Manometry in Chronic Anal Fissures: Clinical and Therapeutic Correlation
Elvis Vargas Castillo1,2*, Ingrid Melo Amaral1,3, Arisel Domínguez1, Aram Rojas1, Sthephfania López1, Daniel Chiantera1, Mariangela Pérez Paz1 and Jenils Daniela Coacuto1
1Coloproctology Unit, Domingo Luciani Hospital, Venezuela
2Coloproctology Unit of Barcelona, Universitary Hospital Dexeus, Spain
3Coloproctology Unit, Universitary Hospital of Clinicas, Paraguay
Submission:March 09, 2021; Published:March 22, 2021
*Corresponding author:Elvis Vargas Castillo, Coloproctology Unit, Domingo Luciani Hospital, Caracas, Venezuela, Coloproctology Unit of Barcelona, Universitary Hospital Dexeus, Barcelona, Spain
How to cite this article:Elvis Vargas C, Ingrid M A, Arisel D, Aram R, Sthephfania L, et al. Manometry in Chronic Anal Fissures: Clinical and Therapeutic Correlation. Adv Res Gastroentero Hepatol, 2021; 16(4): 555943. DOI: 10.19080/ARGH.2021.16.555943.
Abstract
Objective: The aim of this study is to determine the clinical and therapeutic relevance of manometric findings in patients with chronic anal fissure.
Methods: Descriptive, prospective study of 139 patients with chronic anal fissure (CAF) treated with Isosorbide Dinitrate 2% cream (Master Formula) for 6 to 8 weeks with a maximum of 2 treatment cycles. Physical exam findings were recorded prior to treatment, which included location of the fissure(s) and rectal sphincter tone. One week after beginning treatment, High resolution Anal Manometry (HRAM) was performed discriminating the rest pressure (RP) in low (<40 mmHg), normal (40-70 mmHg), and increased (> 70 mmHg) sphincter pressure. The increased (>70 mmHg) category was further subclassified as: mildly increased (71 -100 mmHg), moderately increased (101-150 mmHg) and severely increased (> 150 mmHg) with the intention of further describing the associations between the patients’ therapeutic evolution and their HRAM pressures.
Results: Mean age 42 ± 13 and 51.8% of patients were female. Posterior fissures were present in 87.8% of patients. 61 patients were found to have moderately increased RP (43.9%). 46% of patients with normal RP were classified as hypertonic on digital rectal examination (p = 0.01). Mean healing rate was 80% with medical treatment, this percentage was positively correlated with higher RP (p = 0.004). 20% underwent surgery, with the surgical technique depending on the RP, without reports of complications or fecal incontinence.
Conclusion:HRAM is a guiding tool in the evolution of the CAF, finding that the higher the RP is, the better the response to medical treatment. Additionally, in non-responders patients, to reduce complications, surgical management can and should take the RP into consideration and not only to the physical examination.
Keywords: Anal fissures; Anorectal manometry; Resting pressure; Chemical sphincterotomy; Internal lateral sphincterotomy; Anoplasty and fissurectomy; Fecal incontinence
Abbreviations: ILS: Internal Lateral Sphincterotomy; CAF: Chronic Anal Fissure; DRE: Digital Rectal Examination; RP: Resting Pressure; HRAM: High-Resolution Anorectal Manometry; IAS: Internal Anal Sphincter
Introduction
In the proctology consultation, 5% to 15% of the visits correspond to anal fissures. This pathology is one of the main causes of anal pain and bleeding when evacuating [1]. It produces significant morbidity and affects young adults. A high percentage of acute anal fissures heal spontaneously or with hygienic-dietetic measures. Sometimes they become chronic and do not respond to medical treatment, probably due to hypertonia of the sphincter and the resulting local ischemia. Internal Lateral Sphincterotomy (ILS) is the “Gold Standard” surgery, but hypertonia is not always present, therefore this procedure cannot be offered to all patients. The use of medical treatment, such as nitric oxide-releasing creams, has a cure rate of 91% for acute fissures and 62% for chronic ones, with a recurrence rate of 25% [1,2]. These results are comparable with those of the ILS, in which 95% have recovery [3] and recurrence ranging from 0 to 37.6% [4]. The complications of the use of these creams are minimal compared to the surgical procedure, specifically on continence, publications report a total incontinence rate of 17% post ILS: flatus 9%, spotting 6%, accidental evacuation 0.9%, incontinence to liquid stools 0.67%, incontinence to solid stools 0.83% [5].
