Role of Incision Support Using Elastic Abdominal Binders in Reducing Postoperative Pain after Midline Laparotomy: A Randomized Controlled Trial
Byshetty Rajendar1*, Gomathi Shankar V2, Bala Mourugan2 and Sarath Chandra Sistla3
1Senior Resident, Department of surgery, JIPMER, India
2Assistant Professor, Department of surgery, JIPMER, India
3Professor (Senior Scale), Department of surgery, JIPMER, India
Submission:August 08, 2020;Published:September 15, 2020
*Corresponding author:Byshetty Rajendar, Department of surgery, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry-605006, India
How to cite this article:Byshetty R. Role of Incision Support Using Elastic Abdominal Binders in Reducing Postoperative Pain after Midline Laparotomy: A Randomized Controlled Trial. Adv Res Gastroentero Hepatol, 2020;15(5): 555924. DOI:10.19080/ARGH.2020.15.555924.
Keywords: Midline laparotomy; Chronic pain syndrome; Abdominal binders; Postoperative pain; Quality of life; Postoperative analgesia; 6 minute walk test
Abbreviations: VAS: Visual Anologue Scale; POD: Postoperative Day; ASIS: Abdominal Surgery Impact Scale; PEFR: Peak Expiratory Flow Rate; RCT: Randamized Controlled Trial; QOL: Quality of Life; 6MWT: 6 Minute Walk Test
Introduction
Midline laparotomies constitute a majority of intra-abdominal elective and emergency surgical procedures. Midline laparotomy results in postoperative effects on the patient, which include pain with subsequent immobilisation along with decreased pulmonary function and abdominal muscle laxity. Pain is the most incapacitating of all those mentioned, due to its effect on the physical condition and psyche of the patient. Pain after laparotomy is a frequent complication and the prevalence of pain after midline laparotomy is reported as high as 80%. Pain if inadequately treated will cause complications, which can range from short term complications which include hyperglycaemia, increased surgical site infection to long term complications like decreased quality of life and development of chronic pain syndrome [1]. Pain management includes various methods like use of drugs and several newer analgesic/ anaesthetic techniques. One of the simplest and cheapest mechanisms of the many studied and researched is the use of abdominal binders.
A binder is a contraption used to surround the abdomen circumferentially to support abdomen and incision site over the anterior abdominal wall [2]. They are widely used in different clinical conditions like in abdominal surgeries, spinal cord injury patients, post-Caesarean section to reduce post-operative pain, wound dehiscence, for early ambulation and to improve pulmonary function in post-operative period [3,4]. They are considered to be safe, comfortable, easy to use and acceptable to patients. Various studies have shown that abdominal binders are useful in controlling pain and distress following major abdominal surgeries [2,5,6]. An elastic abdominal binder worn around the abdomen can decrease stress on the incision during ambulation thereby decreasing pain. The contact provided by the binder with the abdominal wall can decrease pain generated at the incision due to gate control mechanism [7]. Application of the binder allows the patient to ambulate early leading to reduction of complications due to immobilization [2,5].
In patients who undergo laparotomy, pulmonary complications are one of the most important causes of morbidity in post operative period. Activities like deep breathing, coughing and ambulation which are very important in preventing pulmonary complications are impaired in post operative period because of various reasons like sedation, pain and fear of wound dehiscence. The application and use of abdominal binder provides the required support to abdomen and helps in aiding the patient to breathe deeply and effectively. A study showed the use of binder helps improve pulmonary status postoperatively. Few clinicians are still sceptical about its use arguing that it may reduce pulmonary function. This concept has been disproved by few studies which showed that the use of binder does not compromise pulmonary function [2,4,8,9] Some of them also argued that the use may lead to deep vein thrombosis due to increased intra-abdominal pressure [10]. Abdominal binders have also been criticized for causing discomfort to patients due to the rolling of its upper and lower edges. They may also impinge on the breast line of females.
Few trials are available in evaluating the benefits and risks of abdominal binders in abdominal surgical procedures. Majority of studies on the role of abdominal binder in enhancing patient comfort have not used validated questionnaires. There are minimal data on the specific relationship between abdominal binders and pulmonary function. So, this study was conducted to assess the effect of incision support using abdominal binders on post operative pain and comfort by using VAS score, quality of life by using abdominal surgery impact scale (ASIS), a validated tool to assess the quality of life in the immediate postoperative period and pulmonary function by PEFR [11].
