Appendiceal Mucinous Neoplasm in Fourth Decade of Life. Report of a Case
García-Marín Gustavo1, Almada-Manzo Dianalaura1, Soto-Chaparro Marianne2, de la O-González Martín1, Monraz-Alvarez Daniel1, Leonher-Ruezga Karla1, Oropeza-Duarte César1 and Torres-Salazar Quitzia3*
1Institute of Security and Social Services for State Workers, Mexico
2Hospital Velmar, Ensenada Baja California, Mexico
3Universidad Juárez del Estado de Durango, Mexico
Submission:November 01, 2022; Published:November 08, 2022
*Corresponding author:Quitzia Libertad Torres Salazar, CEO of Biomedical Sciences Research Institute “Alpha 0.01”, Universidad Juárez del Estado de Durango, Calle Paloma No.812, Colonia Fátima, Durango, Mexico
How to cite this article:García-Marín G, Almada-Manzo D, Soto-Chaparro M, de la O-González M, Monraz-Alvarez D, et al. Appendiceal Mucinous Neoplasm in Fourth Decade of Life. Report of a Case. Adv Res Gastroentero Hepatol, 2022; 19(1): 556002. DOI: 10.19080/ARGH.2022.19.556002.
Abstract
Background: Appendiceal neoplasm has an incidence under 0.5% among all digestive tumors, and if it is not detected and treated on time, this tumor could be a potential precursor of peritoneal pseudomyxoma. Its clinical presentation can simulate other nosological entities, with acute symptomatology in right iliac fossa, so is usually made after histopathological study.
Case Presentation: A 45-year-old female patient is presented with pain in the right iliac fossa that, despite self-administration of non-steroidal analgesic, is persistent. She is admitted to the emergency department with clinical data of peritoneal irritation. Ultrasonographic studies were performed with diagnostic impression compatible with appendicular tumor, therefore surgical intervention was performed to remove the specimen. The histopathological diagnosis was appendiceal mucinous neoplasm.
Conclusions: It is necessary to establish the diagnosis of any appendicular tumor in order to reduce its progression. This, in order to avoid a higher risk lesion or to be confused with non-malignant neoplasms and thus, to be inadequately treated.
Keywords: Appendiceal tumor; Appendiceal mucinous neoplasm; Non-malignant neoplasms; Gastrointestinal tumors; Acute appendicitis; Mucinous cystadenoma; Mucinous neoplasm
Introduction
Appendiceal tumors constitute a heterogeneous group of neoplasms with an incidence ranging from 0.4 to 1% of all gastrointestinal tumors [1]. The most common age at onset is the sixth decade of life [2] and it is more frequent in males. Its presentation is variable, however, the most significant symptom is pain typically located in the right iliac fossa, so it is very common to confuse it with acute appendicitis [3]. Most appendiceal neoplasms are clinically silent and the diagnosis can only be made by formal histopathology. The clinical and pathologic characteristics are unusually varied compared to other gastrointestinal malignancies and require expert clinical judgment for optimal treatment [4]. The classification of appendiceal mucinous tumors (AMT) is controversial when they lack aspects of malignancy but are associated with peritoneal dissemination of mucin. Low-grade tumors confined to the appendix are clinically benign, whereas those that spread to the peritoneum may have a different clinical course. On the other hand, those tumors with appendiceal wall invasion or high degree of atypia, can have an aggressive evolution, and are considered adenocarcinomas [5]. According to the Pai and Longacre classification, AMT are divided into mucinous cystadenoma, mucinous neoplasm of uncertain malignant potential, mucinous neoplasm of low malignant potential, and mucinous adenocarcinoma [4]. It has been described that pseudomyxoma peritonei is present in more than 50% of these patients and its presence indicates higher stage and worse prognosis. This article presents a case of mucinous neoplasia of the appendix.
