Outcome of Biofeedback in the Treatment of Intractable Constipation in Children with Dyssynergic Defecation
Vijay Mehta1, Jeffrey A Bornstein1,2,3, Devendra I Mehta1,2, Shaista S Safder1,2,3 and Yamen Smadi1*
1Center for Digestive Health and Nutrition, Arnold Palmer Hospital for Children, USA
2Clinical Assistant Professor of Pediatrics, Florida State University, USA
3Assistant Professor of Pediatrics, University of Central Florida, USA
Submission:August 30, 2021; Published:September 17, 2021
*Corresponding author:Yamen Smadi, Center for Digestive Health and Nutrition, Arnold Palmer Hospital for Children, Orlando Health, 60 W. Gore st. Orlando, FL 32806, USA
How to cite this article: Vijay M, Jeffrey A B, Devendra I M, Shaista S S, Yamen S. Outcome of Biofeedback in the Treatment of Intractable Constipation in Children with Dyssynergic Defecation.Adv Res Gastroentero Hepatol, 2021; 17(4): 555970. DOI: 10.19080/ARGH.2021.17.555970.
Abstract
Background/Aim: We aimed to study the efficacy of biofeedback on the clinical outcome and the manometric dynamics of children with dyssynergic defecation who failed aggressive conventional treatment for constipation.
Methods: We retrospectively reviewed the medical records of all patients who had dyssynergic defecation and underwent biofeedback. All patients failed conventional treatment of constipation for at least three months before they were referred to biofeedback. Sixty-nine patients (48 males), (Mean age 10±3, range 4-17 years) with dyssynergic defecation were included. Clinical outcomes after at least nine months from the last biofeedback session were assessed and were defined as “success” if the fecal frequency is more than two per week and the fecal incontinence is less than once every 2 weeks.
Results: Forty-six patients [66.6%] reported success of treatment. Biofeedback failed in treating 23 patients [33.3%]. In the “failure group”, 17 patients [24.6%] never experienced significant improvement and 6 patients [8.7%] reported initial improvement followed by relapse. Comparison of the Pre-Biofeedback and post-biofeedback manometric dynamics revealed significant improvement in first sensation volume, urge threshold, push pressure and balloon expulsion test [p<0.01]. After treatment, balloon expulsion test was normal in 24 patients (52%) of the success group compared to 1 patient (4.3%) of the failure group [p <0.0001].
Conclusion: Biofeedback results in resolution of symptoms in majority of children with dyssynergic defecation who failed traditional management of constipation at nine-month follow up.
Keywords: Children; Constipation; Dyssynergia; Biofeedback; Manometry
Introduction
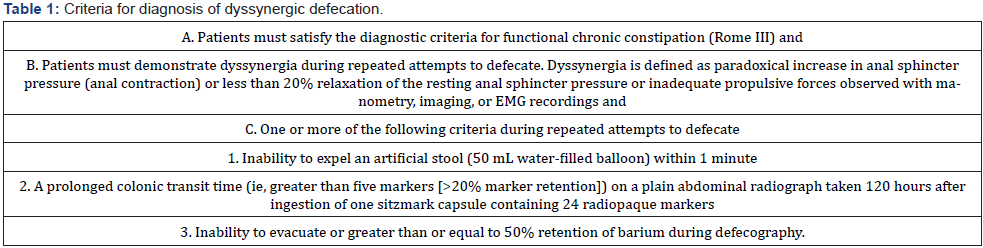
Functional constipation is a common disorder in children that accounts for 3% of visits to general pediatric clinics and up to 30% of visits to pediatric gastroenterologists [1]. Dyssynergic defecation (DD) defined as paradoxical contraction or failure to relax the pelvic floor and anal muscles during defecation, is present in 35% to 63% of constipated children [2-5]. Moreover, children with dyssynergia remains more frequently constipated at long-term follow-up than the other children with constipation (61% versus 29%) [6]. A diagnostic criteria for dyssynergic defecation was published by Dr. Rao in 2008 and has been widely used for diagnostic purposes (Table 1) [7].