Methodology
The study was conducted at the Department of Surgery at Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), India, between September 2015 and June 2017. All patients (≥18 years) , who underwent elective midline laparotomy were included. Patients who had a body-mass index (BMI) of 35 and above, patients with chronic obstructive respiratory disease, pregnant patients, patients with surgical stoma and epidural analgesia were excluded. With an expected difference in VAS score of 1.6 and considering the alpha error as 5% and power of the study as 80%, the sample size was calculated to be 32 in each group (total 64 cases). Block randomization was done by the principal investigator using a computer program with randomly selected block sizes of 4 and 6. Allocation concealment was ensured by serially numbered opaque sealed envelope (SNOSE) technique. Total of 64 patients were enrolled and randomized equally into binder group and non-binder group. Preoperative measurements like PEFR, and walking distance (evaluated with the 6-minute Walk Test) were taken and patients underwent midline laparotomy. Abdominal binder was applied to patients in the intervention group whereas it was not applied to patients in control group. From the binder group, 2 patients had to be excluded as they received top up epidural analgesia. From the non-binder group, 2 patients had to be excluded as stoma was constructed.
For patients in the intervention group, the elastic binder was applied over the abdominal surgical incision site so that upper border of the binder was not higher than the level of xiphisternum and ensuring minimal restriction of chest movement. The tension of the binder was determined by patient comfort; however, for optimum benefits, it was applied firmly (binder circumference 10% smaller than the patient’s postoperative abdominal circumference measured at the level of the umbilicus). Patients were instructed to wear the binder throughout the day until fifth postoperative day. A postoperative pain control protocol was applied to all patients uniformly. Accordingly, Injection paracetamol 1g was given intravenously every eight hours. Injection Morphine 0.1mg/kg was given every 8 hours alternatively with Injection paracetamol 1g for the first 2 days or till the patient is started orally. Once the patient is started on oral diet, tablet paracetamol 1 gram was given every eighth hourly. Injection morphine 0.1mg /kg was given as rescue analgesia if the VAS score was more than 4. The control group did not receive abdominal binder, but they received the standard treatment for surgery and pain control as described above.
patient’s baseline characteristics such as age, gender, diagnosis at admission; surgery performed, co-morbid conditions were noted. Pain was assessed using the ‘Visual Analog Scale ‘from POD 1 to 5 both during rest phase and during activity (Incentive spirometry and walking being considered as activities).Patients’ comfort was assessed using the ‘Visual Analog Scale’ from POD 1 to 5 during rest phase and activity (Incentive spirometry and walking were considered as activities). Visual analogue scale was used and it ranges score from a minimum of 0 (No distress/ discomfort) to a maximum of 10 (maximum discomfort). Pulmonary function was evaluated by a portable spirometer device. PEFR was measured on POD 3 and POD 5 by asking patient to do spirometer three times and the highest value was taken into account. On POD 5, patient’s physical fitness was assessed by 6-minute walk test. The test was conducted on a straight hospital corridor 100 m long. The corridor was measured in advance. Patient is asked to walk to and for and at the end of 6 minutes the total distance walked by the patient is calculated. Patient’s Quality of life was assessed with ‘Abdominal Surgery Impact Scale’ which has a pre-set questionnaire (18-items with 6 domains). The six domains included were pain, visceral function, sleep, physical limitations, psychological function and functional impairment. Patient was asked to answer 18 questions as mentioned in the pre- set questionnaire. Each item is scored on a seven-point Likert scale ranging from 1 to 7. The total score ranges from 18 to 126 as higher scores indicative of better quality of life.