Multiple investigations have compared the medical and surgical treatment of this entity, considering the complications of these two treatment alternatives, and it has been shown that ILS is effective but that it should be reserved for patients who fail to respond to the initial therapy of chemical sphincterotomy [6]. Identification of patients with low and normal pressure anal fissure is very important. They may be more susceptible to incontinence after procedures such as ILS due to altered sphincter anatomy. This may not manifest itself for several years when more damage occurs or with the gradual decrease in sphincter tone over the years [6,7]. Despite the important number of publications that deal with the results and complications of surgery and quality of life studies in patients undergoing aggressive surgical procedures, there are not many studies that evaluate anorectal manometric patterns in the behavior, and evolution of the anal fissure. Of particular interest is the fact that in most cases anal manometry is not performed in those patients who are diagnosed with acute anal fissure, for whom dietary changes are indicated with increased intake of fibers, water, sitz baths, and what does not respond to these changes is placed some medical therapy.
If after 6 to 8 weeks, the patient does not have a satisfactory change in the clinic, then it is considered a chronic anal fissure; and this is when the indication of anal manometry could become important [7,8]. Studies suggest that digital rectal examination is not reliable when making a surgical decision, since normal or low resting pressure is more common than previously reported [8- 10]. Although traditionally it has been assumed that most fissures are hypertonic, the resting pressure profile of patients with anal fissures can be very broad, so that normal pressures can be found in up to 52% of patients. This can depend on many factors, such as location, diameter of the Internal Anal Sphincter (IAS), sex, multiparity, age, which added to the doubtful value that a simple digital examination can provide reinforces the interest that the use of manometry may have in these patients [9,11].
Despite the higher cure rate with surgical treatment compared to medical treatment in the comparative studies carried out, the most recent therapeutic guidelines for treatment begin to establish the use of medical treatments as the first therapeutic line, leaving surgical sphincterotomy as the second step in cases of recurrence or selected patients without risk factors for incontinence [12,13]. Techniques that do not divide the IAS, such as anoplasty and fissurectomy, allow a good frequency of healing, it is theoretically attractive, especially in patients with pre-existing continence problems or in those without hypertonia of the anal sphincter, patients with canal stenosis anal, because of a hemorrhoidectomy, elderly, multiparous women. Studies have been carried out with this technique that report healing of the fissure without changes in continence, but further research is needed now [13]. The anoplasty can be performed in V-Y or in advance of the island or House Flap, in the form of full thickness, to cover the defect caused by the crack [14].
Patients with fissures consist of a heterogeneous population with anal canal pressure profiles ranging from classical hypertonic, normotonic, and hypotonic. Before selecting the surgical treatment, it is essential to determine which subtype it is, due to the risks that sphincterotomy entails. Chronic low-pressure fissures should raise suspicions of a specific etiology, usually it is not a patient who is a candidate for surgery and requires a preoperative physiological study [12]. Determining the pressure profile of each patient can be useful on the one hand in the diagnosis and on the other in choosing the treatment to follow, identifying risk factors for incontinence, recurrence factors, or simply pressure necessary to benefit from Chemical Sphincterotomy or Surgical Sphincterotomy and that is why we decided to determine what is the clinical and therapeutic relevance of manometric findings in patients with chronic anal fissure.
Methods
A single-centre prospective, experimental study was conducted at the coloproctology Unit of Domingo Luciani Hospital, Caracas, Venezuela from January 2016 to 2019. The study protocol was approved by the local ethics research committee (protocol number 00532) and was exempted from an informed consent requirement to the patients.
Inclusion and Exclusion Criteria
Patients with the following criteria were included: Patients between 18 and 70 years with anterior or posterior chronic anal fissure (CAF) without previous anorectal surgery and were able to consent to participate and attend all scheduled followup visits. Exclusion criteria were: Patients with fissure anal not chronic or with lateral localization; men with have anal sex, patients with allergic to treatment or who stop this for adverse effects, anal fissures for secondary diseases such as inflammatory bowel disease, trauma or pelvic radiation and immunosuppressed patients.