The goal of biofeedback [BF] therapy in DD is twofold (1) to correct the dyssynergic function of the abdominal, rectal and anal sphincter muscles (i.e., to restore normal recto-anal coordination) and (2) to improve rectal sensory perception in patients with impaired rectal sensation [7]. Biofeedback uses electrical or mechanical devices to increase the awareness of physiological functions of anal sphincter by providing the patient with visual, verbal and/or auditory information and enhances self-control on body functions [8]. During biofeedback, patients are provided with visual graphs of their rectal pressure and also taught to relax external anal sphincter with the rise of rectal pressure [9].
In our tertiary institution, only those who failed conventional therapy that includes counseling, diet modification, medical treatment and behavioral therapy for at least three months are referred to BF. We aimed to study the efficacy of biofeedback on the clinical outcome and the manometric dynamics of children with dyssynergic defecation who failed aggressive conventional treatment for constipation.
Materials and Methods
After obtaining IRB approval, we retrospectively reviewed the medical records of all children who underwent anorectal biofeedback for dyssynergic defecation in Arnold Palmer hospital for Children between January 2010 and January 2014. Constipation was defined according to Rome III criteria [10]. Fecal incontinence term [FI] was used to describe soiling or encopresis events. Rao’s criteria [7] (Table 1) used to define dyssynergic defecation with one modification of using a 30ml air-filled balloon in the expulsion test.
Patients
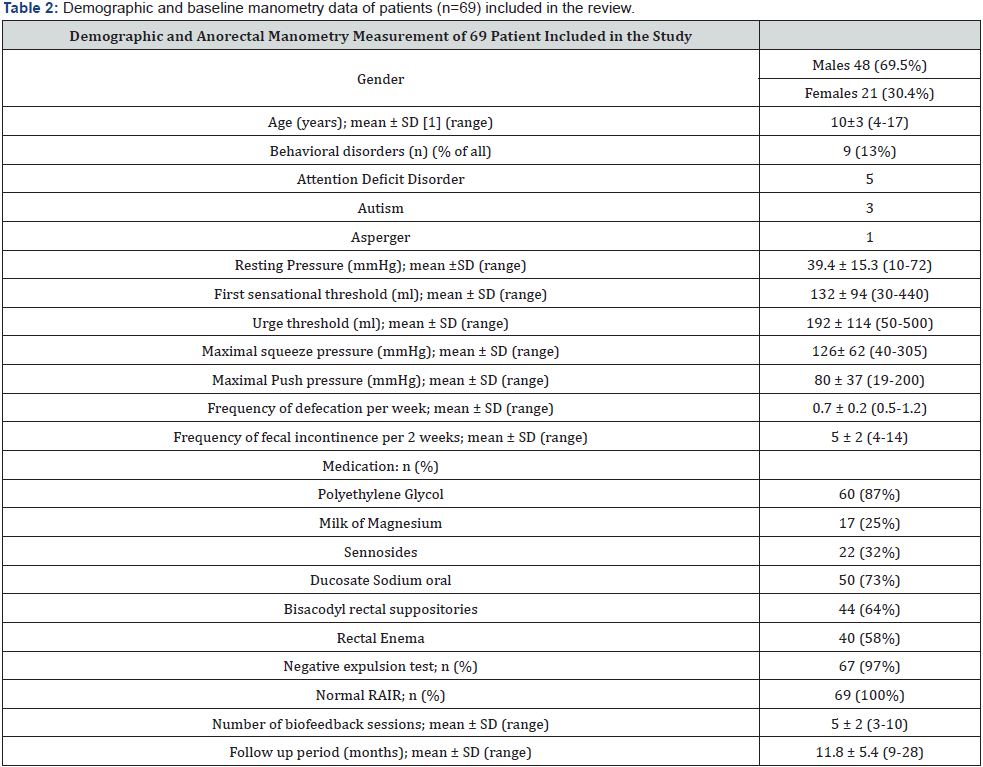
SD: Standard Deviation; 2RAIR: Rectoanal Inhibitory Reflex
Patients who were referred for biofeedback failed aggressive conventional treatment for constipation including stool diary, dietary modification, scheduled toilet training, stool softeners and laxatives for at least 3 months. Sixty-nine patients who met inclusion criteria were included in the analysis (Table 2).