Results
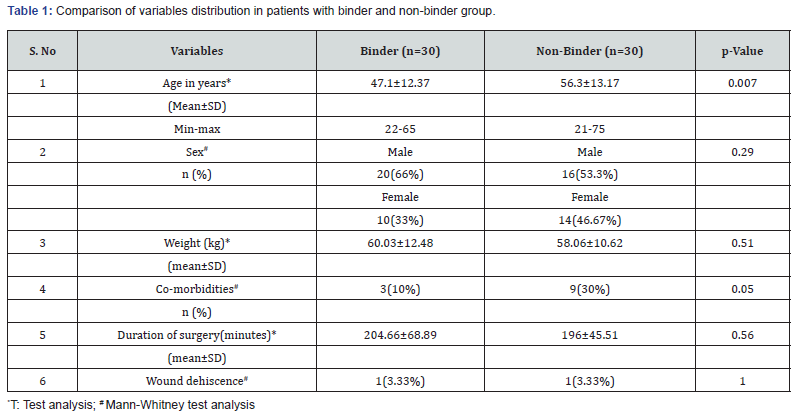
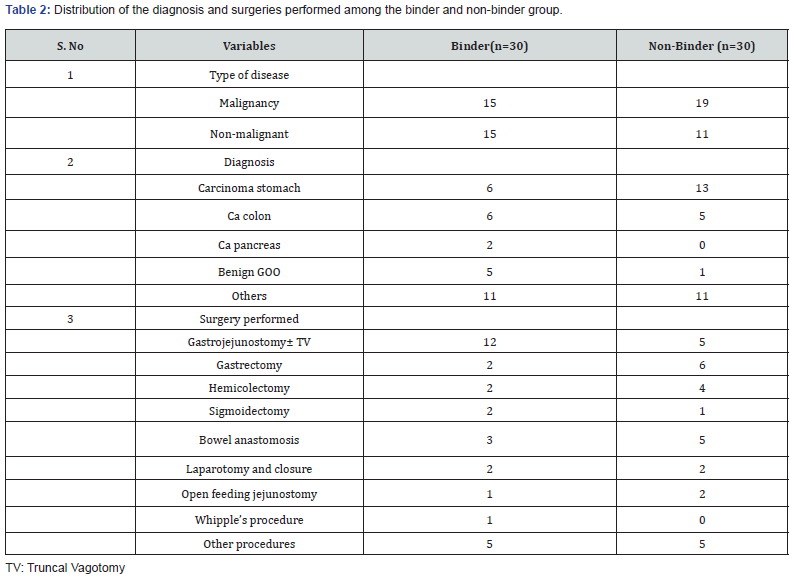
Both the groups were comparable in baseline characteristics like gender distribution, weight, duration of surgery. There is a statistical difference in age and co-morbidities of patients in both groups (Table 1). The other details of the patients such as various diagnoses, various surgeries performed were mentioned in the table 2
Pain at rest phase
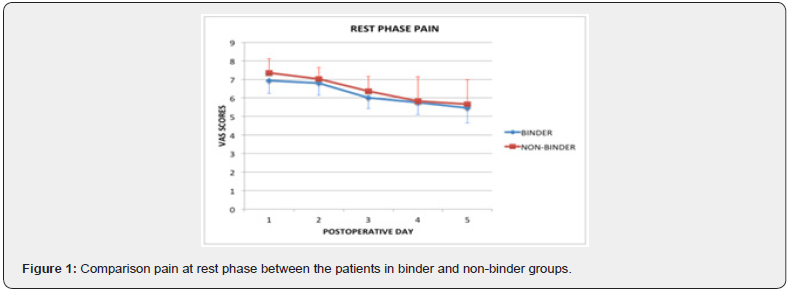
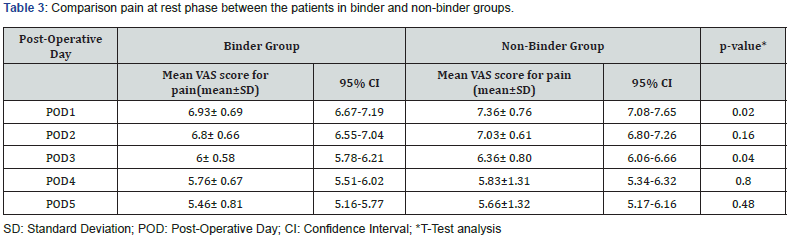
On POD1 and POD3 Post operative pain during rest as measured by VAS score is significantly less in the binder group than in the non-binder group; Mean (SD) VAS score in binder group versus non-binder group were 6.93(0.69) and 6 (0.58) versus 7.36(0.76) and 6.36 (0.80) respectively with p value of 0.02 and 0.04. On POD2, POD4, POD5 also pain experienced by patients in binder group was less compared to non-binder group, but the difference is statistically non-significant (Table 3 & Figure 1).
Pain during activity
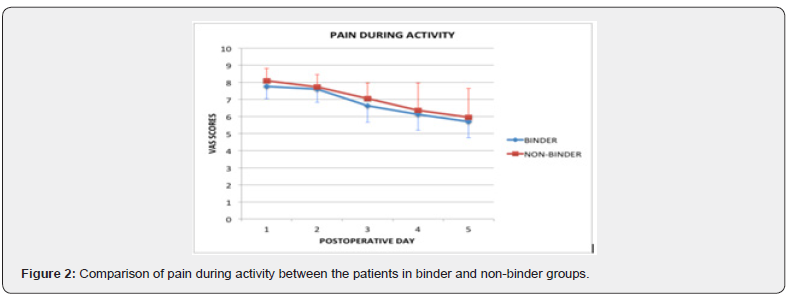
During first 5 post operative days mean VAS scores of patients in the binder group were less than that of the non-binder group. Pain during activity experienced by patients in binder group was less compared to non-binder group but difference is statistically not significant (Table 4 & Figure 2).