MStudy Design
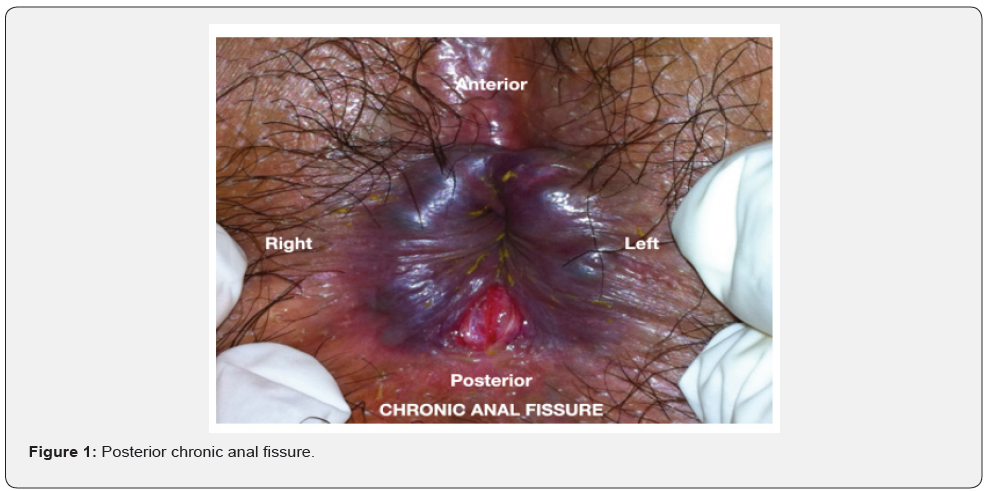
Patients were examined by colorectal surgeon and clinical descriptions were made (location of the fissure, tone of the sphincter on digital rectal examination) (DRE) (Figure 1). Hygienic-dietary measures, stool softeners (if necessary) and Isosorbide Dinitrate Cream 2%, every 8 hours for 8 weeks to be placed with applicators (swabs), without contact with the hands and in a small amount, to minimize adverse effects. A week after starting treatment, all patients were performed a manometry by another colorectal surgeon who was unaware of the previous findings of the physical examination, using a high-resolution anorectal manometry that allowed to measure the Resting Pressure (RP). Patients were followed up at 1 and 2 months and if the anal fissure and symptoms persisted during this time; another cycle of treatment was repeated for 8 more weeks and at 16 weeks the definitive evolution was verified, relating this evolution to the RP findings in the previously manometry. Healed patients with medical treatment were followed up by telephone for 1 to 3 years and those who were not, underwent surgery, deciding the correct surgical approach: Internal lateral sphincterotomy (ILS), Y-V anoplasty or fissurectomy according to the RP values in the manometry with follow-up at 1 month and 2 months and later by telephone like the group who responded to medical treatment. Recurrence and fecal incontinence rate of both groups were recorded. Botulinum toxin treatment option in these patients was not proposed in our study because it was not approved as a treatment for CAF in our health system. The IBM SPSS Statistics version 22.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis. A value of p ≤ 0.05 was considered significant.
