Helicobacter Pylori among Iraqi Patients with Central Serous Chorioretinopathy
Alyaa Abood Kareem1*, Giyathaldeen TH Neamah2, Mohammed Abed Abdulhussein1 and Zaid Ayed Kareem1
1University of Kufa, Faculty of medicine, Iraq
2Jabir Ibn Hayyan Medical University, Iraq
Submission:May 17, 2021; Published:June 21, 2021
*Corresponding author: Alyaa Abood Kareem, University of Kufa, Faculty of medicine, Iraq
How to cite this article: Alyaa Abood K, Giyathaldeen TH N, Mohammed Abed A, Zaid Ayed K. Helicobacter Pylori among Iraqi Patients with Central Serous Chorioretinopathy. Adv Res Gastroentero Hepatol, 2021; 17(2): 555960. DOI: 10.19080/ARGH.2021.17.555960.
Abstract
Purpose: To determine the prevalence of Helicobacter pylori among patients with Central serous chorioretinopathy and effect of its eradication on signs and symptoms of the disease.
Patients and methods: This is a case control study which was conducted at Ibn-Al Haitham Teaching Eye Hospital during the period from July 2017 to June 2018 Eighty-eight Participants (20-59 years of age) were divided into two groups: Group (A) 38 patients diagnosed to have Central serous chorioretinopathy on basis of clinical ophthalmological examination and macular optical coherence tomography. In addition, group (B) including 50 healthy control subjects with normal ophthalmological examination. All participants were sent for urea breath test to detect Helicobacter pylori, those with positive results were referred for eradication of Helicobacter pylori, and reassessment was done at 4-6 weeks for all subjects with Central serous chorioretinopathy.
Result: The prevalence of Helicobacter pylori among patient’s in-group (A) was (68.4%) while in-group (B) was (42%). The majority of those patients’ in-group (A) (92%) showed symptomatic response to eradication of Helicobacter pylori infection and only (7.7%) did not respond.
Conclusion: Helicobacter pylori could be a risk factor for Central serous chorioretinopathy and successful eradication of Helicobacter pylori can improve the common signs and symptoms of Central serous chorioretinopathy.
Keywords: CSCR, H. pylori; Central serous chorioretinopathy; Infection
Introduction
Central serous chorioretinopathy (CSCR) was first describe by Von Graefe in 1886 [1]. it is an idiopathic disorder characterized by localized serous detachment of sensory retina at macula secondary to leakage from the choriocapillary through one or more hyperpermeable retinal pigmented epithelium (RPE) sites [2]. It commonly affects young men (between 25-45) years old, unilateral in (80-90%) patient usually complain of blurred vision, central positive scotoma, micropsia, metamorphopsia, and impaired color vision [3,4]. the disease has spontaneous resolution with good visual prognosis, but recurrence occur in 50% or more of cases, Small percentage of cases may develop chronic course [5].
Pathophysiology of CSCR is poorly understood. Possible theories include choroidal hyperpermeability due to ischemia, stasis or inflammation, which overcome the RPE pumping mechanism responsible for keeping the subretinal space dry [6,7]. RPE dysfunction is another theory for developing CSCR in which focal damage of adjacent RPE cells or even a single RPE cell leads to reversal of ion pumping mechanism and resulting in fluid accumulation in the subretinal space [8]. An alternative theory is a combined choroidal and RPE dysfunction. [9] Several risk factors associated with CSCR such as steroid administration stress, personality type A, sildenafil Obstructive sleep apnea, systemic hypertension, Cushing disease, pregnancy, H. pylori and systemic lupus erythematosus [5].
There is no effective treatment of CSCR; most of cases resolve spontaneously within 1-6 months, Micro pulse diode laser to the site of leakage has shown good response, PDT 30-50% of the dose with 50% light intensity leads to complete resolution. AntiVEGF may show some promise. Other treatment including aspirin, mifepristone and eplerenone [2].
Helicobacter pylori (H. pylori) is one of most common causes of gastrointestinal infection worldwide. It is gram negative, spiral shape, flagellated bacteria, associated with many digestives and extra digestive pathogens for human. The digestive diseases include gastritis, duodenal ulcer gastroesophygeal reflex, gastric cancer, anorexia. The extra digestive disease includes atherosclerosis, cardiovascular disease, Parkinson disease, autoimmune thyroiditis, urticaria, rosacea, and (eye diseases) including glaucoma, blepharitis, sjogren disease, uveitis and CSCR [10-13]. There are invasive and noninvasive technique to diagnose the H. pylori, the invasive requiring endoscopy and biopsy for histological examination and culture. The non-invasive include urea breathe test (which is the most sensitive and specific test), serum antibodies to H. pylori, stool antigen [14].