Comfort during rest
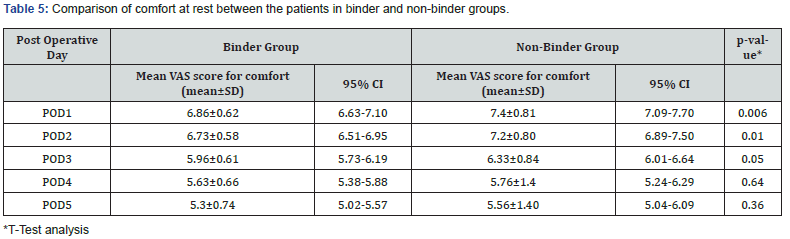
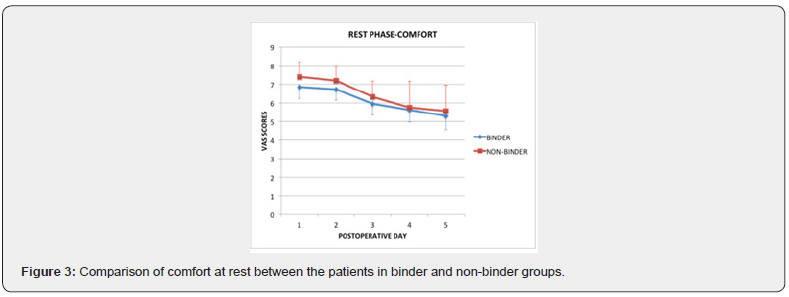
On POD1, POD2, POD3 comfort during rest as measured by VAS score was significantly better in binder group than in nonbinder group; Mean(SD) VAS score between binder versus nonbinder were 6.86(0.62), 6.73(0.58), 5.96(0.61) versus 7.44(0.81), 7.2(0.80), 6.33(0.84) respectively with p value <0.05. On POD 4 and POD5 also comfort experienced by patients in binder group was better compared to non-binder group, but the difference is statistically not significant (Table-5 & Figure 3).
Comfort during activity
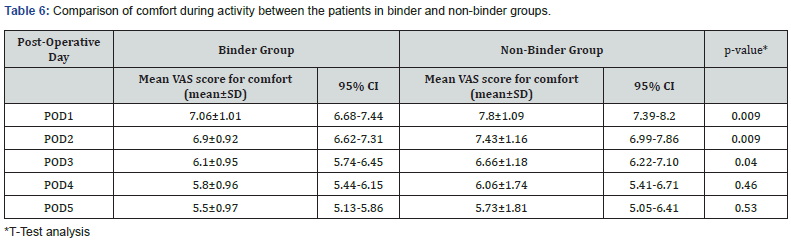
Patients’ comfort during activity on POD1 to POD3 was significantly better in binder group than in non-binder group. Mean (SD) VAS score in the binder versus non-binder were 7.06(1.01), 6.90(0.92) and 6.1(0.95) versus 7.8(1.09), 7.43(1.16) and 6.6(1.18) with p value 0.009, 0.09 and 0.04 on POD1, POD2 and POD3 respectively. On POD4 and POD5 also comfort experienced by patients in binder group was better compared to non-binder group, but the results were statistically not significant (Table-6 & Figure 4).
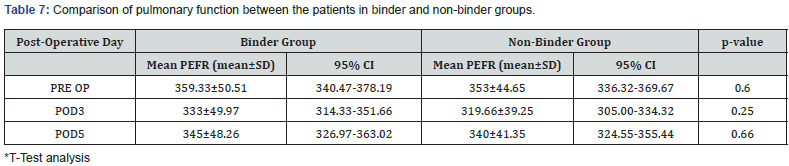
Pulmonary function
There was significant reduction of mean PEFR in postoperative period in both the groups compared to preoperative PEFR, with maximum decline on POD3.The mean (SD) PEFR of binder group in preoperative period was 359(50.5) as compared to 333(49.97) on POD3 and 345(48.26) on POD5. The mean (SD) PEFR of non-binder group in preoperative period was 353(44.65) as compared to 319(39.25) on POD3 and 340(41.35) on POD5. But there was no significant difference statistically between PEFR of both the groups (Table 7 & Figure 5).


