Acute Acalculous Cholecystitis in a Patient with Covid - 19
Alfonso Palmieri1*, Adriana María Palmieri 2, Luz Adriana Hernández3 and Eder Canchila4
1Professor of Chair, subject Adult Health II, University of Sucre, Colombia
2Student of the 5th semester of Medicine program, Universidad del Norte, Colombia
3Faculty of Health Sciences, University of Sucre, Colombia
4Internal Physician, Universidad del Sinú, Colombia
Submission:November 16, 2020; Published:December 23, 2020
*Corresponding author:Alfonso Palmieri Luna, Physician, specialist in General Surgery and Laparoscopy, member of the Colombian Association of Surgery (ACC), Latin American Federation of Surgery (FELAC). Surgeon of the Santa María Clinic; Professor of Chair, subject Adult Health II, Medicine Program, University of Sucre, Carrera 43 # 25A-04 (Barrio Venecia vieja), Sincelejo, Sucre, Colombia
How to cite this article:Palmieri A, Palmieri AM, Hernandez LA, Canchila E. Acute Acalculous Cholecystitis in a Patient with Covid - 19. Adv Res Gastroentero Hepatol, 2020;16(3): 555936. DOI: 10.19080/ARGH.2020.16.555936.
Abstract
Acute alithiasic cholecystitis (AAC), also called acalculous, corresponds to the presence of an inflammation of the gallbladder in the absence of stones inside, it is a rare entity (10%), reported in diabetic patients, immunosuppressed, with pathologies infectious (viral, bacterial), major surgery, drugs, multiple trauma, mechanical ventilation, use of vasopressors, opioid analgesics, prolonged fasting, total parenteral nutrition, burns, among others. In this time of the SARS CoV-2 virus / COVID-19 coronavirus disease pandemic, surgeons have found an increase in the request for interconsultations from respiratory hospitalization services, intermediate care and intensive care units, due to ultrasound findings of incidental abdomen of acute alithiasic cholecystitis in those patients without improvement to treatment or worsening of sepsis, or the cytokine cascade, difficult to evaluate abdominal epigastric pain, right upper quadrant, induces us to explore and find little painful palpable gallbladder, reporting edema gallbladder wall greater than 3 mm, gallbladder distention, sometimes ultrasound Murphy’s sign, extending imaging studies according to the patient’s conditions with contrasted computed axial tomography and nuclear magnetic cholangioresonance, and even with reports of micro perforations with peri-vesicular extravasation of contents , free air on its walls, ruling out other causes of acalculous cholecystitis. It is a real diagnostic and therapeutic challenge in these patients with the SARS virus –COV-2 / COVID-19, already afflicted by viremia, or in some cases subjected to cytokine storms, poor general conditions, hermodynamically unstable in Intensive care units, intubated, with vasopressor support, and even some overcoming the emergency, what would be the best time to resolve Acute acalculous cholecystitis medically or surgically? This is the big question.Keywords: Cholecystitis; Alithiasic; Acalculous; Gallbladder; Sars - cov-2 / Covid-19; Cholecystectomy; Bacterium ; Lactobacillus
Abbreviations: AAC: Acute Alithiasic Cholecystitis; SIRS: Systemic Inflammatory Response Syndrome; RT-PCR: Reverse Transcriptase Polymerase Chain Reaction; ACE 2: Angiotensin Converting Enzyme 2
Introduction
Acalculous cholecystitis is a rare primary disease in 10% of patients, and involves edema of the mucosa, gallbladder wall greater than 3 mm and inflammation, without the presence of stones inside (the most common cause of acute cholecystitis 90%), generally reported as complications in diabetic, immunosuppressed patients, in intensive care units subjected to great stress, septic shock, hypovolemic, mechanical ventilation, prolonged fasts, total parenteral nutritional support, large burns, multiple trauma, multiple transfusions, the use of vasopressors, opioid analgesics; Another infrequent form reported is bacteremia caused by salmonella tiphy and staphylococcus; Coxakie viremia, hepatitis A, B, Q fever, dengue, among others, that colonize the gallbladder [1-3].