Clinical Case
The patient (female), aged 45 years, was originally from Zapopan, Jalisco, Mexico. No significant non-pathological personal history. Hemotype O Rh (+). Her parents have been diagnosed with type 2 diabetes; her mother also suffers from hypothyroidism, arterial hypertension, and glaucoma. The patient has a medical history of systemic arterial hypertension treated with telmisartan/hydrochlorothiazide She denies surgical interventions prior to the current condition. The patient started with symptoms 24 hours before attending the emergency service, presenting sudden abdominal pain (9/10 on the VAS-VISUAL ANALOGUE SCALE-). Initially, the pain was registered in right iliac fossa with subsequent irradiation to the hypogastrium, in addition to presenting intolerance to oral intake and constipation. Due to the symptoms described, the patient decided to selfmedicate (ibuprofen 800mg, single dose), which attenuated the pain for a few hours. However, when the symptoms persisted, she decided to go to emergency services. Once in the hospital unit, the patient was evaluated by surgical service, where vital signs were recorded within the normal range (BP 127/88mmHg, HR 90bpm, RR 18rpm, temperature 36.7°C). Physical examination revealed a globular abdomen with adipose panniculus, hypoactive peristalsis, involuntary rigidity, and the presence of pain on deep palpation in right iliac fossa (10/10 on the VAS scale). There was an indurated mass located in the hypogastrium and frank data of persistent peritoneal irritation, Blumberg (+), Rovsing (+), Obturator (+). The lower extremities retained their strength, temperature, coloration, and sensitivity, with motion and mobility well preserved. CAPRINI scale: High risk (6 points). A hemogram was performed, obtaining data within normal ranges, as well as liver and renal function tests. The studies were complemented with color doopler ultrasound and high-definition linear transducer in gray scale, focused on the right iliac fossa. A fixed loop with blind fundus was described, without peristalsis and vascularity, with an AP (anteroposterior) diameter of 8.1mm that does not modify upon compression, and a wall of 2.7mm. With the above data, the diagnosis of appendicitis with suspicion of appendiceal tumor was made, therefore surgical intervention was decided.
Surgical Technique
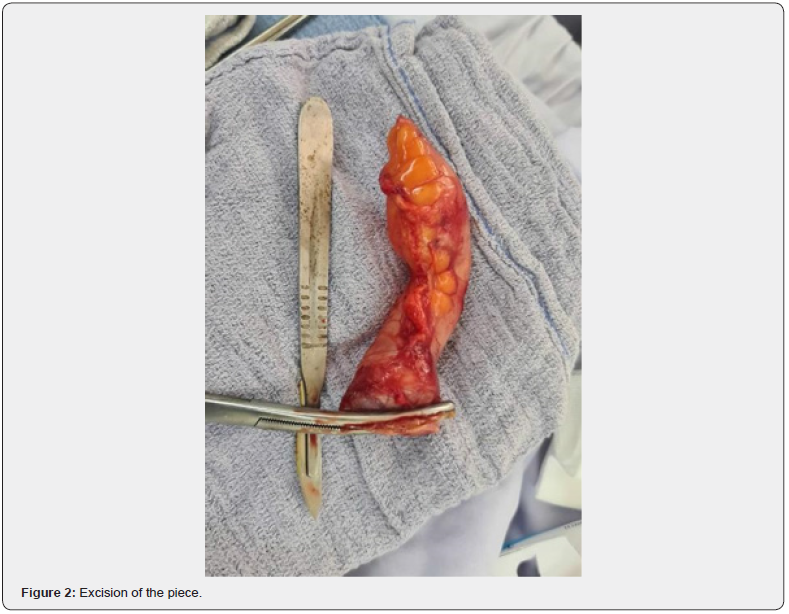
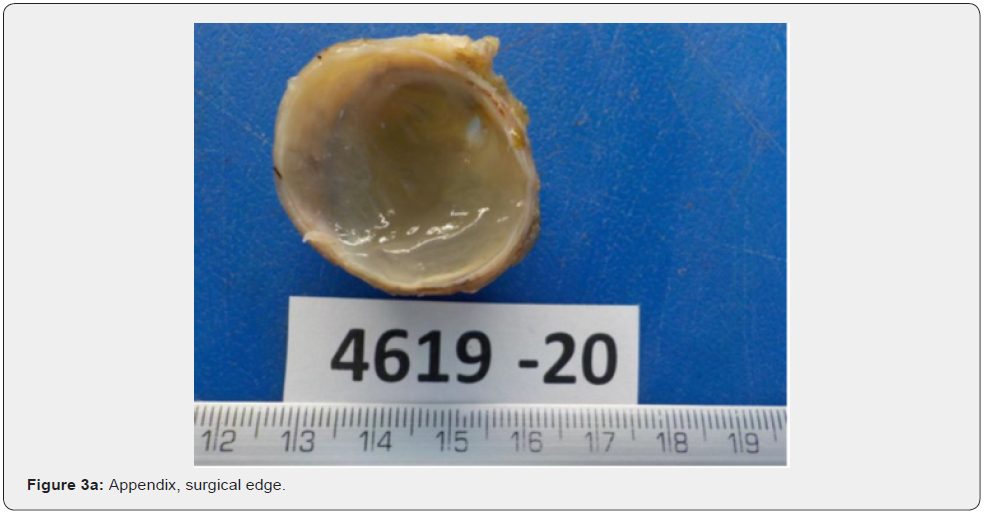
The procedure was performed after asepsis and antisepsis, with the patient in dorsal decubitus position. Under regional block, surgical fields were placed according to protocol. A 5cm long infraumbilical incision was performed, with deep plane dissection; non-foetid free fluid was found, with inflammatory characteristics. The appendix was aspirated and found in the midline, which, due to its length and characteristics, upon exposure, it was decided to extend the surgical incision 5cm supraumbilically. The appendix was found adhered to the abdominal wall and uterus; therefore, it was carefully separated with blunt dissection. The presence of a tumor was identified in the distal portion of the appendix, without compromising this organ. The mesoappendix was cut and ligated using 2-0 free silk and appendiceal resection was performed with a scalpel. The base was ligated with an atraumatic needle at point X and the base was imbricated with the Zuckerman technique. The cavity was washed with abundant warm saline solution, which was subsequently aspirated. A½ Penrose was placed directed to the pelvic hollow. Hemostasis was verified and the aponeurosis was closed with vycril 1 in continuous surge. Subcutaneous cellular tissue was washed with