Recently, the relation between H. pylori and central serous Chorioretinopathy has been documented, it’s thought that antibodies Against H. pylori antigen cross- react with vascular wall antigens lead to damage of arterial cell wall and development of atherosclerosis and microangiopathy [15]. The clinical application of this relation is yet to be emphasized and the role of its eradication is better to be included in the Symptomatic management of CSCR.
Aim of the Study
To evaluate the relationship between CSCR and H. pylori, and the effect of H. pylori eradication on course of CSCR.
Patients and Methods
This is a case control study that was conducted at Ibn- Alhaitham Teaching eye Hospital from July 2017 to June 2018 where 88 participants are included in this study divided into two groups: Group (A) which included Thirty-eight patients recently diagnosed with CSCR and Group B (50) Subjects with normal ophthalmological examination considered as control group. All individuals underwent a full medical history and ophthalmological history and examination including (best corrected visual acuity by Snellen chart, Amsler grid, slit lamp biomicroscopic examination dilated fundus examination by non-contact 90D double aspheric condensing lens. Suspected patients with CSCR were examined by optical coherent tomography (OCT) to confirm the diagnosis of CSCR. All participants were sent for urea breath test to detect H. pylori infection, the patients with positive urea breath test were referred for medical consultation for eradication of H. pylori infection and follow up after 4-6 weeks for ophthalmological symptoms (blurred vision, micropsia, metamorphopasia, and scotoma) and signs (sub retinal fluid) by repeat the OCT and microbial laboratory re-examination (urea breath test). A verbal informed consent was obtained from all patients before urea breath test and before starting the treatment (Use of topical and systemic steroid, Smoking, pregnancy, renal failure, hypertension, SLE, diabetic retinopathy, sildenafil) were excluded.
Statistical analysis