The pathophysiology relates:
a. Low motility of the gallbladder, leading the patient to increased bile viscosity, pigment dehydration phenomenon formation of sludge or bile mud generally the protective glycoprotein of the mucosa is altered by the effect of the hydrolysis of phospholipase passing the luminal lecithin into lysolecithins (toxic), exposing the mucosal epithelium to the direct detergent action of bile salts, erosion of the mucosa by stasis of bile pigments, secondary bacterial colonization, spasm of the duct and cystic artery, progressively to gangrene, perforation and in the case associated with opioid analgesics, the spasm of the sphincter of oddi is added [1,2,4].
b. Hypoperfusion, ischemia, the cystic artery is terminal, without collateral circulation, edema and inflammation factors, gallbladder distention, worsen blood flow, progresses to acute gangrenous or emphysematous cholecystitis and perforation [1,2,4].
Diagnosis
The clinical picture in these critically ill patients, some intubated is difficult to interpret, in some it is impossible to manifest symptoms, despite being very similar to patients with acute lithiasic cholecystitis, but in these, the presentation is insidious, difficult to obtain the symptoms and signs (abdominal pain, epigastrium, right upper quadrant, radiating to the back, nausea, vomiting, fever, findings of a positive Murphy’s sign, palpable gallbladder, painful), in other patients with sepsis or septic shock that do not improve, despite aggressive management in intensive care units, hepatobiliary ultrasound often guides us to the diagnosis, given by obstruction cystic duct due to thick bile or biliary sludge, for which reason to have high suspicion to avoid reaching the diagnosis late, increasing mortality.
Laboratory
Leukocytosis, neutrophilia, acute phase reactants present, elevated bilirubins, alteration of transaminases [2-4].
Images
Diagnostic studies of AAC continue to be supported by hepatobiliary ultrasound with a specificity of 90% with a wall thickness of 3 m, and 98.5% for a thickness of 3.5mm, sensitivity of 100% and 80% respectively [2,4,5].
Major criteria: wall edema greater than 3mm, peri-vesicular fluid, distention greater than 5 cm in length, intramural gas or emphysematous wall. Vesicular hydrops (clear fluid), positive Murphy’s sign.
Minor criteria: Distension of the gallbladder> 5cm in the transverse axis, biliary sludge.
Currently, the world is in a health emergency caused by the Sars-Cov2 virus / Covid-19 coronavirus disease, several publications and research on this virus conclude that the inflammatory process attacks multiple systems [6], organs including: lung, renal hematological, hepatic, gastrointestinal, lately they report involvement of the gallbladder, among others, activation of the cytokine cascade, which can trigger conditions such as in this case acute acalculous cholecystitis, possibly due to this type of virus, sometimes difficult to diagnose, or lead to management of percutaneous drainage or late surgery due to poor patient conditions [2,6].
The objective of presenting this clinical case is to review multifactorial acute acalculous cholecystitis, its diagnostic approach, treatment and, in this time of pandemic, the association between patients with the Covid-19 coronavirus disease and its development, as a possible causal agent.
