, smoking is usually reported together with depression, IBS, CG, hemorrhoids, and urolithiasis in the literature [6,7]. There may be several underlying mechanisms to explain these associations in the smokers [38]. First of all, smoking may have some additional antidepressant properties with several side effects. Secondly, smoking-induced vascular endothelial inflammation may disturb epithelial functions for absorption and excretion in the gastrointestinal and genitourinary tracts. These functional problems may terminate with urolithiasis and components of the IBS including loose stool, diarrhea, and constipation. Thirdly, diarrheal losses-induced urinary changes may even cause urolithiasis [6,7]. Fourthly, smoking-induced sympathetic nervous system activation may cause motility problems in the gastrointestinal and genitourinary tracts terminating with the IBS and urolithiasis. Eventually, immunosuppression secondary to smoking-induced vascular endothelial inflammation may even terminate with the gastrointestinal and genitourinary tract infections causing loose stool, diarrhea, and urolithiasis, because some types of bacteria can provoke urinary supersaturation, and modify the environment to form crystal deposits in the urine.
Actually, 10% of urinary stones are struvite stones which are built by magnesium ammonium phosphate produced during infections with the bacteria producing urease. Parallel to the results above, urolithiasis was detected in 17.9% of cases with the IBS and 11.6% of cases without in the other study (p<0.01) [6].
Alcohol may be the third common cause of systemic vasculitis in the world. It is addictive to humans, and can result in alcohol use disorder (AUD), dependence, and withdrawal. Alcohol is causally associated with more than 200 different pathologies including cancers in whole body [39]. Eventually, people hospitalized with AUD have an average life expectancy of 47-53 years in men and 50-58 years in women and die 24-28 years earlier than the others [40]. People with AUD have three-fold higher mortality in men and four-fold in women [41]. Similar to smoking, alcohol may be more dangerous for women about the atherosclerotic endpoints probably due to their lower body mass induced lower capacity to metabolize alcohol and higher body fat. A very substantial part of the Danish excess mortality and lower life expectancy compared to Sweden can be attributed to higher mortality related with alcohol and smoking [40]. It may even cause unconsciousness and sudden death if taken in high amounts. Hepatic alcohol dehydrogenase is the main enzyme to metabolize alcohol that requires the cofactor, nicotinamide adenine dinucleotide (NAD). Normally, NAD is used to metabolize fats in the liver, but alcohol competes with these fats for the use of NAD. Eventually, prolonged exposure of alcohol causes fatty liver. Ethanol is the only alcohol that is found in alcoholic beverages. Ethanol crosses biological membranes and blood-brain barriers by means of passive diffusion, easily.
Alcohol works particularly by increasing effects of the gamma aminobutyric acid that is the main inhibitory neurotransmitter of the brain. Alcohol causes happiness and euphoria, decreased anxiety, increased sociability, sedation, generalized depression of the central nervous system, and impairment of cognitive, memory, motor, and sensory functions. It may even cause fetal disorders in pregnancy since ethanol is classified as a teratogen. Regular alcohol consumption leads to cell death in the liver, scarring, cirrhosis, and hepatocellular carcinoma. Heavy alcohol consumption may even terminate with permanent brain damage. Alcohol is the major contributing factor of elevated triglycerides which are the sensitive APRs in plasma [24]. Although regular alcohol consumers were excluded, plasma triglycerides were higher in the smokers (163.1 versus 151.3mg/dL, p<0.05), indicating the inflammatory effects of smoking [42].
