Retroperitoneal Sarcoma. Case Report
García-Marín Gustavo E1, González-Luna Antonio1, Romero-Álvarez Katia1, Cervantes-Rojas Marisol1, Reséndiz-Paniagua Diego A1, Chávez-Ibarra Mario H1, Sánchez-Rosado Rodolfo R1 and Torres-Salazar Quitzia L*2
1Institute of Security and Social Services for State Workers, Mexico
2Biomedical Research Institute, Mexico
Submission:November 19, 2022; Published:December 01, 2022
*Corresponding author:Quitzia Libertad Torres Salazar, Biomedical Research Institute Alpha 0.01, Paloma Street No.812 Colonia Fátima CP 34060 Durango, Mexico
How to cite this article:García-Marín Gustavo E, González-Luna A, Romero-Álvarez K, Cervantes-Rojas M, Reséndiz-Paniagua Diego A, et al.Retroperitoneal Sarcoma. Case Report. Adv Res Gastroentero Hepatol, 2022; 19(1): 556005. DOI: 10.19080/ARGH.2022.19.556005.
Abstract
Background: Retroperitoneal sarcomas (RPS) are rare tumors associated with adverse prognosis. This is particularly true in cases of high-grade sarcomas of specific histologic subtypes, as has been demonstrated by major studies over the last decade. Diagnosis and treatment of RPS can be extremely difficult because symptoms are nonspecific and may appear only when the tumor is grossly enlarged. A complete removal is the only successful treatment for this tumor; 51.4% of these tumors can be completely removed, and 50.2% of these removals include adjacent organs. We present the case of a 70-year-old female with a diagnosis of retroperitoneal sarcoma.
Case Presentation: We present the clinical case of a 70-year-old woman who was referred to the surgical service for presenting an abdominal tumor under study. She has a positive paternal and maternal oncologic history, as well as a sister with breast cancer. The patient was admitted with a tomography study indicating the presence of a tumor in the retroperitoneum, with approximate dimensions of 25 x 30cm, heterogeneous, with irregular borders, vascularized appearance, which captures contrast material. The patient was programmed for excision of an adnexal tumor, resecting a 30 x 27cm mass that was dependent on the peritoneum, with implantation in the mesentery, parietal peritoneum and small intestine.
Conclusion: Retroperitoneal sarcoma is an uncommon diagnosis, with diffuse symptomatology in its early stages. It is extremely relevant for the specialist to consider its differential diagnosis, especially after the 6th decade of life. A multidisciplinary management is recommended due to the probable invasion of neighboring organs.
Keywords: Retroperitoneal sarcoma; Sarcoma; Soft tissue tumor; Radiotherapy; Systemic therapy
Introduction
Soft tissue sarcomas are biologically heterogeneous tumors arising from mesenchymal cells, particularly from fat, nerves, blood vessels, and connective tissues, with more than 100 subtypes [1]. Although sarcomas account for <1% of all adult malignancies, retroperitoneal sarcomas are a distinct subgroup, accounting for <15% of all sarcomatous tumors. There is no sex preponderance, and the incidence peak usually occurs in the fifth decade of life [2].
The retroperitoneum is broadly defined as an anatomical space located posterior to the peritoneal cavity. In general terms, it is delimited by the diaphragm in its upper part, the iliopsoas in its lower part, the paraspinous muscle in its medial part, the transversal fascia of the abdominal wall in its lateral part, and the psoas, the quadratus lumborum, the iliacus and the transversus abdominis muscle in its posterior part [3].
Sarcomatous tumors arising in the retroperitoneum often extend into retroperitoneal planes, and may invade or abut multiple retroperitoneal structures, making multivisceral resections a common feature [4].
The major blood vessels may be invaded by primary sarcomas arising from the vessel wall or by secondary infiltration of a retroperitoneal sarcoma. Major vessel involvement is not considered an absolute contraindication for surgical resection. The main issue in evaluating a possible major vascular resection is to balance the potential surgical morbidity with the expected survival benefit. This is strictly related to the biology and clinical behavior of the tumor and to the performance status and comorbidities of the patient [3].
Complete resection, which may require removal of multiple organs, represents the treatment chosen for RPS. Fairweather et al. [5] recently proposed categorization as a possible rationale for visceral resections, including: Suspected organ invasion or neoplastic origin, tumor affecting the vascular supply of end organs, tumor involving an organ with greater than 180 involvement, tumor adherence to organs, tumor adjacent to an organ or needing complete resection, microscopic (R0/R1 resection), other causes such as iatrogenic lesions requiring additional resection.