Clinical Case
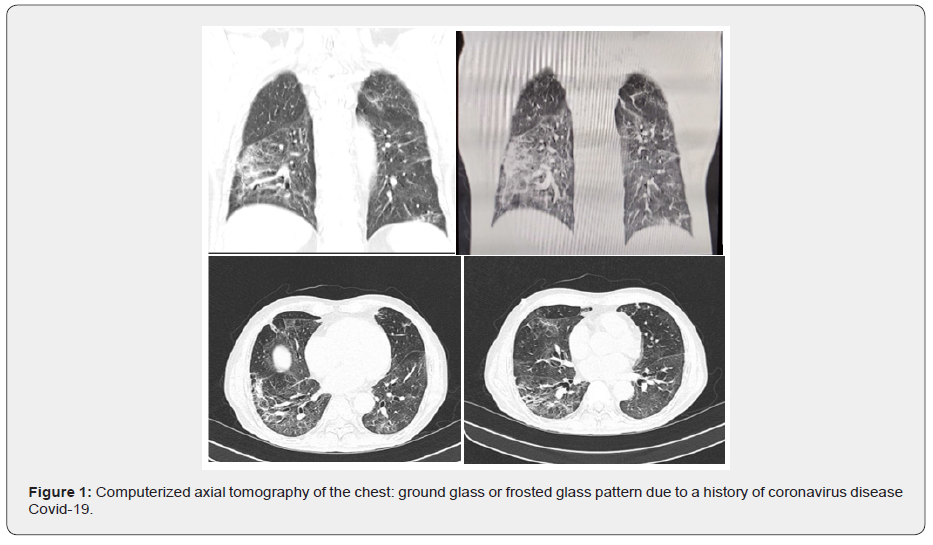
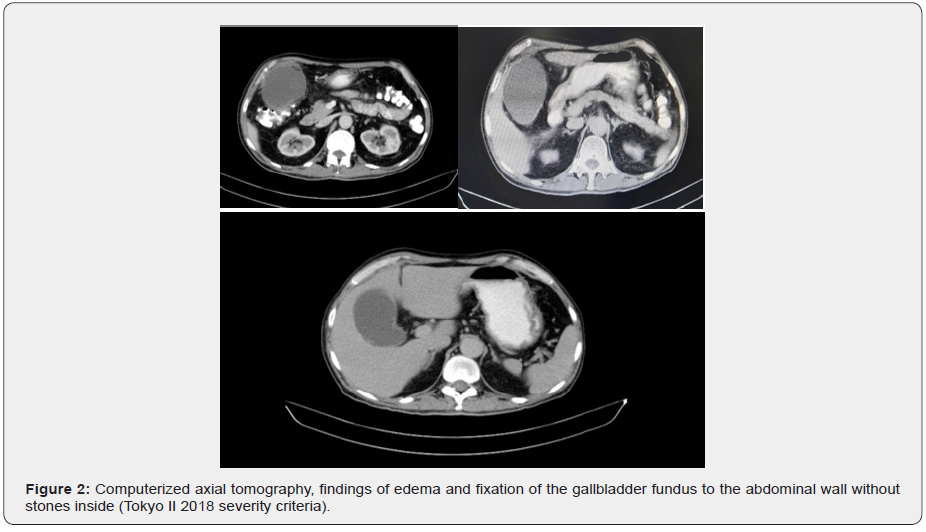
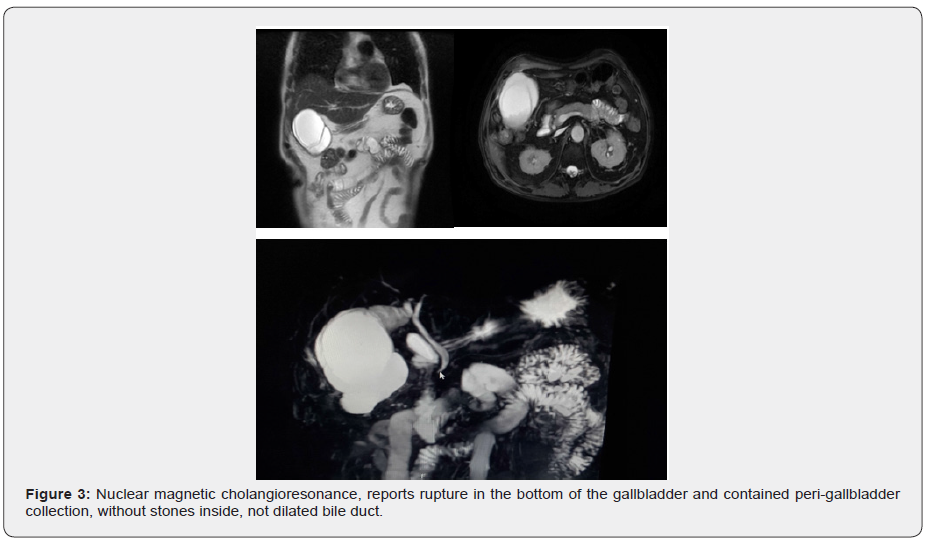
67-year-old male patient, male, re-admitted to the emergency department on 09/19/2020, with a clinical picture characterized by pain in the epigastrium, hypochondrium and right flank that radiates to the dorsal region, nausea, general malaise, myalgia , adynamia, fever not quantified, with a history of Pneumonia due to covid-19 confirmed by nasopharyngeal swab (RT-PCR) on 07/14/2020, sub-acute acalculous cholecystitis, studied and medically managed in the intensive care unit, For its bad conditions, it was decided to follow broad-spectrum antibiotics, until the abdominal pain improvement was achieved, the coronavirus disease was overcome, and on 08/01/2020 for management and follow-up of alithiasic cholecystitis by the outpatient clinic. Findings on physical examination upon readmission: regular general and nutritional conditions, no signs of systemic inflammatory response (SIRS), symmetric chest, eupneic, rhonchi rales in both lung fields, soft, depressible abdomen, slightly painful palpable gallbladder, non-icteric, no signs of peritoneal irritation. Laboratory and imaging studies are carried out: hemogram: hemoglobin: 14.7gr / dl, hematocrit: 45.9%; leukocytes: 10950 x mm3, neutrophils: 72%; platelets: 264,000 x mm3; amylase: 135 U7L; lipase: 85U / L; Got - Ast: 40 U / L; Gpt: 108 U / L. total bilirubins: 1.2mg / dl; creatinine: 0.7mg / dl; sodium 141 mEq / L; blood glucose 133 mg / dl; negative febrile antigens, total abdominal ultrasound reports sub-acute alithiasic cholecystitis, computed tomography of the chest (Figure 1), concludes