SPSS® Software (version 23.0 for Linux®) was used to perform statistical analysis. Qualitative data are presented as numbers and percentages, and continuous numerical data are presented as mean ± standard deviation. Comparison of study groups was carried out using chi- square test for categorical data and using Student’s t-test for continuous data. P value of < 0.05 was considered statistically significant.
Results
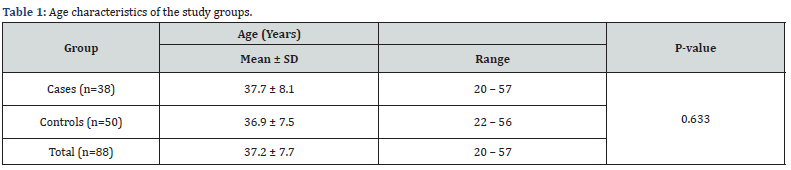
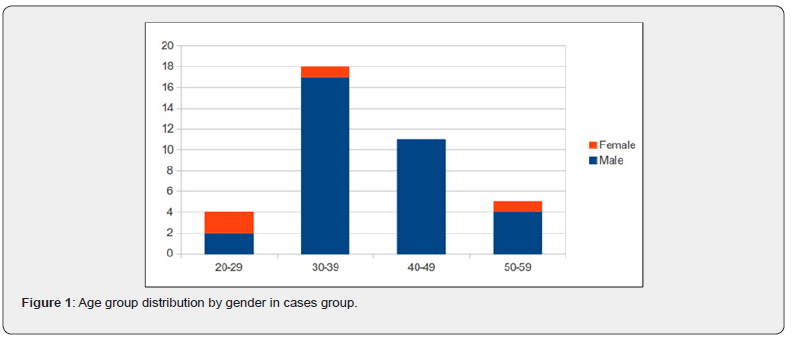
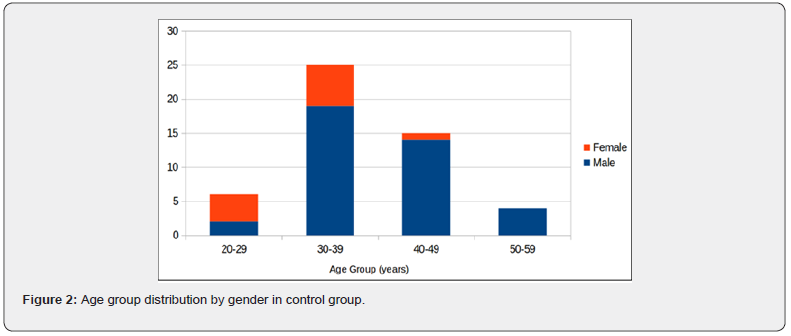
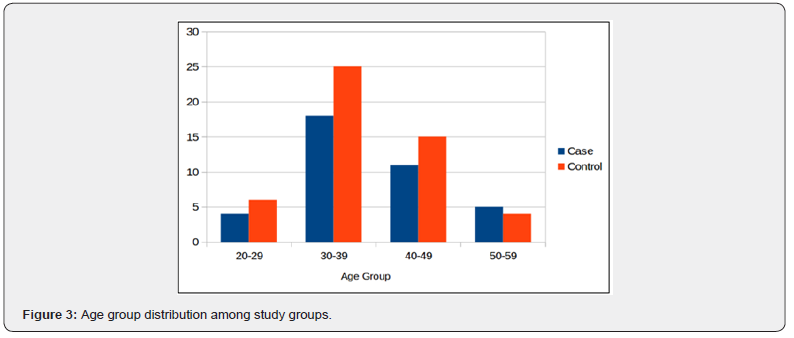
This study included 88 participants: 38 patients diagnosed with central serous chorioretinopathy (CSCR) and 50 healthy controls, all underwent urea breath test for detection of presence of H. pylori. Males comprised 89.5% of the group (A) while females comprised 10.5%; compared to 78.0% males and 22.0% females in the group (B). Age characteristics of the study groups are described in (Table 1). No statistically significant difference was found regarding the age across males & females, a represent that age of patients group is comparable between the two genders. Age group distribution for cases group is summarized in (Figure 1), while age group distribution for control group is summarized in (Figure 2). The right eye examined involved 57.9% of the patients while the remaining 42.1% patients had their left eye examined (Figure 3).
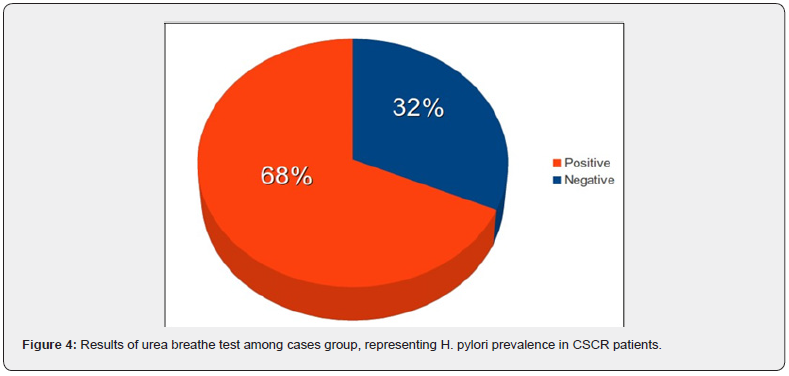
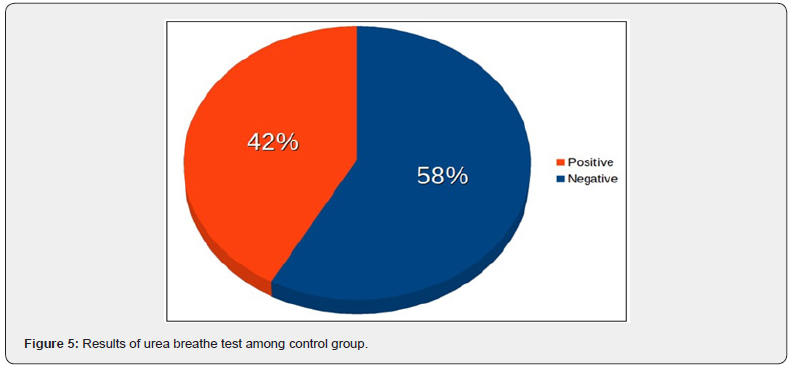
Prevalence of H. pylori in cases group as indicated by the results of urea breath test is found to be 68.4%, with a total positive results of 26 out of 38 (Figure 4), while the prevalence in control group was 42.0%, with a total positive results of 21 out of 50 controls (Figure 5). Status of H. pylori infection by gender in cases group is summarized in (Table 2). No statistically significant difference has been found regarding H. pylori infection across gender. Table 3 compares status of H. pylori infection across gender in controls group.
