Eosinophilic Enteritis, A Rare Dissease
Andy Rivera*, Roberto Délano, Jose de Jesús Herrera Esquivel and Carlos Valenzuela Salazar
Endoscopy Unit, Hospital General, Manuel Gea González, México
Submission:October 10, 2020;Published:October 22, 2020
*Corresponding author:Andy Gabriel Rivera Flores, Endoscopy Unit, Hospital General, Dr Manuel Gea González, México City, México
How to cite this article:Andy Gl R F, Roberto D A. Eosinophilic Enteritis, A Rare Dissease. Adv Res Gastroentero Hepatol, 2020;16(1): 555930. DOI: 10.19080/ARGH.2020.16.555930.
Abstract
Eosinophilic enteritis is a rare disease characterized by eosinophilic infiltration in the small intestine; In the absence of non-gastrointestinal diseases that cause eosinophilia or causes known as parasites, medications, or malignancies.
Keywords: Eosinophilic enteritis; Endoscopy; Treatment
Introduction
Eosinophilic enteritis is a rare disease characterized by eosinophilic infiltration of the small intestine; In the absence of non-gastrointestinal diseases that cause eosinophilia [1]. It was described in 1937 by Kaijser. The pathophysiology of this entity is not well described. The symptoms are manifested according to the affected small intestine layer, the mucosa being the most common (25-100%) characterized by weight loss, anemia, positive stool guaiac; The Muscular (13-70%) presents data of intestinal obstruction; Subserosa presents with eosinophilic ascites [2]. Diagnosis is made by endoscopic findings (nodular, friable and ulcerated appearance of the small intestine) and more than 20-25 eosinophils per high-power field on microscopic examination, excluding other causes of eosinophilia (they are not really necessary for the diagnostic) [3]. The recommended treatment is Budesonide 9 mg per day for 2 to 4 weeks until clinical improvement and endoscopic control [4].
Case Report
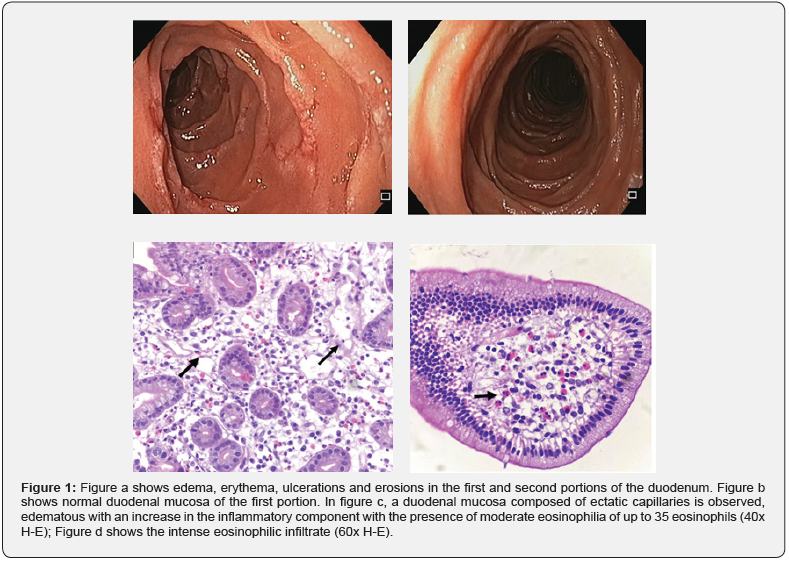
69-year-old female; with a history of smoking, gastroesophageal reflux disease, gastrointestinal bleeding secondary to gastric ulcer in antrum associated with Helicobacter Pylori, isolated systolic hypertension. She refers to a weight loss of 5kg, dyspepsia, incoercible vomiting and intolerance to the oral route of both liquids and solids with clinical data of dehydration, for which she goes to the emergency room, where she is evaluated and vital signs are observed within normal parameters. The physical examination revealed slight dryness of the mucosa, the rest without abnormalities. The results of the laboratory tests were within normal parameters (hematic biometry, 35-element blood chemistry, general urinalysis, thyroid profile). A Simple Complete Abdominal Computerized Axial Tomography was performed with oral and intravenous contrast, which demonstrated thickening of the proximal small intestine that does not occlude the intestinal lumen. Panendoscopy is performed where duodenal ulcers are observed in the first and second portion of the duodenum (Figure 1), taking biopsies of the duodenum and the Sydney protocol. The patient was initially managed with sucralfate, Itopride, Ilaprazole with an improvement of the symptoms, deciding her hospital discharge; On the third day, the histopathology report is received (Figure 1), starting treatment with budesonide 9mg orally every day for 4 weeks; At the end of the month of treatment, it was decided to perform a control panendoscopy, where the duodenum was observed without abnormalities (Figure 1).
Discussion
There is very little literature on this pathology; In Mexico there is a described case of eosinophilic gastroenteritis with clinical presentation of eosinophilic ascites in Sinaloa [1]. The precise diagnosis is complicated, however, when presenting endoscopic and histological findings, the diagnosis of eosinophilic enteritis can be considered, as was the case of the patient described above. The long-term prognosis is unknown [2,4-6].
References
- Rothenberg ME (2004) Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Inmunol 113(1): 11-28.
- Baig MA, Qadri A, Rasheed J (2006) A review of eosinophilic gastroenteritis. J NatlMedAssoci 98(10): 1616-1619.
- Zhang L, Duan L, Ding S, ShigangDing, Jingjing Lu, et al. (2011) Eosinophilic gastroenteritis: ClinicalManifestations and morphologicalcharacteristics, a retrospectivestudy of 42 patients. Scand J Gastroenterol 46(9): 1074-1080.
- Lee CM, Changchien CS, Chen PC, LinDY, SheenIS, et al. (1993) Eosinophilic gastroenteritis: 10 yearsexperience. AM J Gastroenterol88(1): 70-74.
- Talley NJ, Shorter RG, Phillips SF, ZinsmeisterAR (1990)Eosinofilic gastroenteritis; a clinicopathologicalstudy of patientswithdissease of the mucosa, musclelayer and subserosaltissues. Gut31(1):54-55.
- Schwartz DA, Pardi DS, Murray JA (2001) Use of monterlukast as steroid-sparingagent for recurrenteosinphilic gastroenteritis. DigDisSci 46(8):1787-1790.






