findings suggestive of coronavirus covid-19; Double contrast computerized axial tomography of the abdomen (Figure 2), findings suggestive of sub-acute alithiasic cholecystitis with fixation of the gallbladder fundus to the anterior abdominal wall, Tokyo II classification, Cholangioresonance (Figure 3), reports suggestive changes of hydrocolecyst plus rupture gallbladder at fundus level, accompanied by peri-vesicular collection and moderate intravesicular bile sediment.
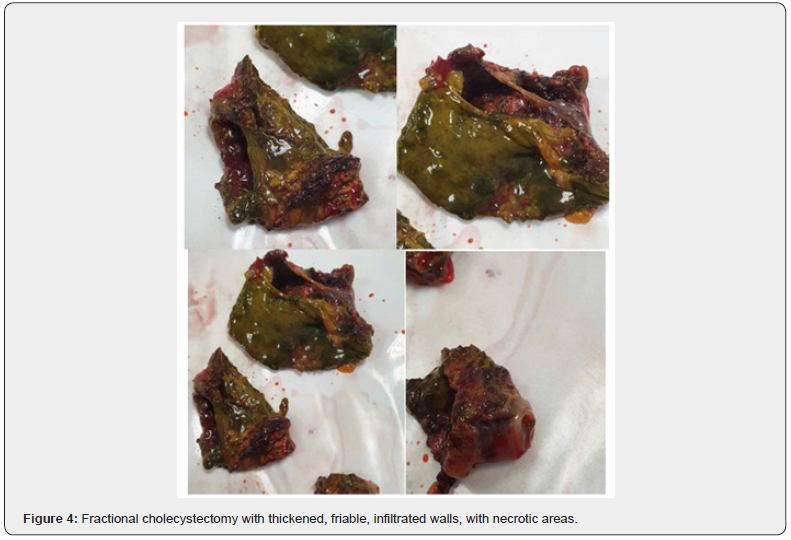
Patient is motivated to perform open cholecystectomy due to persistence of symptoms and report of micro perforation, perivesicular collection (images), finding a large gallbladder plastron, showing a gallbladder with thickened, necrotic, infiltrated walls, a sample is taken and sent for study of Laboratory for Gram, culture, antibiogram of non-purulent biliary juice, multiple peritoneal adhesions, firm, perforation contained in the bottom of the gallbladder, due to the state of the walls, resection of the gallbladder is performed in scale or fragments (Figure 4) , identifying the vascular anatomical structures and undamaged biliary drainage duct, post-operative management in the intensive care unit, satisfactory evolution, tolerating the oral route at 48 hours, leaving home at 6 days, removing drains, gram and reported culture at 72 hours negative for common germs, which makes suspect the viral possibility, even in our country requests to carry out RT-PCR tests to symptomatic patients, it is worth filling out authorization documents (mipres), glossing the accounts for which the bile juice study was not carried out, a control appointment at 10 and 30 days without complications.