Inclusion criteria
a) Children [0-18 years] who were diagnosed with DD by anorectal manometry and underwent biofeedback for treatment.
b) Biofeedback sessions are completed at least nine months before the chart was reviewed.
Exclusion criteria
a) Organic or anatomical cause of constipation
b) Surgical intervention for constipation such as cecostomy
Methods
Biofeedback: All patients underwent standard anorectal manometry [ARM] in the first session and rectoanal inhibitory reflex [RAIR] was documented. The 1st sensation volume threshold corresponds to the minimum volume felt in the rectum. The sensation of rectal fullness with a constant desire to defecate corresponds with the urge volume threshold. Maximal squeeze pressure is determined by asking the child to squeeze the sphincter complex as tight as possible without contracting abdominal muscles for 10 seconds. This maneuver is repeated few times. The maximum squeeze pressure is measured as the highest pressure during these efforts. Patients then are educated to push by asking to contract abdominal muscles, flex knees against abdomen and relaxing pelvic floor while intra-rectal and sphincter pressures are recorded and the push pressure is measured. For balloon expulsion test, the balloon is inflated with 50 ml of air and the child then is asked to defecate in left lateral position. If this does not occur within two minutes, 20 ml of air is withdrawn [leaving 30 ml] and the attempt is repeated. If defecation fails with 30 ml air-filled balloon, the expulsion test is recorded as abnormal. The physician then tries to assist defecation by applying slight traction for training purpose. Similarly, another 15ml is withdrawn if defecation still does not occur (leaving 15ml) and if this is still unsuccessful the equipment is removed.
Biofeedback sessions start with explaining the anorectal dysfunction and discuss its relevance with the patients and their parents before approaching the treatment. Patients are next shown anal manometry recordings displaying their anal function and are taught through trial and error to relax the pelvic floor and anal muscles during straining. This objective is pursued with the help of visual feedback on pelvic floor muscle relaxation coordinated with abdominal contraction, accompanied by continuous encouragement from the therapist [2,7,11-15]. Patients also are educated to practice toilet training at home by attempting a bowel movement at least twice a day, 30 minutes after meals, and to strain for no more than 5 minutes.
Data collection
We collected our data by reviewing the electronic medical records including clinical visit notes, phone notes and recorded notes during biofeedback sessions. Demographic data included age, sex and race. Clinical elements included frequency of defecation, fecal incontinence (soiling and/or encopresis), consistency and size of stool, pain during defecation, laxative medications use, and associated symptoms such as abdominal pain, appetite, and enuresis. We also recorded behavioral or psychological disorders such as Attention Deficit Disorder (ADD), Asperger disorder, Obsessive-Compulsive Disorder (OCD) and autism. This was reported based on medical history. All patients were asked to follow up with a clinic visit one month after the biofeedback sessions are completed. Our clinic staff contacted those who completed treatment to document long-term clinical outcome. We collected manometric dynamics before and after BF treatment including resting pressure, 1st sensation threshold, urge threshold, squeeze pressure, push pressure and balloon expulsion test.
Measures
Clinical outcomes after at least nine months from the last BF session were assessed and were defined as “success” if the fecal frequency is more than two per week and the fecal incontinence is less than once every 2 weeks. Balloon expulsion test was defined as normal if patient can expel 30ml air-filled balloon without assistance and abnormal if patient fails to do that with assistance. The balloon volume was decreased to 30 ml instead of 50ml to account for smaller size of pediatric patients.