Manometry Technique
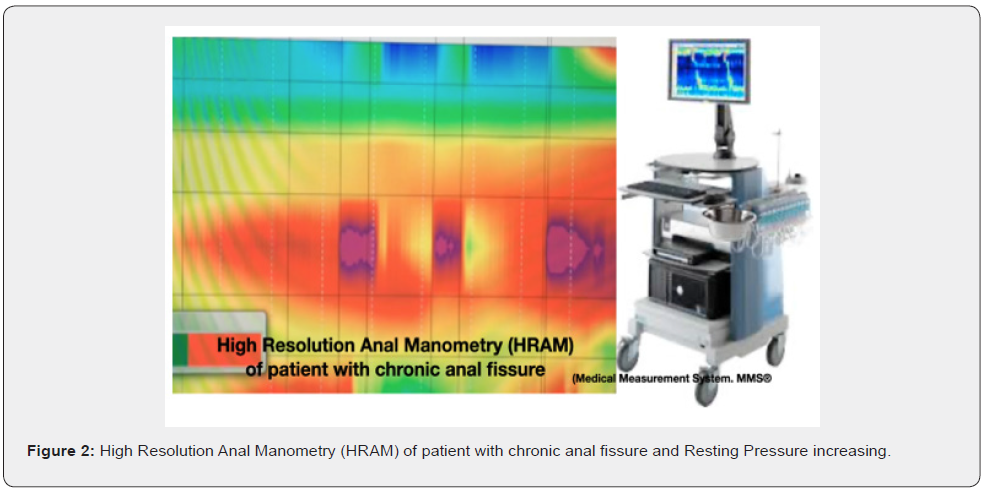
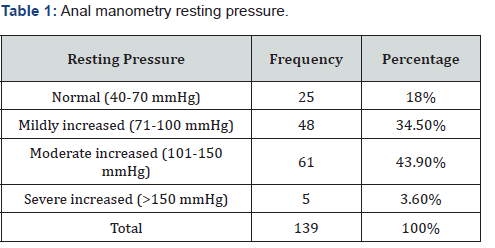
High-resolution anorectal manometry (HRAM) (Medical Measurement Systems®), with an adult catheter of 8 longitudinal channels, external diameter of 4.2mm and a balloon of 3.3cm long and maximum capacity of 400cc was performed to all patients one week after starting medical treatment with Dinitrate isosorbide ointment. These catheters use novel solid-state pressure transduction technology (touch array sensors) that acquire data at 35 Hz and provide a single mean pressure across the entire circumference at 6 mm intervals throughout the entire length of the anal canal, without the need for stationary withdrawal (Figure 2). We used a Sim´s position and complete manometry findings were recorded including: Resting pressure, wave slow and ultra-slow, squeeze pressure, sustained squeeze, inhibitory rectoanal reflex, cought reflex, sensitivity, and compliance. However, we considered the resting pressure (RP) values due to their relationship in the pathophysiology of the anal fissure and it was referred to as low value < 40 mmHg, normal value between 40-70mmHg and high > 70 mmHg. When the RP was increased it was sub-classified into: Mildly increased (71-100mmHg), moderate (101-150mmHg) and severe (> 150mmHg).
Results
Between January 2016 to 2019, 230 consecutive patients with anal fissure, but after inclusion and exclusion criteria, sample of 139 patients (72 women and 67 men; mean age 42.55 (s.d) (13.4) (range 22.3 – 63.9 years). The CAFs were in the posterior commissure in 87.8% (n = 122), anterior 10.8% (n = 15), and 0.7% (n = 2) anteroposterior.
High resolution anal manometry resting pressure and digital rectal examination
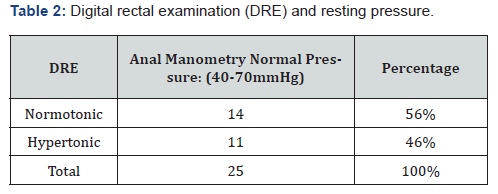
HRAM RP was moderately elevated in 43.9% (n = 61), mildly increased 34.5% (n = 48), normal RP 18% (n = 25), severely increased 3.6% (n = 5) and no patients with low pressure (n = 0) (Table 1). Of the 25 patients who had normal RP in manometry 46% (n = 11) were diagnosed with sphincter hypertonia on DRE and 54% (n = 14) normotonic (p = 0.01) (Table 2).
Chronic anal fissure healing
By RP ranges, 80% healed to medical treatment (range 64 to 100%), this response was mean 4.55 weeks (s.d.) (1.8 weeks) and showing that while higher the RP, greater the response to treatment; thus, we had that 100%, 92%, 71% and 64% of the patients with severely, moderate, slightly increased, and normal RP were healed with medical treatment, respectively (p = 0.004) (Table 3).