Discussion
Acute alithiasic cholecystitis (AAC) is a rare disease (2-15%), predominantly male from 1.5: 1 to 3: 1; Fifth decade of life, there are multiple risk factors: diabetics, immunosuppressed, patients in intensive care units subjected to prolonged fasting, total parenteral feeding, multiple trauma, severe burn, poly-transfused, hypovolemic shock, septic, use of analgesics opiates, vasopressor support [1-4].
The first description of acute alithiasic cholecystitis was published by Duncan in 1884 in an autopsy of a patient operated on for femoral hernia, who developed acute allithiasic cholecystitis, sepsis and death, describing it as gangrenous [7].
The arrival of the SARS CoV-2 virus, developing severe acute respiratory distress syndrome or coronavirus disease 2019 (COVID -19), in the city of Wuhan (China), reported in a retrospective study in December 2019 [8], from of which the multiple symptoms and associated pathologies have been revealed, due to the different affinities of the virus to ACE2 receptors, within the last reported: gastroenteritis, myocarditis, myositis, and acute alithiasic cholecystitis [9-11].
In children under 11 years of age, the presentation of acute acalculous cholecystitis (AAC) is around 30-70%, associated with bacterial infections (Salmonella, Escherichia coli, group A beta-hemolytic streptococcus, or viral (hepatitis A and B. cytomegalovirus, Epstein Barr, human immunodeficiency virus (HIV), dengue, Q fever, parasitic: ascariasis, toxoplasmosis, plasmodium [2,4,9,12,13].
The difficulty of early diagnosis of AAC in a critically ill patient leads to an additional mortality of over 30%, due to gallbladder gangrene in 50% and perforation in 10% [2]; bizarre symptoms, clinical findings in an intubated patient, on mechanical ventilation, sedation, in sepsis, decompensated diabetic, heart failure, postresuscitation from cardiac arrest, shock hemorrhagic, postoperative major cardiovascular surgery, polytrauma, or infectious bacterial or viral diseases, makes it part of a late diagnosis, a challenge that we must face with suspicion.
In patients with the SARS CoV-2 virus, who develop severe acute respiratory distress syndrome or coronavirus disease 2019 (COVID -19), according to their risk factors, clinical course of the disease, its complications, multi-organ dysfunction, and mortality, always Identifying the virus with the reverse transcriptase polymerase chain reaction (RT-PCR), we have been taught every day more about this new disease, its transmission mechanisms and recent reports of acute acalculous cholecystitis are striking (9 -11), affection of the gastrointestinal tract, mediated by its high affinity with angiotensin converting enzyme 2 (ACE 2) receptors, identified in the duodenum, small intestine and colon, isolating the virus in the feces, opening other possible sources of contagion, suggesting to extend the studies with RT-PCR in feces routinely [9].