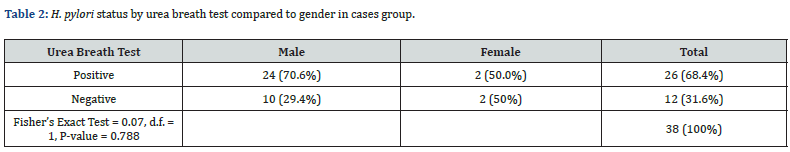
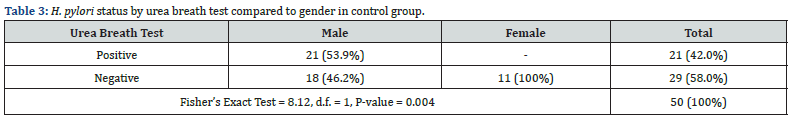
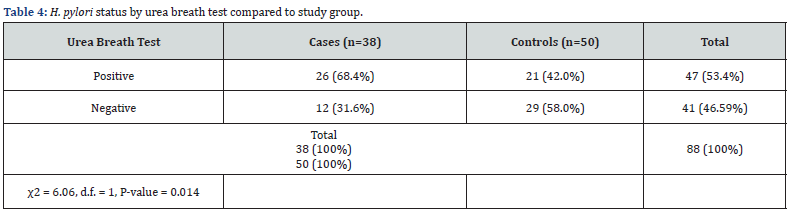
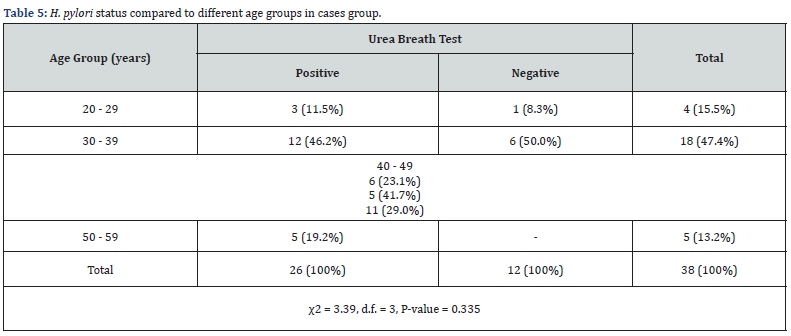
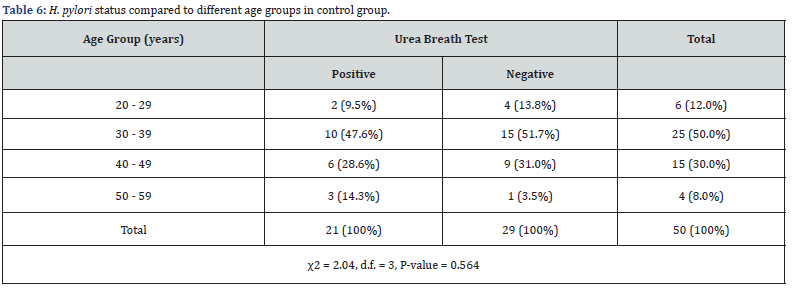
Comparison between cases and controls have demonstrated that there is a statistically significant difference between the two groups regarding H. pylori status, P-value=0.014 (Table 4). Odds ratio was 2.99 with 95% confidence interval of (1.23-7.25). Comparison of different age groups in the cases group regarding H. pylori status is summarized in (Table 5). No significant difference was found between the different age groups in cases group. A similar comparison was performed for control group, similarly no significant difference was observed between the different age groups of the controls (Table 6).
Patients who tested positive for urea breath test have underwent eradication of H. pylori, then CSCR condition was reassessed clinically and by OCT. The majority (92.3%) of those patients have shown improvement in the symptoms of the disease and decrease in sub retinal fluid while the remainder (7.7%) has shown no improvement (Figure 6).
Discussion
In view of the list of risk factors for the development of CSCR, ideas of targeting or controlling extraocular possible causes for the problem are to be thought of H. pylori infection of the digestive system has been pointed as a risk for CSCR, but its eradication is not a fixed protocol in the disease management. This study utilized Iraqi patients recently diagnosed to have CSCR to determine the prevalence of H. pylori in the upper digestive system depending of the urea breath test. It was found that (68.4%) of CSCR, patients had these bacteria; compared to the 42% positive results in the control group the finding was statistically significant.