aquaseptic and faced with separate sutures (2-0 vycryl). Finally, the skin was closed with single suture (2-0 nylon) and the Penrose was fixed with the same material (Figures 1 & 2). The specimen was sent to the pathology service, who described the specimen as: tubular appendix with dimensions of 12.2x3.6cm, with a serous, smooth, light brown and vascularized surface. Upon cutting, there was an outflow of mucoid material, with a thinned wall, light brown color, and soft consistency (Figure 3a & 3b). The histological sections analyzed showed a dilated appendicular wall with simple and stratified epithelium of mucoproductive columnar cells. The cells are arranged on a fibrous wall showing a few lymphocytes and mucinous material is identified towards the lumen. The resection limits showed no alterations. No evidence of malignancy was observed, and the histopathologic diagnosis was low-grade appendiceal mucinous neoplasm.


Discussion and Conclusions
The appendix is an anatomical structure, which appears approximately in the eighth week of gestation. It is formed as a sac derived from the cecum that rotates during gestation to be in its medial position [6]. It can be found in different locations in the abdomen and pelvis, thanks to its descent during organogenesis [7]. Most appendicular neoplasms are silent. In the case of our patient, the diagnostic suspicion was made after the appearance of her symptomatology, with the support of ultrasonographic studies. The certain diagnosis was confirmed by histopathology, coinciding with what has been mentioned by other authors, who affirm that its diagnosis is mostly incidental [8]. On the other hand, the most reported discomfort is abdominal pain, which is present in more than 80% of the cases, as an acute appendicitis-like presentation with right lower quadrant pain due to distention of the appendix by mucin. Other symptoms are a palpable mass in the right iliac fossa, nausea, vomiting, weight loss, anemia, infertility, new onset umbilical or inguinal hernias, omental implants, intestinal obstruction and spontaneous rupture with generalized peritonitis [9]. Although the occurrence of these lesions is relatively low and the age reported is after the sixth decade of life, the possibility of their presentation in young adults should be considered at the time of establishing a diagnostic suspicion. This is mentioned by Suárez-Velázquez et al, who present a similar case in the fourth decade of life [10]. In contrast, Trujillo et al. [11] presented in 2018, a series of 36 cases of benign non-carcinoid neoplasms of the cecal appendix, reported during the last 17 years in a third level hospital; after reviewing a total of 4,910 surgical pieces the incidence of benign epithelial neoplasms was 0.073%, that is 7.3 cases per 10,000 surgical pieces analyzed, with an average age of 67 years. Hiroshi Takeyama et al. [12] conducted a retrospective study searching for prognostic-related factors, including the timing of lymph node dissection. Takeyama concluded that lymph node metastasis was an independent prognostic predictor after surgical resection with lymphadenectomy. They also describe that neither tumor depth nor histologic type were predictors of prognosis but were predictors of lymph node metastasis. Secondary lymphadenectomy, based on the pathologic findings of the resected specimens, is considered an acceptable surgical management with no worse prognosis than primary lymphadenectomy. This can be omitted in low-grade appendiceal mucinous neoplasm + G1 or in any tumor in situ and primary appendiceal tumor T1, a situation that corresponds to the case presented here according to the Staging Manual [13].