Treatment
The treatment of calculous acute cholecystitis is cholecystectomy, preferably laparoscopic; Regarding acalculose, the approach from long before the onset of the Covid-19 coronavirus disease is controversial, initially, broad-spectrum antibiotic therapy covering gram-negative germs (Escherichia coli: 41%; Enterococcus: 12%; Klebsiella: 11 %; enterobacter: 9%; anaerobic percentage variable [14-17]; depends on the time of evolution of the disease, patient conditions, mechanical ventilation, hemodynamic instability, vasopressor support, use of anticoagulants [2,4,6,14-17], expectant conservative management will be preferred, clarifying that it does not attempt to replace cholecystectomy when peri-vesicular collections are suspected; in case of no improvement in symptoms, opting for percutaneous drainage (ultrasound-guided cholecystostomy) report success in a 85-90%, including transpapillary and transmural peroral endoscopic drainage guided by endosonography, and in others laparoscopic or open cholecystectomy, according to the surgeon’s experience [14-17], without forgetting within the differential diagnosis of gallbladder volvulus, hepato-biliary ultrasound has been reported, often as acute alithiasic cholecystitis [18].
Now in the case of patients infected by SARS CoV - 2 / Covid -19, to take into account the need for the patient’s prone position, stabilize the cytokine storm, following the Tokyo 2018 severity guidelines [6], we welcome furthermore, the guidelines of the American College of Surgeons [19], and those of the Colombian Association of Surgery [20], initially follow expectant medical management, as in the case of our patient, who improves, overcomes the Covid, provide an outlet for convalescence and readmission due to non-response or failure in outpatient treatment; advancing in the protocol of performing percutaneous drainage guided by ultrasound (cholecystostomy, report its risks, such as bleeding, perforation of the hollow viscus, intestinal fistulas, peritonitis), no clinical improvement, persistent palpable gallbladder, fever, imaging of contained perforation, open cholecystectomy is preferred [15], until further studies clarify the side effects of the aerosols issued by the electrosurgical knife in the laparoscopic route, not being a source of contagion to health personnel. It remains for the future to carry out routine cultures of bile juice with RT-PCR, given the possibility of turning the gallbladder into a reservoir of the SARS-Cov-2 virus, eliminating it through the feces, favoring another mechanism of viral transmission and spread.
Conclusion
Acute alithiasic cholecystitis is a disease associated with patients with comorbidities (diabetes, chronic kidney disease, immunosuppressed), or those hospitalized in intensive care units, severe burns, prolonged fasting, total parenteral feeding, postsurgical major surgeries, multiple trauma and in lower proportion of bacterial, viral, parasitic and fungal infectious diseases. The conduct to be followed is expectant with medical management and the majority respond favorably, few are taken to interventional percutaneous drainage procedures, laparoscopic or open cholecystectomy in the emergency room. With the arrival of the pandemic caused by the SARS CoV-2 virus / Covid-19 coronavirus disease, an increase in consultations to the emergency services of general surgery for acute alithiasic cholecystitis has been noted, the great affinity of the virus for ACE 2 receptors , located in the digestive tract and in view of reports of virus isolation by RT-PCR in feces, raises the possibility of being another source of contagion, and in the gallbladder becoming a reservoir of the disease as occurs in salmonellosis. The conduct continues to be expectant, accepting the recommendations of the American College of Surgeons and the Colombian Association of Surgery
Acknowledgement
Dr Gustavo Navarro Ulloa, Dr Alfredo Navarro Ucrós, from the Santa María Clinical Radiology service; Álvaro Sánchez, services of the Respiratory Intensive Care Unit and Dr Luis Armando Mejía Vargas, General Surgeon at the Santa María Clinic for joint management.
References
- Theise Neil, Robins-Cotran (2015) Structural and functional pathology, (Chapter 18.), Liver and gallbladder, Elsevier Saunders, (9th edn.), Spain, pp. 878.
- Barie PS, Eachempati SR (2010) Acute Acalculous Cholecystitis. Gastroenterol Clin North Am 39(2): 343-357. doi:10.1016/j. gtc.2010.02.012
- Patiño JF (2000) Acalculous cholecystitis. In: Patiño JF (Edt.), Surgery Lessons. Pan-American, Colombia, pp. 654-660.