The acute phase response occurs in case of infection, infarction, cancer, trauma, and burn-like inflammatory conditions of the body. Certain mediators known as APRs are increased or decreased during the response [43,44]. These markers are commonly used in clinical practice as indicators of acute and chronic inflammations in the body. The terms of acute phase proteins and APRs are usually used synonymously, although some APRs are polypeptides rather than proteins. Positive and negative APRs are those whose concentrations increase or decrease during the acute phase response, respectively. The response is predominantly mediated by the pro-inflammatory cytokines including TNF, interleukin-1, and interleukin-6 secreted by neutrophils and macrophages into the circulation. The liver and other organs respond to the cytokines by producing many positive APRs. ESR, CRP, fibrinogen, ferritin, procalcitonin, hepcidin, haptoglobin, ceruloplasmin, complement proteins, and serum amyloid A are some of the well-known positive APRs. CRP is a useful indicator of the acute phase response, clinically. It is responsible for activation of the complement pathway. CRP reaches up to the maximum concentration within two days and decreases with the resolution of the inflammation with a half-life of 6-8 hours, rapidly. It correlates with ESR, but not simultaneously since ESR is largely dependent upon elevation of fibrinogen with a half-life of one week, approximately.
Thus, ESR remains higher for a longer period of time despite the removal of the inflammatory stimulus. Similarly, white blood cells and platelet counts may also behave as some other positive APRs in the body [45]. On the other hand, productions of the negative APRs are suppressed, simultaneously. Albumin, transferrin, retinol-binding protein, antithrombin, transcortin, alpha-fetoprotein, and hemoglobin are some of the well-known negative APRs in the body. Suppressions of such negative APRs are also used as indicators of the acute phase response in the body. Suppressions of such negative APRs may actually be secondary to the protection of amino acids and polypeptides required for the production of positive APRs, sufficiently. As also observed in the smokers in the above study [42], production of HDL may also be suppressed in the liver during the acute phase response [46]. Similarly, triglycerides, DM, and CHD were all higher in patients with plasma HDL values of lower than 40mg/dL, significantly [46]. So, HDL may actually behave negatively whereas triglycerides positive APRs in the plasma. Similarly, the highest CHD of the group with HDL values of lower than 40 mg/dL can also be explained by the same hypothesis in the other study [24]. Additionally, plasma triglycerides increased whereas HDL decreased during infections [47]. On the other hand, a 10 mg/dL increase of plasma LDL values was associated with a 3% lower risk of hemorrhagic stroke [48]. Similarly, the highest prevalence’s of HT and DM parallel to the elevated values of LDL and HDL, and the highest prevalence’s of COPD, CHD, and CRD in contrast to the lowest values of LDL and HDL may show initially positive but eventually negative behaviors of LDL and HDL as the APRs [49]. Probably, HDL turns in the negative direction much earlier than LDL in plasma. Interestingly, the most desired values were between 80 and 100mg/dL for LDL, between 40 and 46 mg/dL for HDL, and lower than 60mg/dL for triglycerides in the plasma [24]. Parallel to ESR and CRP, plasma triglycerides and LDL may behave as positive whereas FPG and HDL negative APRs in smokers in the above study [42]. In another words, lower HDL values should alert clinicians for researching of any acute phase response in the body [50,51].
Cholesterol, triglycerides, and phospholipids are the major lipids of the body. They do not circulate in plasma freely, instead they are bound to proteins and transported as lipoproteins. There are five major classes of lipoproteins in plasma. Chylomicrons carry exogenous triglycerides to the liver via the thoracic duct. Very low-density lipoproteins (VLDL) are produced in the liver and carry endogenous triglycerides to the organs. VLDL are converted into intermediate density lipoproteins (IDL) by removal of 90% of triglycerides by lipases in the capillaries of adipocytes and muscle tissues. Then the IDL is degraded into LDL by removal of more triglycerides. So VLDL is the main source of LDL in plasma, and LDL delivers cholesterol from the liver to organs. Although the liver removes the majority of LDL from the circulation, a small amount is up taken by scavenger receptors of the macrophages migrating into the arterial walls and become the foam cells of atherosclerotic plaques. HDL removes fats and cholesterol from cells including the arterial wall atheroma, and carries the cholesterol back to the adrenals, ovaries, and testes-like steroidogenic organs and liver for excretion, re-utilization, or disposal. All of the carrier lipoproteins are under dynamic control, and are readily affected by diet, drug, inflammation, infection, cancer, trauma, smoking, alcohol, and excess weight. Thus, lipid analysis should be performed during a steady state, but the metabolic syndrome alone is a lowgrade inflammatory process, and it may even cause abnormal lipoproteins levels in the plasma. HDL may normally show various anti-oxidative, anti-inflammatory, and anti-atherogenic properties including reverse cholesterol transport [52]. However, HDL may become ‘dysfunctional’ in pathologic conditions which means that relative compositions of lipids and proteins, as well as the enzymatic activities of HDL are altered [52]. For example, properties of HDL are compromised in patients with DM by means of the oxidative modification, glycation, and/or transformation of HDL proteomes into the proinflammatory proteins.