Statistical analysis
Prevalence of clinical outcome improvement was calculated. The effect of balloon expulsion test on clinical outcome was measured by fisher test. T-test was used to compare manometric dynamics before and after BF treatment. The effect of gender and behavioral disorders as a risk factor on outcome was measured by using fisher test.
Results
Patient characteristics
From January 2010 till January 2014, seventy-nine patients underwent BF treatment. Ten patients were excluded for reasons explained in (Figure 1). Sixty-nine patients met inclusion criteria. Patients demographic data, constipation characteristics, medical management and baseline manometry dynamics are shown in (Table 2). There were more male patients [n= 48, 69.6%], and the mean age of our patient group was 10 [range 4-17 years]. Baseline pre-BF treatment manometric dynamics revealed elevated first sensation threshold and urge threshold and diminished maximum push pressure (Table 2). All patients except 2 failed 30ml air-filled balloon expulsion test (n=67, 96.5%). These 2 patients were included in our study due to clinical symptoms of intractable constipation and fecal incontinence and we included them to measure their response to biofeedback on clinical symptom of constipation and fecal incontinence. All patients met Rome III criteria for constipation and all patients had daily faecal incontinence at presentation. All 69 patients underwent 3 or more BF sessions [mean 5, range 3-10]. Average follow-up period was 11.8 months [range 9-28months].
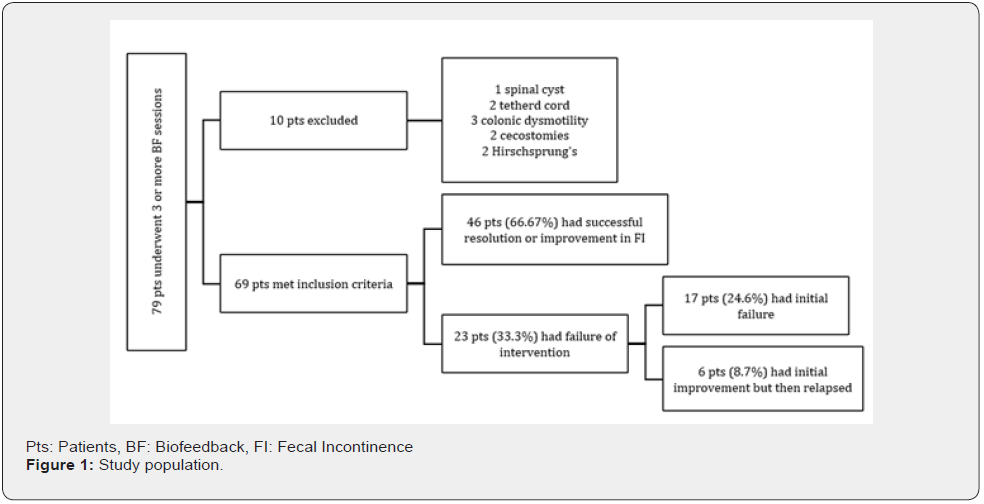
Clinical outcome
Forty-six patients [66.66%] reported success of treatment. Average FI frequency in the success group was once every 21 days (range: 17-60 days) and average fecal frequency in the success group was 3 bowel movements per week (range: 2-5 per week). In 23 patients [33.33% of all] BF failed in treating constipation; Among them 17 patients [24.6% of all] never experienced significant improvement in their symptoms and 6 patients [8.7% of all] reported initial improvement then relapsed symptoms.
Manometric dynamics
Pre-BF and post-BF manometric dynamics were compared using T-test. The comparison revealed significant improvement in first sensation threshold, urge threshold and push pressure. Squeeze pressures, pre and post BF, were not significantly different. (Table 3 & Figure 2) show detailed results of the pre and post BF dynamics. There was significant difference in all dynamics between success and failure group (p < 0.01).