Finally, it is important to mention that, although appendiceal tumors until a few decades ago were very infrequent, their incidence has been increasing in recent years, so they should not be omitted in the differential diagnosis of pelvic masses. It was described mucinous neoplasms with uncertain malignant potential with the characteristics of low-grade tumors with acellular mucin in or beyond the appendiceal wall, so in this case, if an appendiceal tumor had not been suspected, there might have been progression to diffuse collections of gelatinous material in the abdomen and pelvis and spread into the peritoneal cavity which would have changed the prognosis and the therapeutic approach [13]. With its early recognition, unfortunate consequences at the operative level can be prevented, such as rupture and potential dissemination of malignant cells within the peritoneal cavity [14].
References
- Anisa-Nutu O, Marcacuzco-Quinto A, Manrique-Municio A, Justo-Alonso I, Calvo-Pulido J, et al. (2017) Tumores mucinosos del apéndice: incidencia, diagnóstico y tratamiento quirú 95(6): 321-327.
- Rouchad A, Gayet M, Bellin M (2014) Appendiceal mucinous cystadenoma. Diagn Interv Imaging 95(1): 113-116.
- Lai C, Yue C, Chen J (2013) Mucinous cystadenocarcinoma of the appendix mimics acute appendicitis. Clin Gastroenterol Hepat 11.
- Ploenes T, Börner N, Kirkpatrick J, Heintz A (2013) Neuroendocrine Tumour, Mucinous Adenocarcinoma and Signet-Ring Cell Carcinoma of the Appendix: Three Cases and Review of Literature. Indian J Surg 75 (Suppl 1): S299-S302.
- Darriba-Fernández M, Madrozo-Gonzalez Z, Aranda-Dausa H, Sanjuan-Garriga X, Hernández-Gañán X (2012) Mucinous appendiceal neoplasm. Do we all speak the same language? Rev Esp Enferm Dig 104(1): 44-45.
- Shankar S, Ledakis P, El Halabi H, Vadim Gushchin, Armando Sardi (2012) Neoplasms of the appendix: current treatment guidelines. Hematol Oncol Clin North Am 26(6):1261-1290.
- Zuluaga A, Sarmiento J, Cock A, Uribe R, Osorio L, et al. (2015). Mucionous Noeplasm of the Appendix. Rev Colomb Radiol 26: 1261-1290.
- Kelemouridou E, Mogrampi S, Tsavis G, Verroiotou M, Rallis T, et al. (2011) Mucinous cystadenoma of the appendix. A diagnostic dilemma? Chirugia 106: 251-254.
- Rymer B, Forsythe R, Husada G (2015) Mucocoele and mucinous tumours of the appendix:a review of the literature. Int J Surg. 18: 132-135.
- Suarez D, Oropeza C, Sol A, García K, García M, et al (2021) Appendiceal Mucinous Neoplasm. Cir y Cir, In Press, 95(6): 321-327.
- Trujillo-Díaz J, Ruiz-Soriano M, Solórzano-Aurusa J, Andrés-Asenjo B, Corrales-Cruz D, et al. (2019) Benign non-carcinoid neoplasms of the cecal appendix: presentation of 36 cases during the last 17 years in a third level hospital. Cir Cir 87: 630-635.
- Takeyama H, Murata K, Takeda T, Fujii M, Kagawa Y, et al. (2021) Clinical significance of Lymph node dissectio and lymph node metastasis in primary appendiceal tumor patients after curative resection: a retrospect multicenter cohort study. J gastrointest surg 26(1): 128-140.
- Shaib W, Assi R, Shamseddine A, Nese O, Memis B, et al. (2017) Appendiceal Mucinous Neoplasms: Diagnosis and Management. The Oncologist 22: 1107-1116.
- Hajiran A, Baker K, Jain P, Hashmi M (2014) Case of an appendiceal mucinous adenocarcinoma presenting as a leftadnexal mass. InJ Surg Case Rep 5(3): 745-749.






