Additionally, the drugs increasing HDL values such as niacin, fibrates, and cholesteryl ester transfer protein inhibitors cannot reduce all-cause mortality, CHD mortality, myocardial infarction, and stroke [53]. In other words, HDL may just be some indicators instead of being the main actors of the health. Similarly, BMI, DM, and CHD were the lowest between the HDL values of 40 and 46mg/ dL, and the prevalence of DM was only 3.1% between these values against 22.2% outside these limits [54]. Similar to the above study [42], HDL and FPG values were also suppressed in the sickle cell diseases (SCDs), probably due to the severe inflammatory nature of the diseases [55]. Smoking may reduce HDL and FPG by means of the moderate or severe inflammatory effects on the vascular endothelium all over the body [29]. On the other hand, triglycerides alone may be one of the most sensitive APRs indicating the metabolic syndrome [56]. Although ATP II determined the normal plasma triglycerides as lower than 200mg/dL in 1994 [57], World Health Organization in 1999 [58] and ATP III in 2001 reduced the normal limits as lower than 150mg/dL [14]. Although these cut points, there are still suspicions about the safest values of triglycerides in plasma [56]. Besides that, triglycerides are the only lipids which were not suppressed with the pathological weight loss [59]. For example, plasma triglycerides increased in contrast to the suppressed body weight and BMI in the SCDs [59]. Similarly, prevalence’s of excess weight, DM, HT, and smoking were all higher in the hypertriglyceridemia group (200mg/dL and higher) in the other study [60]. Interestingly, the greatest number of deteriorations of the metabolic parameters was observed with the triglyceride’s values of 60mg/dL and higher [56].
The body’s homeostatic mechanism keeps blood glucose levels within a narrow range with two groups of mutually antagonistic hormones. Glucagon, cortisol, and catecholamines are the catabolic hormones increasing the blood glucose, whereas insulin is the anabolic hormone decreasing the blood glucose levels. Glucagon is secreted from the alpha cells while insulin is secreted from the beta cells of pancreatic islets which are the bundles of endocrine tissues. When the blood glucose levels are too high, insulin tells muscles to take up excess glucose for storage as glycogen. When the blood glucose levels are too low, glucagon informs the tissues to produce more glucose from the stores of glycogen. Catecholamines prepare the muscles and respiratory system for a ‘fight to fight’ response. Cortisol prepares the body for the various stresses. A blood glucose level of four grams, or about a teaspoon, is critical for the normal function of millions of cells of a person with the weight of 70kg [61]. The constant blood glucose levels are maintained via the hepatic and muscular glycogen stores on fasting. There are approximately 100 and 400 grams of glycogen stored in the skeletal muscles and liver, respectively [61].
The brain consumes about 60% of the blood glucose on fasting. FPG is the most commonly used indication of overall glucose homeostasis, and it is measured after a fasting period of 8 hours. Infection, inflammation, surgical operation, depression, alcohol, and smoking-like stresses may affect blood glucose homeostasis. For example, smoking was negatively associated with the FPG and DM in Chinese men with the normal weight, but not in men with excess weight or in women [62]. Similarly, smokers have a lower likelihood of newly-diagnosed DM in Chinese men with a lower BMI in the other study [63]. Parallel to the above studies, FPG and DM were also lower in the smokers (102.3 versus 111.6mg/ dL, p=0.007 and 8.9% versus 14.3%, p<0.05, respectively), and although majority of the smokers were male again (70.0%), BMI was higher (26.6kg/m2) in contrast to the above studies [42].