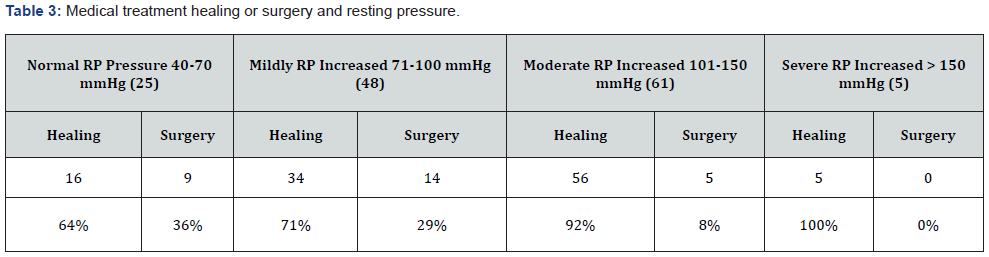
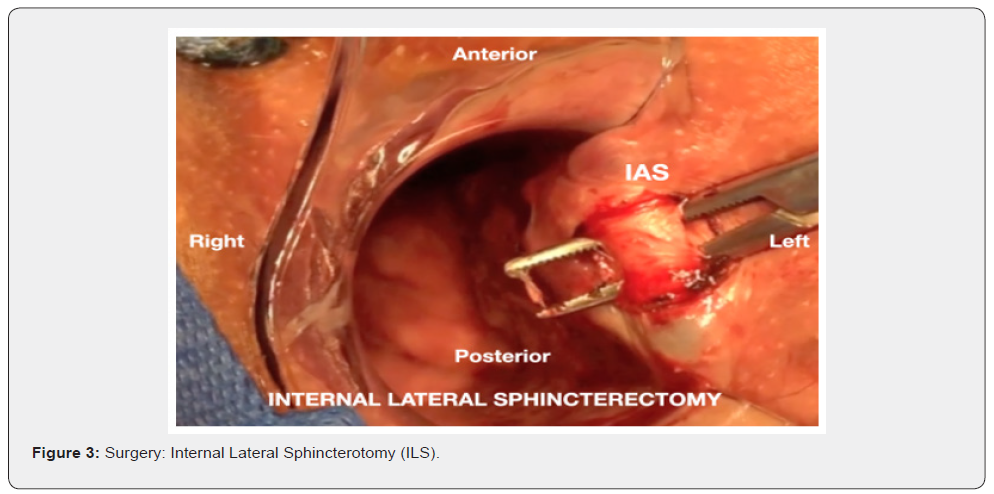
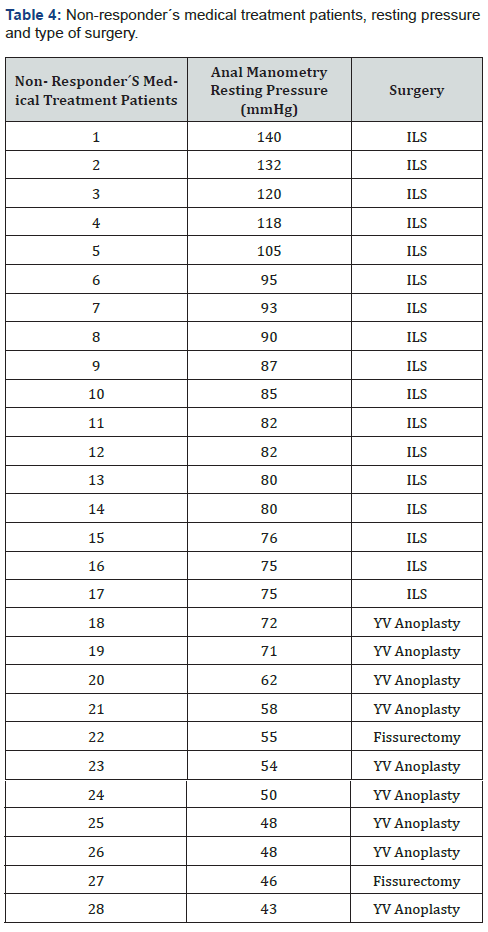
Surgery
20% (n = 28) needed surgical resolution. Type of surgery was made based on the manometry RP, performing ILS in 17 patients, (Figure 3) 5 with moderately increased RP and 12 with mildly increased RP. YV anoplasty technique was performed in 9 patients, 7 with normal RP and 2 with mildly increased RP because they had values very close to normal. Fissurectomy was performed in 2 of normal RP, due to surgeon preference (Table 4).