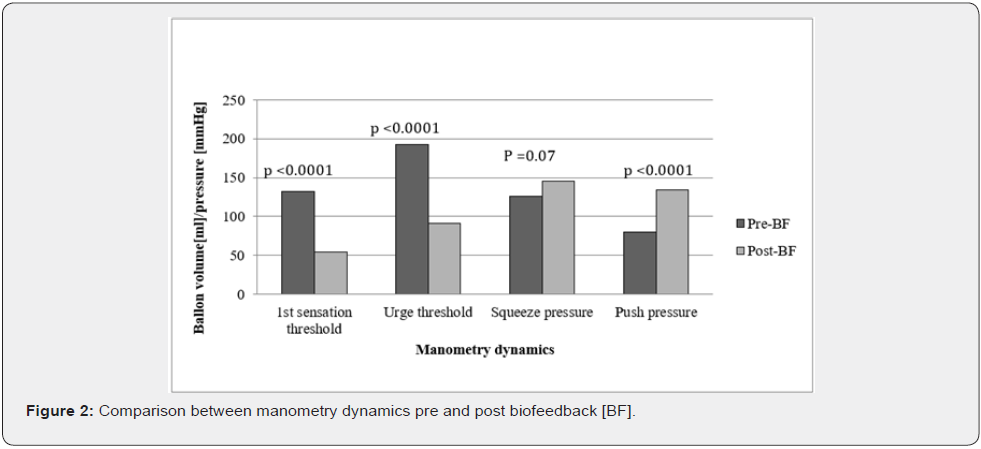
Balloon Expulsion Test: Balloon expulsion test was normal in 2 patients (2.8% of all) before BF compared to 25 patients (36% of all) after BF (p < 0.01). After BF treatment, balloon expulsion test was normal in 24 patients (52%) of the success group compared to 1 patient (4.3%) of the failure group [p <0.0001, CI 95%], [Relative Risk 1.9 (1.37-2.08)].
Influencing factors on success of treatment
Gender and outcome: 33 male patients (69%) compared to 13 female patients (56.5%) reported successful intervention [p=0.59, CI 95%]. On the other hand, after BF treatment, 15 male patients had positive expulsion test compared to 10 female patients [p=0.276, CI 95%]. The above results indicate no significant effect of gender on clinical outcome or on expulsion test.
Behavioral disorders: Behavioral disorders such as ADD, autism and Asperger disorders, were more common in the failure group compared to the successful group (21.7% vs. 8.6% respectively). However, that was not statistically significant [p 0.148, CI 95%].
Discussion
10-year retrospective study on 264 children with Chronic Constipation found that >30% of patients experienced persistent symptoms for >2 years and a prominent psychiatric burden despite aggressive laxative therapy [16]. These findings suggest that better treatments are needed rather than laxatives alone, the present standard of care [17], and that recognition of dyssynergic defecation and the use of biofeedback might improve the quality of life of children with intractable constipation.
Our experience is that biofeedback is effective most of the time in improving both clinical and defecation dynamic outcomes in children treated for dyssynergic defecation. In contrast to most of the trials discussed below, which compared conventional treatment to biofeedback, our practice is to refer patients for biofeedback only if they fail aggressive conventional treatment, therefore our population is different from most of studies done before. In our study, BF was effective in treating children with DD in two thirds of the cases and BF resulted in significant improvement in manometric dynamics and clinical outcome correlated with normalization of balloon expulsion test. Behavioral disorders were more common in patients who failed to respond to treatment but that was not statistically significant. Normal expulsion test was significantly more common in patients who had improvement in their symptoms [p<0.0001]. However, 48% of patients in this group continued to fail the test despite their improved clinical outcome. One explanation is that we perform the expulsion test in lateral position instead of physiologic sitting position. In contrast to Minguez et al. [13] who found that 9 out of 10 patients who failed balloon expulsion test were female, our study found that gender was not a risk factor for neither abnormal balloon expulsion test nor clinical outcome. In adults, several randomized trials comparing BF to either placebo or alternative strategies (e.g., laxatives, sham BF) reported outcomes favoring BF. The response rates in randomized control trials of BF ranged from 53% to 75% [18]. Chiarioni et al. [18] conducted a literature review on efficacy of BF for DD and concluded that functional defecation disorder, one of the most frequent and disabling subtypes of adult constipation, can be treated effectively with biofeedback training. This improvement was sustained at 12 and 24 months [2,19] due to a change in underlying pathophysiology. Moreover, biofeedback therapy was recommended for the short-term and long-term treatment of constipation and fecal incontinence with dyssynergic defecation in the most recent position paper published by Rao et al. [20].