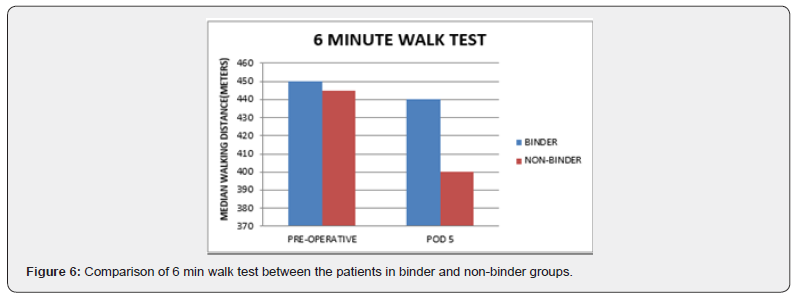
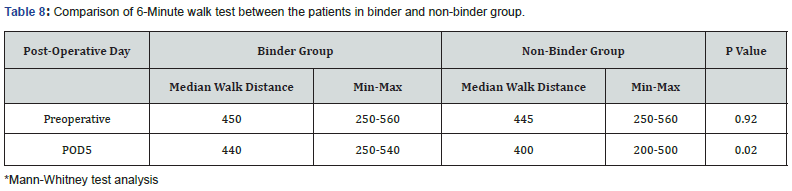
Physical fitness
Physical fitness as assessed by 6-minute walk test was significantly reduced in post-operative period in both the groups. Pre–operatively median walking distance of the binder group was 450 and non-binder group was 445. That difference was statistically not significant. On POD 5 median walking distance in binder group was 440 and the same in the non-binder group was 400. This difference was statistically significant with p value 0.02. The distance covered was significantly more in binder group than in non-binder group (Table 8 & Figure 6).
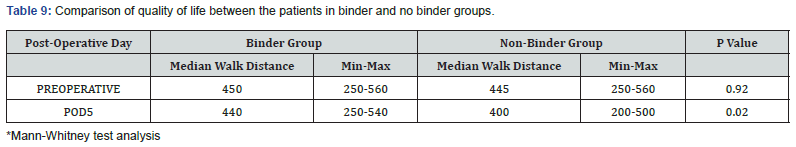
Quality of life
On POD3 and POD5, quality of life as measured by ASIS score was significantly better in binder group than in non-binder group; On POD 3, the median value of 82.5 in binder group versus 68 in non-binder group with p value of <0.05 .On POD 5 the median value of 105 in binder group versus 92 in non-binder group which was statistically significant (Table 9 & Figure 7).
Post-operative analgesia
According to protocol, on POD 1 & POD 2 analgesic used was the same. Total number of patients received rescue analgesia on POD 3 to POD 5 was calculated for both the groups. On POD 3, 53.33% of patients in the binder group received rescue analgesia and 85.33% of patients in non-binder group received rescue analgesia. This difference was therefore, statistically significant.
On POD 4 and POD 5, less percentage of people received rescue analgesia in binder group as compared to the non-binder group though the difference was statistically not significant (Table 10 & Figure 8).



Discussion
Midline laparotomy constitutes majority of the elective and emergency abdominal surgeries. The postoperative pain experienced can be very debilitating. Hence, it is essential to manage the pain effectively. There are numerous methods of pain management like use of drugs and several newer analgesic/ anaesthetic techniques [12]. One of the simplest, safest and accessible modalities is the use of abdominal binders [12].
Demographic variables effect on pain
Age: There was a statistically significant difference in the mean age of the patients in both groups. The mean age of the patients in the non-binder group was more than that of the patients in the binder group, being 56.3 years and 47.1 years respectively. Wander et al. conducted study on patients to study the effect of age on pain. They showed that the patients in older age were more sensitive to pain and more willing to report regarding the sensation of pain than their counterparts in the middle age [13]. In our study, patients in the Non-binder group were older than the patients in the binder group. This difference in age could have given difference in pain perception.
Gender: Women were shown to be more pain sensitive but had higher pain endurance than males and they were found to be more willing to report pain as compared to males [13,14]. In our study, the non-binder group has a preponderance of females with a possibility of higher pain scores than expected. Baseline characteristics like gender distribution, weight, duration of surgery were similar in both groups.