Case Presentation
We present the case of a 70-year-old woman, with a positive family history of oncological diseases (prostate and gastric) on the father’s and mother’s side respectively. The patient was evaluated with 100% Barthel functional capacity, independent in all activities of daily living and KATZ A up to 1 month prior to her evaluation by our service. She denies chronic diseases. The patient reported having undergone an appendectomy 30 years ago and a hysterectomy 11years ago; in both cases she required blood transfusion. She refuses exposure to biomass; exposure to chalkboard chalk for more than 20years by trade.
The patient was admitted to our hospital unit to study an abdominal tumor, which apparently extended from the peritoneal cavity to the retroperitoneum, measuring approximately 25 x 30cm, heterogeneous, with irregular borders, vascularized appearance, and contrast material uptake. Both renal units presented ureteropielocaliceal ectasia, with preserved corticomedullary relationship, predominantly right ectasia. Their azo levels were within normal parameters, GFR 54.8ml/min/1.73.
On physical examination, she presented good general condition with no cardiorespiratory alterations, the abdomen was globular due to abdominal distention and mass. Slightly decreased peristalsis was auscultated. The palpation procedure identified a pelvic hollow tumor of approximately 15cm of stony consistency, with no evidence of peritoneal irritation, vaginal examination was deferred at the patient’s request. Extremities symmetrical, integral, palpable peripheral pulses, immediate capillary filling, without edema.
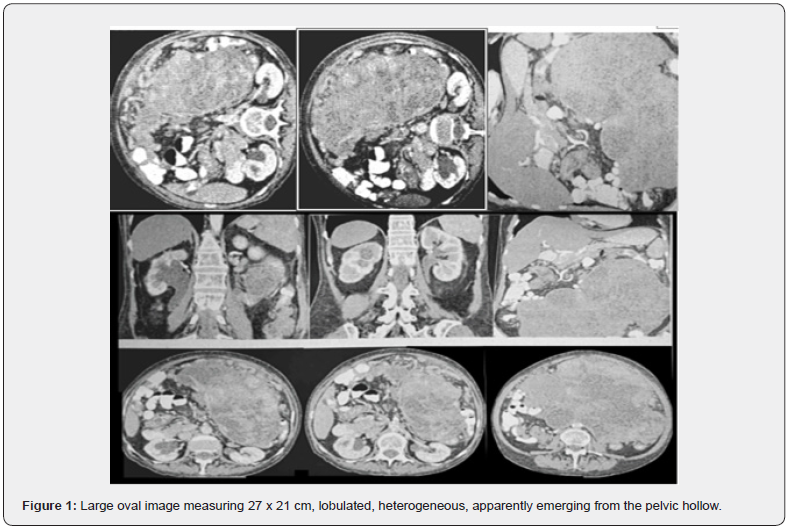
With the diagnosis of abdominal tumor under consideration, an abdomino-pelvic computed axial tomography (CAT) scan was indicated, which reported the following: In pelvic hollow bladder was observed with scarce repletion without lithos in its interior, as well as scarce free liquid, a large oval image was identified measuring 27 x 21cm, lobulated, heterogeneous, apparently emerging from the pelvic hollow. The CAT diagnosis was: large tumor covering the entire abdominal cavity to rule out possible ovarian tumor, measuring 27 * 21cm. Right renal ectasia due to ureteral compression. Chronic vesicular lithiasis, free fluid in pelvic hollow, arteriosclerosis (Figure 1). The patient is scheduled for excision of an adnexal tumor.