However, the efficacy of BF in treating children with DD varies in pediatric literature. In 1987, Wald et al. compared biofeedback therapy with mineral oil in a group of 55 encopretic children; 16 of whom showed evidence of functional defecation disorder. Although a trend toward greater improvement in the biofeedback group was evident, the difference in success rate did not reach significance [21]. In another controlled study, a well-defined pediatric population of 43 children with functional defecation disorder was randomized to receive biofeedback therapy plus conventional care (laxatives) or conventional treatment only. The biofeedback group did significantly better than the conventional one, with about half of patients showing successful symptoms resolution at one year follow-up compared to 16% in the conventional-care-only group. The clinical benefit was correlated with normalization of defecation dynamics [2,22]. Similar benefits were reported in another controlled study in pediatric population, but the follow-up was too short (3 months) [2,23]. Another small trial evaluating the effects of biofeedback found that all children learned to relax the external anal sphincter after five sessions of biofeedback [24].
In contrast to the successful studies described above, the largest randomized, controlled study in pediatric constipation (192 children), which compared laxatives plus Electromyogram [EMG] biofeedback therapy to laxatives alone, failed to show any benefit from biofeedback.4 However, a criticism of this study was that not all the subjects had functional defecation disorder.2 Twenty-one randomized trials with a total of 1371 children were reviewed by Brazziel et al. [25] and published as a Cochrane review in 2011. The authors concluded that there is no evidence that biofeedback training adds any benefit to conventional treatment in the management of functional faecal incontinence in children. However, sample sizes were generally small and interventions varied amongst trials and few outcomes were shared by trials addressing the same comparisons.
Our study included patients with DD exclusively and excluded other pathologies for constipation, which was necessary to study the effect of BF on those patients. The discrepancy between adult and pediatric literature on one hand and among pediatric publications itself is not well explained. Furthermore, trials studying the effect of biofeedback in dyssynergic defecation in children are limited and other options of treatment are not well defined [11,26]. The results of our study support favorable outcome with BF for treating children with DD if they fail conventional management of constipation.
Limitations
This is a retrospective review of children with DD who underwent treatment with BF. Three pediatric gastroenterologists performed manometry and BF sessions. The later might have resulted in variation in interpreting manometry results. Thought it is not studied in pediatrics, we think that performing the balloon expulsion test in a lateral position might affect the results of the test.
Acknowledgements
We would like to acknowledge our motility nurse Kathy Pueschel, RN for her help in data entry.
References
- Partin JC, Hamill SK, Fischel JE, Partin JS (1992) Painful defecation and fecal soiling in children. Pediatrics 89: 1007-1009.
- Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G (2006) Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology 130(3): 657-664.
- Benninga MA, Buller HA, Taminiau JA (1993) Biofeedback training in chronic constipation. Arch Dis Child 68: 126-129.
- van der Plas RN, Benninga MA, Buller HA, P M Bossuyt, L M Akkermans, et al. (1996) Biofeedback training in treatment of childhood constipation: a randomised controlled study. Lancet 348(9030): 776-780.
- Loening-Baucke V, Cruikshank B, Savage C (1987) Defecation dynamics and behavior profiles in encopretic children. Pediatrics 80(5): 672-679.
- Michaud L, Lamblin MD, Mairesse S, Turck D, Gottrand F (2009) Outcome of functional constipation in childhood: a 10-year follow-up study. Clin Pediatr (Phila) 48: 26-31.
- Rao SS (2008) Dyssynergic defecation and biofeedback therapy. Gastroenterol Clin North Am 37(3): 569-586.