Postoperative Pain
VAS is simple, easy to understand for patients, validated scale so it was used in this study to assess postoperative pain. Shea et al. reported that postoperative pain was greater during activity than rest phase. Hence pain was assessed using VAS at rest and during activity in this study. It was observed that mean VAS scores of in binder group were less than the VAS scores in non-binder group. It was concluded that the patients in the binder group complained less pain than the patients in the non-binder group at rest phase and during activity. Binders helped in significant pain reduction in initial postoperative period. The mechanism that forms the basis of pain at the outset is the Gate Control Pathway. The abdominal binder causes the activation of A beta fibres in the anterior abdominal wall by touch and pressure. These A beta fibres cause inhibition of projection fibres which transmit pain sensation and hence the pain sensation not being felt due to the inhibitory mechanism. The results were similar to previous studies conducted by Clay & Arici et al. [6,7]. Chefeitz et al. [2] included a group of patients who underwent major abdominal surgery using laparotomy. They assessed pain using the Short form Mc Gill Pain questionnaire. They observed in their survey that binder group had less pain but it was not statistically significant.
Various studies done by Ali, Christofferson, Giller, Fagevic & Larson et al, [4,13-15] concluded that there was no difference in postoperative pain with application of binder. These studies had different result with present study might be because of some drawbacks these studies had in their methods. Fagevic et al. studied the effect of abdominal binder on postoperative pain using VAS and concluded that there was no effect. They had used epidural analgesia in each patient. This gave satisfactory pain relief so assessment of pain relief with binder in such category of patients was not warranted. Gillier et al, [4] used abdominal binders for women who underwent low transverse incision for caesarean section and Ali et al. studied in sub costal incision. Both showed that the binders had no significant effect on the pain. These studies were done in patients with low transverse incision and sub costal incision where binder use was doubtful as these include areas on upper and lower boundaries of the abdominal binder. Placement of binder in either boundaries of abdomen can impinge on surgical site and cause pressure on incision site and aggravate the pain. Christoffersen et al, [15] studied the effect of abdominal binder used postoperatively after laparoscopic umbilical and epigastric hernia repair. It was found to have no significant effect on pain. It was done in patients who underwent laparoscopic repair where binder role is not of any significance.
Types of surgeries were not similar in both groups of this study. Though the type of surgical insult has role in Surgery induced neuropathic pain (SNIP), it’s role in acute postoperative pain could not be established inspite of extensive literature review[58]. The patients in binder group were aware that they were wearing binder so there was a chance of bias in VAS pain scores. However, blinding was not possible due to the fact that binder is an externally worn visible contraption.
Postoperative Comfort
Distress caused by physical strain and mental anxiety is usually due to a temporary external cause. Comfort implies the feelings of relief after the cause of pain/distress/anxiety in a person is relieved. Abdominal Binder has been proposed to allay fear and anxiety thereby increasing comfort. Patient distress levels or in other words their comfort can be measured using VAS scale, Patients experienced more comfort during their initial postoperative period with binder application. Similarly, patients with binder experienced more comfort during activity. In a study by Fagevic et al, [14] VAS was used to compare postoperative comfort in binder and no binder group. It was found that majority of patients in binder group reported that using abdominal binder in the initial postoperative period was comfortable. Christofferson et al, [15] also commented that abdominal binder group reported subjective beneficial effects of binder.
Chieftz et al, [2] assessed patient perceived symptom associated distress by Adapted Symptom Distress Scale (ASDS-2). Binder group postoperative distress levels remained unchanged during entire postoperative period. In contrary, distress symptoms were increased significantly in the non-binder group. Giller et al, [4] used Symptom distress scale and it showed that there was no difference in comfort experienced by both the groups.
The study had many drawbacks as the duration of the study was very short , only two days and also most patients enrolled in the study included women in labor and immediately after delivery who were fatigued. There was also no defined period from point of time of caesarean section to assessment of pain/distress in the women, allowing variable amount of time for managing the subsequent pain and distress. This resulted in disparities in the reporting of pain/distress by women within the same group.
Quality of Life (QOL)
Quality of life is an assessment of a patient’s well-being or its lack in their daily life. QOL depends on physical factors and mental factors of which postoperative pain and comfort being the most important physical factors and postoperative subjective feelings of fear/anxiety are the essential mental factors. Preoperative use of incentive spirometry before major surgeries, use of abdominal binder postoperatively, walking and exercise preoperatively and postoperatively aid in the enhancement of QOL. Abdominal binders have its fair share of advantages in all factors which aiding in the enhancement of QOL. It effects physical factors by decreasing postoperative pain and improving comfort, also affects mental factors by decreasing fear or anxiety allowing patients to mobilize earlier and improves postoperative mobility which aid in enhancement of quality of life. Dutta et al. used ASIS to assess QOL in patients underwent Ileal Pouch Anal Anastomosis and proved internal validity of ASIS.