Conclusion
As a conclusion, because FPG and plasma triglycerides are well-known APRs in the body, IBS and CG may be low-grade inflammatory processes initiated with anxiety, depression, infection, inflammation, trauma, and cancer fear-like stresses of the body, and eventually terminate with smoking, antidepressants use, hemorrhoids, and urolithiasis. Because of the highly significant association of the IBS and CG, they may actually be the two sides of the same paper and should be called irritable gastrointestinal syndrome in the literature.
References
- Valenkevich LN, Iakhontov OI (2004) Modern myths of clinical gastroenterology. Eksp Klin Gastroenterol 105(3): 72-74.
- Rhee PL (2006) Definition and epidemiology of irritable bowel syndrome. Korean J Gastroenterol 47(2): 94-100.
- Lee OY (2006) Psychosocial factors and visceral hypersensitivity in irritable bowel syndrome. Korean J Gastroenterol 47(2): 111-119.
- Wang W, Pan G, Qian J (2002) Effect of psychological factors on visceral sensation of patients with irritable bowel syndrome. Zhonghua Yi Xue Za Zhi 82(5): 308-311.
- Park H (2006) The pathophysiology of irritable bowel syndrome: inflammation and motor disorder. Korean J Gastroenterol 47(2): 101-110.
- Helvaci MR, Kabay S, Gulcan E (2006) A physiologic events’ cascade, irritable bowel syndrome, may even terminate with urolithiasis. J Health Sci 52(4): 478-481.
- Helvaci MR, Algin MC, Kaya H (2009) Irritable bowel syndrome and chronic gastritis, hemorrhoid, urolithiasis. Eurasian J Med 41(3): 158-161.
- Helvaci MR, Kaya H, Algin MC, Yalcin A (2008) A physiologic events’ cascade: irritable bowel syndrome may even terminate with chronic gastritis. Med J Malaysia 63(2): 140-142.
- Chadwick VS, Chen W, Shu D, Paulus B, Bethwaite P, et al. (2002) Activation of the mucosal immune system in irritable bowel syndrome. Gastroenterology 122(7): 1778-1783.
- Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, et al. (2004) Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology 126(3): 693-702.
- Tornblom H, Lindberg G, Nyberg B, Veress B (2002) Full-thickness biopsy of the jejunum reveals inflammation and enteric neuropathy in irritable bowel syndrome. Gastroenterology 123(6): 1972-1979.
- Wahnschaffe U, Ullrich R, Riecken EO, Schulzke JD (2001) Celiac disease-like abnormalities in a subgroup of patients with irritable bowel syndrome. Gastroenterology 121(6): 1329-1338.
- Lapii GA, Nepomnyashchikh DL, Khudaiberganova LKh (2004) Structural and functional changes in gastric epithelium in Helicobacter pylori-associated chronic gastroduodenal pathologies. Bull Exp Biol Med 138(4): 418-422.
- Third Report of the National Cholesterol Education Program (NCEP) (2002) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106(25): 3143-3421.
- O'Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, et al. (2003) European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens 21(5): 821-848.
- Helvaci MR, Seyhanli M (2006) What a high prevalence of white coat hypertension in society! Intern Med 45(10): 671-674.
- Helvaci MR, Kaya H, Borazan A, Ozer C, Seyhanli M, et al. (2008) Metformin and parameters of physical health. Intern Med 47(8): 697-703.
- Helvaci MR, Algin MC, Abyad A, Pocock L (2018) Physical inactivity or an excessive eating habit. Middle East J Nursing 12(1): 14-18.
- Eckel RH, Grundy SM, Zimmet PZ (2005) The metabolic syndrome. Lancet 365(9468): 1415-1428.