This agree with a study conducted in Spain by Asensiosanchenz et al. [16] who observed that 68.75 % of patient with CSCR infected with H. pylori comparing to with 30 % of control. Similarly, In Iran, Feghhi et al. [17] found 68.5% of patient with CSCR have H. pylori positive, which was higher than the rate of control people. And Roshani et al. [18] reported a much higher prevalence of H. pylori in patients with CSCR than in control group. Another study conducted in Poland by Misiuk Hojlo, et al. [19] reported that H. pylori detected in 67.0% of total patients with CSCR comparing with 47.0% of control. An Italian study by Cotticelli et al found 78.2% of patients with CSCR have H. pylori positive while control group reported only 43.5% [20]. Another study have been done in France on patients with chronic CSCR by Mauget-Faysse et al. [21] they found (56.3%) of patient were H. pylori positive comparing with general French population 27.5%. While a study done in New York – USA by Warrow et al. [22] showed lower prevalence of H. pylori infection in patient with CSCR.
After successful medical eradication of H. pylori as proven by repeating the urea breath test, the CSCR patients VA, symptoms like (micropsia, metamorphopsia were improved and decrease of sub retinal fluid was noted. the same was seen in study done in France by Abnoux- Zabsonre which reported that improvement of the symptoms and signs was associated with complete eradication of H. pylori [23]. Roshani et al. [18] note that the symptoms of patients with CSCR get better after successful eradication of H. pylori. Also, Casella et al. [24] reported eradication of H. pylori could improve the V.A of patient with CSCR. Rahbani- Nobar et al. [25] found the reabsorption time of SRF in H. pylori eradication group a much shorter compare with the control Group but Dang et al found in his study H. pylori eradication neither improve the VA nor decrease sub retinal fluid [5].
The exact relation between H. pylori and CSCR is not fully understood It has been suggested that H. Pylori cytotoxin associated gene A (cag A) Increase the risk of atherosclerosis because anti-cag A antibody cross React with vascular cell wall antigen stimulating immunological reactions that cause damage of the arterial cell wall and development of Atherosclerosis [17,26]. In addition, IgG response to H. pylori infection act as another risk factor for endothelial dysfunction that may induce ischemia [27] these mechanisms might be part of pathophysiology of CSCR and explain the relation between H. pylori and vascular endothelial disorders like CSCR and coronary artery disease [28]. Age and sex showed no significant effect on the prevalence of H. pylori infection among patients with CSCR or the control group except in the sex.
Conclusion and Recommendations
Conclusion
H. pylori infection is risk factors for CSCR and eradication of these bacteria could be beneficial for improvement of signs and symptoms.
Recommendations
a) Larger sample study.
b) Study unilateral VS bilateral cases and chronic VS acute or recurrent cases in relation to the association with H. pylori may uncover further facts about the association.
For management of patients with CSCR a vital step to be considered is looking for the possible association of H. pylori infection and proper medical eradication in cooperation with the physician is encouraged to speed up the recovery.
References
- Mateo-Montoya A, Mauget-Faÿse M (2014) Helicobacter pylori as a risk factor for central serous chorioretinopathy: literature review. World journal of gastrointestinal pathophysiology 5(3): 355.
- Bowling B (2016) Kanski's Clinical Ophthalmology eight editions, chapter 14. Aquired macular disorder, pp. 624-627.
- Iida T, Yannuzzi LA, Spaide RF, Borodoker N, Carvalho CA, et al. (2003) Cystoid macular degeneration in chronic central serous chorioretinopathy. Retina 23(1): 1-7.
- Teschner S, Noack J, Birngruber R, Schmidt-Erfurth U (2003) Characterization of leakage activity in exudative chorioretinal disease with three- dimensional confocal angiography. Ophthalmology 110(4): 687-697.
- Dang Y, Mu Y, Zhao M, Li L, Guo Y, et al. (2013) The effect of eradicating Helicobacter pylori on idiopathic central serous chorioretinopathy patients. Therapeutics and clinical risk management 9: 355-360.
- Prünte C, Flammer J (1996) Choroidal capillary and venous congestion in central serous chorioretinopathy. American journal of ophthalmology 121(1): 26-34.
- Yannuzzi LA (2010) Central serous chorioretinopathy: a personal perspective. American journal of ophthalmology. 149(3): 361-363.
- Spitznas M (1986) Pathogenesis of central serous retinopathy: a new working hypothesis. Graefe's Archive for Clinical and Experimental Ophthalmology 224(4): 321-324.
- Abouammoh MA (2015) Advances in the treatment of central serous chorioretinopathy. Saudi Journal of Ophthalmology. 29(4):278-286.
- De EK, De IB, Langlet P, Deltenre M (2000) Evidence based medicine and extradigestive manifestations of Helicobacter pylori. Acta gastro- enterologica Belgica 63(4): 388-392.