Out of 6 domains in ASIS, it was observed that the use of abdominal binders resulted in positive outcomes of decreased pain, increased comfort, decreased fear, undisturbed sleep, improved early mobilization and even provided the needed psychological support postoperatively. There was no effect on visceral function supported by studies done by Arici et al. [7] showing that there is no effect on gastrointestinal function. It was found that patients who used abdominal binder had significant improvement of quality of life both on POD 3 and POD in binder group.
Christofferson et al, [15] assessed the effect of binder in laparoscopic hernia repair patients wherein he concluded that it has no effect on quality of life. This study used Carolina comfort scale which is a validated scale. Quality of life will be affected more in midline laparotomy surgeries than in laparoscopic surgery. There were no other previous studies in which a valid questionnaire was used to evaluate effect of abdominal binder on patient’s quality of life.
Co-morbid conditions have much more significant effect on generic QOL measures rather than disease specific QOL measures. Co-morbid diseases significantly lower generic QOL scores[55]. In this study non-binder group had a higher rate of co-morbidities as compared to binder group.
Pulmonary Function
Effect of abdominal binder on pulmonary function is controversial. Few state that it worsens pulmonary function by restricting the expansion of chest while others argue that it improves respiratory function by providing support, reducing postoperative pain and promoting patient to take fuller, deeper breaths. In our study, abdominal binder was applied below the level of the xiphisternum to avoid restriction to expansion of chest. There was no significant difference in PEFR preoperatively between two groups and subsequently there was no significant difference between mean PEFR of both the groups post operatively on day 3 and day 5. It showed that application of abdominal binder didn’t affect the pulmonary function of the patients in binder group. The results are similar to studies by Larson, Clay, Fagevic, Chieftz & Arici et al. [2,6,7,13,14] who showed that there is no significant effect on pulmonary status with binder application. A previous study by Ali et al. showed an improvement of lung function with binder application which may be due to analgesia effect.
Physical Fitness
Postoperatively patients hesitate to move or get out of bed due to fear of pain or even sutures giving away leading to increased probability of potential complications like deep venous thrombosis, dependent area edema and pulmonary complications. The six-minute walk test devised by the American Thoracic Society is the most validated and has been used by us in the study to assess the post–operative functional status. This 6-minute walk test was found to be easy to administer, tolerated well even by patients with pre-operative respiratory disease and proved to be most reflective of the patients’ daily activities. Physical fitness was assessed on preoperatively and on postoperative day 5. There was no significant difference preoperatively between two groups but there was significant improvement in walking distance in binder group post operatively in 6-minute walk test. On POD5 walking distance was recovered by 97.7% of preoperative levels by the patients in the binder group wherein only 89% of preoperative distance was recovered by the patients in the non-binder group. It showed that there was effect of abdominal binder application on improvement of patient mobility and physical fitness in postoperative period. Binders supports abdominal wall thereby allays fear of wound gaping, decreases pain and improves comfort during ambulation so It helps in early mobilization thereby prevents complication like deep venous thrombosis, pneumonia et cetra. The results were similar to previous studies by Chieftz & Arici et al, [2,7] who showed improvement in walking distance postoperatively by using binders.
Fagevic et al, [14] showed no significant difference in mobility but used Hansdottir score, which was not validated. Thus this scale will not be able to compare the physical fitness of patients who can walk beyond 75 m after midline laparotomy. This explains why there was no difference between the physical fitness of the different groups.
Analgesia
A standard postoperative analgesia protocol was applied to all patients uniformly on POD 1 and POD 2 so analgesic used was same on those days. Thereafter Injection morphine 0.1mg /kg was given as rescue analgesia if the VAS score was more than 4. The percentage of people received rescue analgesia was less in binder group as compared to the non-binder group. The binder group need for these analgesics was compensated by the use of abdominal binder, which aided in the alleviation of the postoperative pain. The results are similar to a previous study by Ghana et al, [16] who found that the intervened group with an abdominal binder, consumed significantly less pain medications than the control group. Two patients in the present study had postoperative wound dehiscence on Day 5, one patient in each group. This study had analyzed only the effects of binder in the first five postoperative days. As the patients were not followed up till discharge, late wound dehiscence cannot be commented upon. In this study, short-term outcomes of placing abdominal binder in postoperative patients undergoing laparotomy were evaluated, but further follow up is needed for long term outcomes like incisional hernias. Fink et al. conducted a trial in patients undergoing midline laparotomies and found that incidence of incisional hernia was 12.6% at one year and 22.4% at three-year follow up. They concluded that minimum of 3 years of follow-up was mandatory to comment about the incisional hernia secondary to midline laparotomies [17].