- Helvaci MR, Ayyildiz O, Muftuoglu OE, Yaprak M, Abyad A, et al. (2017) Aging syndrome. World Family Med 15(3): 39-42.
- Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW (1999) Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med 341(15): 1097-1105.
- Helvaci MR, Kaya H, Yalcin A, Kuvandik G (2007) Prevalence of white coat hypertension in underweight and overweight subjects. Int Heart J 48(5): 605-613.
- Helvaci MR, Kaya H, Duru M, Yalcin A (2008) What is the relationship between white coat hypertension and dyslipidemia? Int Heart J 49(1): 87-93.
- Helvaci MR, Yapyak M, Tasci N, Abyad A, Pocock L (2020) The most desired values of high- and low-density lipoproteins and triglycerides in the plasma. World Family Med 18(8): 21-27.
- Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi T, Azizi F (2005) Beneficial effects of a Dietary Approaches to Stop Hypertension eating plan on features of the metabolic syndrome. Diabetes Care 28(12): 2823-2831.
- Helvaci MR, Ayyildiz O, Gundogdu M, Aydin Y, Abyad A, et al. (2019) Body mass and blood pressure. World Family Med 17(1): 36-40.
- Funahashi T, Nakamura T, Shimomura I, Maeda K, Kuriyama H, et al. (1999) Role of adipocytokines on the pathogenesis of atherosclerosis in visceral obesity. Intern Med 38(2): 202-206.
- Fodor JG, Tzerovska R, Dorner T, Rieder A (2004) Do we diagnose and treat coronary heart disease differently in men and women? Wien Med Wochenschr 154(17-18): 423-425.
- Helvaci MR, Altintas E, Yalcin A, Muftuoglu OE, Abyad A, et al. (2022) Positive and negative acute phase reactants in smokers. Middle East J Nursing 16(2): 42-48.
- Grunberg NE, Greenwood MR, Collins F, Epstein LH, Hatsukami D, et al. (1992) National working conference on smoking and body weight. Task Force 1: Mechanisms relevant to the relations between cigarette smoking and body weight. Health Psychol 11: 4-9.
- Walker JF, Collins LC, Rowell PP, Goldsmith LJ, Moffatt RJ, et al. (1999) The effect of smoking on energy expenditure and plasma catecholamine and nicotine levels during light physical activity. Nicotine Tob Res 1(4): 365-370.
- Hughes JR, Hatsukami DK (1997) Effects of three doses of transdermal nicotine on post-cessation eating, hunger and weight. J Subst Abuse 9: 151-159.
- Miyata G, Meguid MM, Varma M, Fetissov SO, Kim HJ (2001) Nicotine alters the usual reciprocity between meal size and meal number in female rat. Physiol Behav 74(1-2): 169-176.
- Froom P, Melamed S, Benbassat J (1998) Smoking cessation and weight gain. J Fam Pract 46(6): 460-464.
- Helvaci MR, Altintas E, Yalcin A, Muftuoglu OE, Abyad A, et al. (2023) Smoking may not prevent overweight or obesity. World Family Med.
- Helvaci MR, Kaya H, Gundogdu M (2012) Gender differences in coronary heart disease in Turkey. Pak J Med Sci 28(1): 40-44.
- Prescott E, Hippe M, Schnohr P, Hein HO, Vestbo J (1998) Smoking and risk of myocardial infarction in women and men: longitudinal population study. BMJ 316(7137): 1043-1047.
- Helvaci MR, Dede G, Yildirim Y, Salaz S, Abyad A, et al. (2019) Smoking may even cause irritable bowel syndrome. World Family Med 17(3): 28-33.
- Rehm J (2014) Alcohol and mortality. Alcohol Res 35(2): 174-183.
- Juel K (2008) Life expectancy and mortality in Denmark compared to Sweden. What is the effect of smoking and alcohol? Ugeskr Laeger 170(33): 2423-2427.
- Westman J, Wahlbeck K, Laursen TM, Gissler M, Nordentoft M, et al. (2015) Mortality and life expectancy of people with alcohol use disorder in Denmark, Finland, and Sweden. Acta Psychiatr Scand 131(4): 297-306.