Recurrence and fecal incontinence
Mean follow-up was 22 months (range 8-36). Anal fissure recurrence in 15 patients (10,7%), 13 were after medical treatment, which were treated with a new cycle and improving all and 2 after surgery, specifically ILS in which, due to previously having manometry PR mildly increased we decided to perform later YV anoplasty. No cases of fecal incontinence in two groups were reported.
Discussion
The resting pressure that is known as normal and according to international standards is 40-70mmHg, figures that can vary greatly in patients with anal fissure [8,15,16]. Several authors have studied anorectal pressures in patients with anal fissure using manometric techniques and although some have found no differences in resting pressures between patients with fissure and controls, most studies have shown an increase in the pressure at rest in individuals with anal fissure [14,15]. It has been suggested that the disparity in results could be due to the use of different measurement techniques and catheters of different diameter.
In 2013 an investigation was published with many patients with CAF who had normal resting pressure ranges (52.1%), this observation has two consequences. First, sphincterotomy could induce borderline hypotonia to fecal incontinence and second, anorectal manometry may be necessary in this group of patients before performing sphincterotomy [17]. In 1995, Prohm et al. published an interesting article about the essentials of performing anorectal manometry in patients with anal fissure and its influence on the evolution of this pathology. They included 177 patients who underwent preoperative manometry to demonstrate the increase in resting pressure. The control group was made up of 14 patients without proctological problems, with a resting pressure of 74.4 ± 8.9 mmHg, with a normal pressure limit of 90 mmHg. Patients with fissure were divided into two groups: A) resting pressure less than or equal to 90mmHg and B): greater than 90mmHg. Six weeks after the operation, a new manometry was performed. The resting pressure decreased in all patients from 106 ± 27.2 to 80 ± 10.4 mmHg. In relation to continence, despite not being statistically significant, fecal spotting, flatus and fluid incontinence had a frequency of 3.2% in patients with resting pressure less than 90 mmHg with a recurrence rate of 9.7%, compared to 0.7% with resting pressure greater than 90 mmHg with a recurrence of 2.1%. Demonstrating the importance of pre-surgical manometry [18]
It is true that the ILS is a relatively simple and effective technique , is considered the treatment of choice in these cases, but the incidence of fecal incontinence that it causes, has prompted the search for other medical therapies that allow a chemical sphincterotomy, obtaining a high healing rate and those patients who do not improve with this type of treatment, it is then recommended to perform anal manometry, to determine which surgical treatment would be ideal according to the resting pressure [8,19]. It must be borne in mind that although the ILS is the Gold Standard, not all patients qualify for its performance, in clinical-manometric studies it has been shown that there is a group of patients with certain associated conditions (> 50 years, incontinence, risk factors for incontinence known in the literature as: previous anal surgery, multiple vaginal deliveries, diabetes, inflammatory bowel disease, etc.) or with anal fissure without associated hypertonia, in which there is a greater risk of residual incontinence after surgery, so we must avoid it as the first therapeutic option and look for other alternatives, such as chemical sphincterotomy, Botulinum toxin, anoplasty, fissurectomy which does not produce residual incontinence [20].
As we have shown in our work, the use of anal manometry, helps to know the patient’s profile and to intuit the possibilities of cure and therefore the possibility of surgery. Furthermore, we observe that this group that does not improve has a wide range of variability in RP figures ranging from a moderate increase to normality; patterns that are difficult to determine with rectal examination. The group with most risk of fecal incontinence is those with normal or mildly increase manometry pressure and these were in our experience of 18% and 34,5% correspondingly and precisely these are the groups that least responded to medical treatment and also, they are not diagnosed with DRE in 46%. All this look decisive when deciding the best surgical technique with the intention of avoiding continence alterations in these patients especially doing a ¨gold standard¨ procedure (ILS). These results do not have much support in the bibliography, which is why a greater number of investigations must be carried out to standardize the best and ideal performance in the face of this frequent pathology.
Conclusion
HRAM is a guiding tool in the evolution of the CAF, finding that the higher the RP is, the better the response to medical treatment. Additionally, in non-responders’ patients, to reduce complications, surgical management can and should take the RP into consideration and not only to the physical examination.