Conclusion
In patients undergoing midline laparotomy, incision support using elastic abdominal binder resulted in less post-operative pain on the first three post-operative days. Incision support using elastic abdominal binder also resulted in better patient comfort and the post-operative quality of life as measured by abdominal surgery impact scale was also better in patients receiving support with binders. There were no adverse effects due to elastic abdominal binder. Based on our findings, we recommend routine use of incision support using elastic abdominal binder in patients undergoing midline laparotomy. Studies with long term follow up are needed to clarify the role of abdominal binders in preventing incisional hernias.
References
- Reardon DP, Anger KE, Szumita PM (2015) Pathophysiology, assessment, and management of pain in critically ill adults. Am J Health-Syst Pharm AJHP Off J Am Soc Health-Syst Pharm 72(18): 1531-1543.
- Cheifetz O, Lucy SD, Overend TJ, Crowe J (2010) The Effect of Abdominal Support on Functional Outcomes in Patients Following Major Abdominal Surgery: A Randomized Controlled Trial. Physiother Can 62(3): 242-253.
- Wadsworth BM, Haines TP, Cornwell PL, Paratz JD (2009) Abdominal binder use in people with spinal cord injuries: a systematic review and meta-analysis. Spinal Cord 47(4): 274-284.
- Gillier CM, Sparks JR, Kriner R, Anasti JN (2016) A randomized controlled trial of abdominal binders for the management of postoperative pain and distress after cesarean delivery. Int J GynecolObstet 133(2): 188-191.
- Melzack R, Wall PD (1965) Pain mechanisms: a new theory. Science 150(3699): 971-979.
- Clay L, Gunnarsson U, Franklin KA, Strigård K (2014) Effect of an elastic girdle on lung function, intra-abdominal pressure, and pain after midline laparotomy: a randomized controlled trial. Int J Colorectal Dis 29(6): 715-721.
- Arici E, Tastan S, Can MF (2016) The effect of using an abdominal binder on postoperative gastrointestinal function, mobilization, pulmonary function, and pain in patients undergoing major abdominal surgery: A randomized controlled trial. Int J Nurs Stud 62: 108-117.
- Zhang HY, Liu D, Tang H, Sun SJ, Ai SM, et al. (2016) The effect of different types of abdominal binders on intra-abdominal pressure. Saudi Med J 37(1): 66-72.
- Urbach DR, Harnish JL, McIlroy JH, Streiner DL (2006) A measure of quality of life after abdominal surgery. Qual Life Res 15(6): 1053-1061.
- Harsoor S (2011) Emerging concepts in post-operative pain management. Indian J Anaesth 55(2): 101-103.
- Wandner LD, Scipio CD, Hirsh AT, Torres CA, Robinson ME (2012) The perception of pain in others: how gender, race, and age influence pain expectations. J Pain Off J Am Pain Soc 13(3): 220-227.
- Berkley KJ (1997) Sex differences in pain. Behav Brain Sci 20(3): 371-380.
- Larson CM, Ratzer ER, Davis-Merritt D, Clark JR (2009) The effect of abdominal binders on postoperative pulmonary function. Am Surg 75(2): 169-171.
- FagevikOlsén M, Josefson K, Wiklund M (2009) Evaluation of abdominal binder after major upper gastrointestinal surgery. Adv Physiother 11(2):104-110.
- Christoffersen MW, Olsen BH, Rosenberg J, Bisgaard T (2015) Randomized Clinical Trial on the postoperative use of an abdominal binder after laparoscopic umbilical and epigastric hernia repair. Hernia 19(1): 147-153.
- Ghana S, Hakimi S, Mirghafourvand M, Abbasalizadeh F, Behnampour N (2017) The Effects of Abdominal Binder on Wound Healing and Consumed Pain Medications After Cesarean Section: A Randomized Control Trial. Iran Red Crescent Med J19(4).
- Fink C, Baumann P, Wente MN, Knebel P, Bruckner T, Ulrich A, et al. (2014) Incisional hernia rate 3 years after midline laparotomy. Br J Surg101(2):51-54.






