- Rosas-González G, Carreño-Vásquez KW, Ramírez-Onofre CA (2017) Acute Alithiasic Cholecystitis: About a case in an adolescent patient. Health and Administration 4(11): 53-57.
- De La Fuente M, Catrip JM (2006) Alithiasic cholecystitis. Diagnostic certainty by ultrasound. Rev Gastroenterol 71(2): 122-126.
- Tokyo Guidelines 2018 (TG18). Recuperado de. http://www.jshbps.jp/ modules/en/index.php?content_id=47
- Duncan J (1844) Femoral hernia: Gangrene of the gallbladder; extravasation of bile; peritonitis death. North J Med 2: 151-153.
- Fei Zhou, Ting Yu, Ronghui Du, Guohui Fan, Ying Liu, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229): 1054-1062.
- Xiao F, Tang M, Zheng X, Liu Y, Xiaofeng L, et al. (2020) Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 158(6): 1831-1833. Doi: 10.1053 / j. gastro.2020.02.055.
- Singh R, Domenico Ch, Rao SD, Urgo K, Prenner SB, et al. (2020) Novel Coronavirus Disease 2019 in a Patient on Durable Left Ventricular Assist Device Support. Journal of Cardiac Failure 26(5): 438-439. . https://doi.org/10.1016/j.cardfail.2020.04.007.
- Puig G, Gimenez M, Campistol E, Caño V, Valcarcel J, et al. (2020) Development of concomitant diseases in COVID-19 critically ill patients. Revista Española de Anestesiología y Reanimación 68(1): 37- 40. https://doi.org/doi:10.1016/j.redar.2020.09.001.
- González L, López G, Santolaria S, García D, Ferrero M, et al. (2005) Colecistitis alitiásica: Una forma infrecuente de presentación de fiebre Q. Gastroenterol Hepatol 28(4): 232-236.
- Rueda E, Méndez A, González G (2002) Síndrome hemofagocítico asociado con dengue hemorrágico. Revistabiomedica org 22(2): 160- 166. https://doi.org/10.7705/biomedica.v22i2.1155.
- Senival O, Véras Th, Costa de Medeiros E, Dantas A, Carvalho C, De Sousa e Silva S, Meneses AC, Araújo I. Acute Acalculous Cholecystitis in Critically ill Patients: Risk Factors, Diagnosis and Treatment Strategies. JOP. Journal of the Pancreas. 2016; 17 (6): 580-6. Recuperado de https://pancreas.imedpub.com/acute-acalculous-cholecystitis-incritically- ill-patients-risk-factors-diagnosis-and-treatment-strategies. pdf
- Soria V, Galindo L, Flores D, Carrasco M, Aguayo JL (2017) ¿Es la colecistectomía el tratamiento de elección en la colecistitis aguda alitiásica? Revisión sistemática de la literatura. Rev Esp Enferm Dig 109(10): 708-718.
- Straverg SM (2008) Acute Calculous Cholecystitis. N Engl J Med 358: 2804-2811.
- Baron TH., Grimm IS, Swanstrom LL (2015) Interventional Approaches to Gallbladder Disease. N Engl J Med 373(4): 357-365. DOI: 10.1056/ NEJMra1411372.
- Palmieri A, Hernández LA, González C, Hernández KJ, Pérez JB, Tovío IP. Vólvulo de la vesícula biliar. Rev Colomb Cir. 2019; 34: 269-76. https:// doi.org/10.30944/20117582.446.
- American College of Surgeons (ACS) (2020) COVID-19 and surgery. Fecha de consulta: 12 de abril de. 2020. Disponible en: https://www. facs.org/covid-19.
- Torregrosa L, Prieto R, Cabrera LF, Ordoñez J, Sánchez E, et al. (2020) Recomendaciones generales para los Servicios de Cirugía en Colombia durante la pandemia COVID-19 (SARS-CoV-2). Rev Colomb Cir 35: 264- 280.https://doi.org/10.30944/20117582.633.






