Limitations of the Study
Single-center study. DRE was performed without medical treatment and anal manometry one week later of starting treatment. Numerical difference between RP manometry groups. No anal manometry after healing CAF.
References
- Cacarian H (1982) Role of internal sphincter in Chronic anal fissures. Dis Colon y rectum 25(6): 525-528.
- Werre AJ, Palamba HW, Bilgen EJ, W F Eggink (2001) Isosorbide dinitrate in the treatment of anal fissure: a randomised, prospective, double blind, placebo-controlled trial. Eur J Surg 167: 382-385.
- Pascual M, Courtier R, Gil M y colaboradores (2005) Endosonographic and manometric assessment of the internal anal sphincter in patients with chronic anal fissure. Cir Esp 77(1): 27-30.
- Orsay Ch, Rakinic J, Perry B, Hyman N, Buie D, et al. (2004) Practice Parameters for the Management of Anal Fissures (Revised). Dis Colon Rectum 47: 2003-2007.
- Xynos E, Tzortzinis A, Chrysos E, Tzovaras G, Vassilakis J (1993) Anal manometry in patients with fissure-in-ano before and after internal sphincterotomy. Int J Colorect Dis 8: 125-128.
- Farouk R, Duthie G, MacGregor A, Bartolo D (1994) Sustained internal sphincter hypertonia in patients with chronic anal fissure. Dis Colon Rectum 37: 424-429.
- Evans JP, McLeod RS (2001) Anal Fissure. Probl Gen Surg 18: 7-16.
- Horvath K, Whelan R, Golub R, Ahsan H, Cirocco W (1995) Effect of catheter diameter on resting pressures in anal fissure patients. Dis Colon Rectum 38: 728-731.
- Perea R, Mendoza C, García I y colaboradores (2005) Fisura anal: experiencia en 10 añ Revista Cirujano General.
- Oliver Jones, Ramalingam T, Lindsey I, Chris Cunningham, Bruce D George, et al. (2005) Digital rectal examination of sphincter pressures in chronic anal fissure is unreliable. Diseases of the colon and rectum Dis Colon Rectum 48(2): 349-352.
- Altomare D, Binda, Canuti S, Landolfi V, Trompetto M, Villani R, et al. (2011) The management of patients with primary chronic anal fissure: a position paper. Tech Coloproctol 15: 135-141.
- Thornton MJ, Kennedy ML, King DW (2005) Manometric effect of topical glyceryl trinitrate and its impact on chronic anal fissure healing. Dis Colon Rectum 48(6): 1207-1212.
- Lund JN, Scholefield JH (1996) Aetiology and treatment of anal fissure. Br J Surg 83: 1335-1344.
- Ciriza de los Ríos, Miguel Mínguez, José María Remes Troche, Glòria Lacima (2018) Manometría anorrectal de alta resolución y de alta definición: Redescubriendo la función anorrectal. Rev Esp Enferm Dig 110(12): 794-805.
- Bove A, Balzano A, Perrotti P, Antropoli C, Lombardi G, Pucciani F (2004) Different anal pressure profiles in patients with anal fissure. Tech Coloproctol 8(3):151-156.
- Romano G, Rotondano G, Santangelo M, Esercizio L (1994) A critical appraisal of pathogenesis and morbidity of surgical treatment of chronic anal fissure. J Am Coll Surg 178: 600-604.
- P Garg, M Garg, R Menon (2013) Long term continence disturbance after lateral internal sphincterotomy for chronic anal fissure: a systemic review and meta-analysis. Colorectal Dis 15(3): e104-117.
- Peter Prohm, Christoph Bonner (1995) Is Manometry Essential for Surgery of Chronic Fissure-in-Ano? Dis Colon Rectum 38: 735-738.
- Simkovic D, Smejkal K (2001) Importance of the anorectal manometry in chronic anal fissure 44(3): 105-107.
- Günal O, Gürlevik E, Arikan Y, Pehlivan M (2007) Assessment of anal sphincter function by Sengstaken-Blakemore tube anal manometry. World J Surg 31(2): 399-402.






