- Carloni E, Cremonini FI, Di Caro SI, Padalino C, Gerardino LA, et al. (2000) Helicobacter pylori-related extradigestive diseases and effects of eradication therapy. Digestive and Liver Disease 32: 214-216.
- Zbinden R (2005) Expanding the spectrum of Helicobacter pylori-associated diseases. Infection. 33(2): 49.
- Roussos A, Philippou N, Gourgoulianis KI (2003) Helicobacter pylori infection and respiratory diseases: a review. World journal of gastroenterology 9(1): 5.
- Ricci C, Holton J, Vaira D (2007) Diagnosis of Helicobacter pylori: invasive and non-invasive tests. Best Practice & Research Clinical Gastroenterology 21(2): 299-313.
- Franceschi F, Sepulveda AR, Gasbarrini A, Pola P, Silveri NG, et al. (2002) Cross-reactivity of anti-CagA antibodies with vascular wall antigens: possible pathogenic link between Helicobacter pylori infection and atherosclerosis. Circulation 106(4): 430-434.
- Asensio-Sanchez VM, Rodriguez-Delgado B, Garcia-Herrero E, Cabo- Vaquera V, García-Loygorri C (2008) Central serous chorioretinopathy as an extradigestive manifestation of Helicobacter pylori gastric infection. Archivos de la Sociedad Espanola de Oftalmologia 83(3): 177-182.
- Feghhi M, Hajiani E, Khataminia G (2008) Incidence of Helicobacter pylori in central serous chorioretinopathy: a case control study. Jundishapur Journal of Microbiology 1(1): 15-19.
- Roshani M, Davoodi NA, Seyyed Majidi MR, Zojaji H, Sherafat SJ, et al. (2014) Association of Helicobacter pylori with central serous chorioretinopathy in Iranian patients. Gastroenterology and Hepatology from bed to bench 7(1): 63.
- Misiuk-Hojło M, Michałowska M, Turno-Krecicka A (2009) Helicobacter pylori--a risk factor for the developement of the central serous chorioretinopathy. Klinika oczna 111(1-3): 30-32.
- Cotticelli L, Borrelli M, D'Alessio AC, Menzione M, Villani A, et al. (2006) Central serous chorioretinopathy and Helicobacter pylori. Eur J Ophthalmol 16(2): 274-278.
- Mauget-Faysse M, Kodjikian L, Quaranta M, Ben DE, Trepsat C, et al. (2002) Helicobacter pylori in central serous chorioretinopathy and diffuse retinal epitheliopathy. Results of the first prospective pilot study. J Fr Ophtalmol 25(10): 1021-1025.
- Warrow D, Mukkamala K, Rosen RB (2012) Relationship between Helicobacter Pylori and Central Serous Chorioretinopathy. Investigative Ophthalmology & Visual Science 53(14): 5227.
- Ahnoux-Zabsonre A, Quaranta M, Mauget-Faysse M (2004) Prevalence of Helicobacter pylori in central serous chorioretinopathy and diffuse retinal epitheliopathy: a complementary study. J Fr Ophtalmol 27(10): 1129-1133.
- Casella AM, Berbel RF, Bressanim GL, Malaguido MR, Cardillo JA (2012) Helicobacter pylori as a potential target for the treatment of central serous chorioretinopathy. Clinics 67(9): 1047-1052.
- Rahbani-Nobar MB, Javadzadeh A, Ghojazadeh L, Rafeey M, Ghorbanihaghjo A (2011) The effect of Helicobacter pylori treatment on remission of idiopathic central serous chorioretinopathy. Molecular vision 17: 99.
- Sherafat SJ, Tajeddin E, Majidi MR, Vaziri F, Alebouyeh M, et al. (2012) Lack of association between Helicobacter pylori infection and biliary tract diseases. Polish journal of microbiology 61(4): 319-322.
- Prasad A, Zhu J, Halcox JP, Waclawiw MA, Epstein SE, Quyyumi AA (2002) Predisposition to atherosclerosis by infections: role of endothelial dysfunction. Circulation. 106(2): 184-190.
- Georges JL, Rupprecht HJ, Blankenberg S, Poirier O, Bickel C, et al. (2003) Impact of pathogen burden in patients with coronary artery disease in relation to systemic inflammation and variation in genes encoding cytokines. Am J Cardiol 92(5): 515-521.






