- Helvaci MR, Kayabasi Y, Celik O, Dede G, Abyad A, et al. (2014) What a lower prevalence of diabetes mellitus but higher incidence of dyslipidemia in smokers. World Family Med (in press).
- Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340(6): 448-454.
- Wool GD, Reardon CA (2007) The influence of acute phase proteins on murine atherosclerosis. Curr Drug Targets 8(11): 1203-1214.
- Helvaci MR, Aydogan F, Sevinc A, Camci C, Dilek I (2014) Platelet and white blood cell counts in severity of sickle cell diseases. HealthMED 8(4): 477-482.
- Helvaci MR, Abyad A, Pocock L (2020) High and low density lipoproteins may be negative acute phase proteins of the metabolic syndrome. Middle East J Nursing 14(1): 10-16.
- Pirillo A, Catapano AL, Norata GD (2015) HDL in infectious diseases and sepsis. Handb Exp Pharmacol 224: 483-508.
- Ma C, Na M, Neumann S, Gao X (2019) Low-density lipoprotein cholesterol and risk of hemorrhagic stroke: a systematic review and dose-response meta-analysis of prospective studies. Curr Atheroscler Rep 21(12): 52.
- Helvaci MR, Abyad A, Pocock L (2020) The safest values of low density lipoproteins in the plasma. World Family Med 18(4): 18-24.
- Toth PP (2005) Cardiology patient page. The "good cholesterol": high-density lipoprotein. Circulation 111(5): 89-91.
- Ertek S (2018) High-density lipoprotein (HDL) dysfunction and the future of HDL. Curr Vasc Pharmacol 16(5): 490-498.
- Femlak M, Gluba BA, Cialkowska RA, Rysz J (2017) The role and function of HDL in patients with diabetes mellitus and the related cardiovascular risk. Lipids Health Dis 16(1): 207.
- Keene D, Price C, Shun SMJ, Francis DP (2014) Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: meta-analysis of randomised controlled trials including 117,411 patients. BMJ 349: 4379.
- Helvaci MR, Abyad A, Pocock L (2020) What a low prevalence of diabetes mellitus between the most desired values of high-density lipoproteins in the plasma. World Family Med 18(7): 25-31.
- Helvaci MR, Altintas E, Yalcin A, Muftuoglu OE, Abyad A, et al. (2022) Positive and negative acute phase reactants in sickle cell diseases. World Family Med 20(3): 36-42.
- Helvaci MR, Abyad A, Pocock L (2020) The safest upper limit of triglycerides in the plasma. World Family Med 18(1): 16-22.
- National Cholesterol Education Program (1994) Second Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II). Circulation 89(3): 1333-1445.
- World Health Organization (1999) Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications. Report of a WHO consultation.
- Helvaci MR, Salaz S, Yalcin A, Muftuoglu OE, Abyad A, et al. (2021) Cholesterol may be a negative whereas triglycerides positive acute phase reactants in the plasma. Asclepius Med Res Rev 4(1): 1-8.
- Helvaci MR, Aydin LY, Maden E, Aydin Y (2011) What is the relationship between hypertriglyceridemia and smoking? Middle East J Age and Ageing 8(6).
- Wasserman DH (2009) Four grams of glucose. Am J Physiol Endocrinol Metab 296(1): E11-21.
- Wang S, Chen J, Wang Y, Yang Y, Zhang D, et al. (2019) Cigarette smoking is negatively associated with the prevalence of type 2 diabetes in middle-aged men with normal weight but positively associated with stroke in men. J Diabetes Res 1853018.
- Hou X, Qiu J, Chen P, Lu J, Ma X, et al. (2016) Cigarette smoking is associated with a lower prevalence of newly diagnosed diabetes screened by OGTT than non-smoking in Chinese Men with normal weight. PLoS One 11(3): e0149234.






