- Loening-Baucke V (1996) Biofeedback training in children with functional constipation. A critical review. Dig Dis Sci 41: 65-71.
- Rajindrajith S, Devanarayana NM (2011) Constipation in children: novel insight into epidemiology, pathophysiology and management. J Neurogastroenterol Motil 17: 35-47.
- Hyman PE, Milla PJ, Benninga MA, Davidson GP, Fleisher DF, et al. (2006) Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology 130: 1519-1526.
- Bongers ME, Tabbers MM, Benninga MA (2007) Functional nonretentive fecal incontinence in children. J Pediatr Gastroenterol Nutr 44: 5-13.
- van Ginkel R, Buller HA, Boeckxstaens GE, van Der Plas RN, Taminiau JA, et al. (2001) The effect of anorectal manometry on the outcome of treatment in severe childhood constipation: a randomized, controlled trial. Pediatrics 108: E9.
- Minguez M, Herreros B, Sanchiz V, Vicent Hernandez, Pedro Almela, et al. (2004) Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology 126(1): 57-62.
- Andromanakos N, Skandalakis P, Troupis T, Filippou D (2006) Constipation of anorectal outlet obstruction: pathophysiology, evaluation and management. J Gastroenterol Hepatol 21: 638-646.
- Nolan T, Catto-Smith T, Coffey C, Wells J (1998) Randomised controlled trial of biofeedback training in persistent encopresis with anismus. Arch Dis Child 79: 131-135.
- Sonnenberg A, Koch TR (1989) Physician visits in the United States for constipation: 1958 to 1986. Dig Dis Sci 34: 606-611.
- Belkind-Gerson J, Goldstein AM, Kuo B (2013) Balloon expulsion test as a screen for outlet obstruction in children with chronic constipation. J Pediatr Gastroenterol Nutr 56(1): 23-26.
- Jodorkovsky D, Dunbar KB, Gearhart SL, Stein EM, Clarke JO (2013) Biofeedback therapy for defecatory dysfunction: "real life" experience. J Clin Gastroenterol 47(3): 252-255.
- Rao SS, Valestin J, Brown CK, Zimmerman B, Schulze K (2010) Long-term efficacy of biofeedback therapy for dyssynergic defecation: randomized controlled trial. Am J Gastroenterol 105: 890-896.
- Rao SS, Benninga MA, Bharucha AE, Chiarioni G, Di Lorenzo C, et al. (2015) ANMS-ESNM position paper and consensus guidelines on biofeedback therapy for anorectal disorders. Neurogastroenterol Motil 27: 594-609.
- Wald A, Chandra R, Gabel S, Chiponis D (1987) Evaluation of biofeedback in childhood encopresis. J Pediatr Gastroenterol Nutr 6(4): 554-558.
- Loening-Baucke V (1990) Modulation of abnormal defecation dynamics by biofeedback treatment in chronically constipated children with encopresis. J Pediatr 116(2): 214-222.
- Sunic-Omejc M, Mihanovic M, Bilic A, D Jurcić, B Restek-Petrović, et al. (2002) Efficiency of biofeedback therapy for chronic constipation in children. Coll Antropol 26 Suppl: 93-101.
- Croffie JM, Ammar MS, Pfefferkorn MD, Debra Horn, Ann Klipsch, et al. (2005) Assessment of the effectiveness of biofeedback in children with dyssynergic defecation and recalcitrant constipation/encopresis: does home biofeedback improve long-term outcomes. Clin Pediatr (Phila) 44(1): 63-71.
- Brazzelli M, Griffiths PV, Cody JD, Tappin D (2011) Behavioural and cognitive interventions with or without other treatments for the management of faecal incontinence in children. Cochrane Database Syst Rev 1(12): CD002240.
- Tabbers MM, Boluyt N, Berger MY, Benninga MA (2010) Constipation in children. Clin Evid (Online).






