Surgical Technique
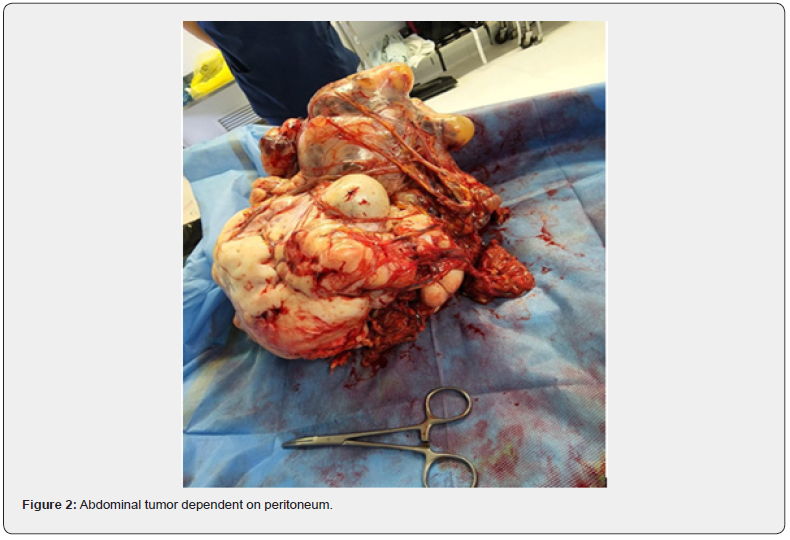
After aseptic and antisepsis, the patient was prepared with mixed anesthesia (general and peridural); she was positioned in dorsal decubitus and sterile fields were placed. A suprainfraumbilical midline incision of approximately 25 cm was made; it was dissected by planes until accessing the cavity, finding free liquid, from which a sample was taken for study. An abdominal tumor of approximately 30 x 27cm was identified, peritoneum-dependent, multilobulated of heterogeneous aspect, very vascularized and adhered to the omentum (Figure 2). Tumor resection was performed with metzenbaum scissors and bipolar energy, the vascular bundle was sealed with adequate hemostasis, managing to remove the tumor. The cavity revision was performed, finding implants in the mesentery, parietal peritoneum predominantly in the pelvic cavity and in the small intestine, finding distal ileum from the ileocecal valve. The cecal stump was closed with a double suture line using continuous surgete anchored with 3-0 vicryl and lembert stitches with 3-0 silk, a lateral end ileo-colonic anastomosis (ascending colon) was performed with connel and mayo stitches with 3-0 vicryl and lembert with 3-0 silk. The mesenteric gap was performed with 3-0 continuous surgete silk and hemostasis was verified. The hepatic gland was checked and found without macroscopic nodulations or metastasis data. Gauze and material were counted, and the aponeurosis was closed.
Discussion
In most cases, the diagnosis of retroperitoneal sarcoma is made by imaging findings during routine medical examination. The rest of the time, as in the case presented, patients are diagnosed because they manifest pain and/or increase in abdominal volume. It is necessary to perform imaging studies, even when signs and symptoms highly suggestive of abdominal tumor are identified, to establish the diagnosis and appropriate treatment, in addition to the importance of identifying whether the tumor is resectable or not, its size and its relationship with neighboring organs.
It is important for resection to be approached by multidisciplinary groups due to the probability of tumor adhesion to the different organs. In the case of our patient, it was necessary to resect a portion of the intestine and to perform a careful inspection to look for implants in underlying organs. Diamantis et al. [6] report that neoadjuvant or adjuvant radiotherapy is associated with better survival at five years. Roeder & Krempien [7] report that, with the combination of preoperative and perioperative radiotherapy, disease control at five years is achieved in 51-83% of cases.
References
- Schmitz E, Nessim C (2022) Retroperitoneal Sarcoma Care in 2021. Cancers (Basel) 14(5): 1293.
- Trans-Atlantic RPS Working Group (2015) Management of primary retroperitoneal sarcoma (RPS) in the adult: a consensus approach from the Trans-Atlantic RPS Working Group. Ann Surg Oncol 22(1): 256-263.
- Cananzi F, Ruspi L, Fiore M, Sicoli F, Quagliuolo V, et al. (2021) Major vascular resection in retroperitoneal sarcoma surgery. Surgery 170(3): 848-856.
- Dingley B, Fiore M, Gronchi A (2019) Personalizing surgical margins in retroperitoneal sarcomas: an update. Expert Rev Anticancer Ther 19(7): 613-631.
- Sbaraglia M, Bellan E, Dei T (2021) The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives. Pathologica 113(2): 70-84.
- Diamantis A, Baloyiannis I, Magouliotis D, Tolia M, Symeonidis D, et al. (2020) Perioperative radiotherapy versus surgery alone for retroperitoneal sarcomas: a systematic review and meta-analysis. Radiol Oncol 54(1): 14-21.
- Roeder F, Krempien R (2017) Intraoperative radiation therapy (IORT) in soft-tissue sarcoma. Radiat Oncol 12(1): 20.






























