Platelet to Lymphocyte Ratio and Neutrophil to Lymphocyte Ratio Changes Significantly in Case of Helicobacter Pylori Infection Irrelevant of Inflammation Degree
Yusuf Serdar Sakin1*, Alpaslan Tanoglu2, Kadir Öztürk1, Fatih Özçelik3, Tolga Duzenli4, Seyit Ahmet Uslu5, Yusuf Yazgan2 and Ahmet Uygun1
1Department of Gastroenterology, University oh Health Sciences, Gulhane School of Medicine, Ankara, Turkey
2Department of Gastroenterology, University of Health Sciences, Sultan 2. Abdulhamid Han Training and Research Hospital, Istanbul, Turkey.
3Department of Medical biiochemistry, University of Health Sciences, Sultan 2. Abdulhamid Han Training and Research Hospital, Istanbul, Turkey.
4Department of Gastroenterology, Hitit University, Erol Ucok Training and research hospital, Corum, Turkey
5Department of Internal Medicine, University of Health Sciences, Sultan 2. Abdulhamid Han Training and Research Hospital, Istanbul, Turkey
Submission:February 03, 2020;Published:August 24, 2020
*Corresponding author:Yusuf Serdar Sakin, Department of Gastroenterology, Gulhane School of Medicine, Ankara, Turkey
How to cite this article:Yusuf SS, Alpaslan T, Kadir O, Fatih O, Tolga D, et al. Platelet to Lymphocyte Ratio and Neutrophil to Lymphocyte Ratio Changes Significantly in Case of Helicobacter Pylori Infection Irrelevant of Inflammation Degree. Adv Res Gastroentero Hepatol, 2020;15(5): 555921. DOI: 10.19080/ARGH.2020.15.555921.
Abstract
Introduction:The correlation between inflammatory markers and Helicobacter pylori (HP) infection has been investigated by previous studies. There are conflicting results about the diagnostic utility of the mean platelet volume (MPV), Platelet to Lymhocyte Ratio (PLR) and neutrophil to lymphocyte ratio (NLR) indices as a marker of inflammation in patients diagnosed with HP infection. We aimed to determine the relationship between HP infection and these novel indices.
Methods:The study enrolled 390 consequent patients who underwent esophagogastroduodenoscopy due to dyspepsia. Patients were divided into two groups according to the presence of histologically proven HP (HP positive vs. HP negative). Complete blood count variables including MPV, PLR and NLR values were recorded. Statistical analyses were performed to determine the correlations between MPV, PLR and NLR indices and HP positivity
Results:Out of the 390 cases, 290 (73%) were HP positive and 100 (27%) were HP negative. We found significantly higher MPV, PLR and NLR values in patients with HP infection when compared to control group. NLR level was found to be strongly correlated with the existence of HP infection.
Conclusion:Serum NLR, PLR and MPV levels could be a good predictor of inflammation in HP infection irrevelant of the degree of the inflammation. Further prospective studies are needed to determine the efficacy of serum MPV and NLR level in determining inflammation in HP infection.
Keywords: Helicobacter pylori; Mean platelet volume; Neutrophil to lymphocyte ratio; Mean Platelet volume to platelet ratio; Inflammation
Abbreviations:HP: Helicobacter Pylori; NLR: Neutrophil to Lymphocyte Ratio; MPV: Mean Platelet Volume; PLR: Platelet to Lymphocyte Ratio; CBC: Complete Blood Count; SD: Standard Deviation; ROC: Receiver Operating Characteristics
Introduction
Helicobacter pylori (HP) infection is a well-known provoking agent for gastritis and peptic ulcer disease and one of the most commonly encountered chronic bacterial infections [1]. Its role in a variety of extra-intestinal manifestations and inflammation has also been reported previously [2]. The use of biochemical markers for the assessment of systemic inflammation has gained wide interest recently due to their cost effectiveness and easy accessibility. Among these markers are the mean platelet volume (MPV), Platelet to Lymphocyte Ratio (PLR) and Neutrophil to lymphocyte ratio (NLR) indices, which have been found to be reliable indicators of systemic inflammation [3-6]. Although previous studies have attempted to identify a relationship between these inflammatory markers and the presence of HP infection, no specific marker for HP infection has been identified yet [3]. Although these novel inflammatory markers have been studied in HP infection, there are conflicting results about correlation with inflammatory markers such as NLR and PLR in recent studies [5, 7-10]. Thus, the purpose of this study was to determine the relationship between HP associated inflammation and MPV, PLR and NLR.
Materials and Methods
This study was a retrospective, two-centered study of patients with dyspeptic complaints and endoscopically proven H. pylori positive or negative gastritis that were followed up at the GATA Haydarpasa Training, and Gulhane Military Medical Academy hospitals in Istanbul and Ankara respectively between January 2016 and July 2018. The study enrolled 390 consequent patients who underwent esophagogastroduodenoscopy due to dyspepsia. Patients with chronic conditions (renal and cardiac diseases or diabetes mellitus, rheumatic diseases, hematological diseases, and chronic obstructive lung diseases) or a history of hypertension, coinfection with hepatitis B or C virus, HIV and hepatitis D virus, malignancy or autoimmune disorders were excluded from the study. Other criteria for exclusion were the history of usage of drugs such as aspirin, heparin, warfarin, and anti-hyperlipidemic, antidiabetic and anti-hypertensive drugs.
Complete blood count (CBC) analysis was performed by using a fully automated hematologic analyzer (Cell-Dyn Sapphire; Abbott Diagnostics, Lake Forest, Illinois, USA). The CBC values were retrieved from institutional review board approved electronic databases and patient notes. All patients had previously undergone esophagogastroduodenoscopy for the evaluation of dyspeptic symptoms. The existence of H. Pylori infection was confirmed by histopathological examination that was performed by obtaining two specimens each from the antrum, corpus and incisura angularis. Experienced pathologists evaluated collected specimens.
Statistical analysis
Continuous variables that followed normal distributions are expressed as mean standard deviation (SD). Variables that did not follow normal distributions are summarized in terms of their medians and ranges. Categorical variables were analyzed using the chi-square test or Fisher’s exact test. Comparisons of normally distributed continuous variables were performed using. Student’s t-test or one-way analysis of variance (ANOVA). The Mann-Whitney U-test or the Kruskal-Wallis test was used when a variable was not normally distributed. The Cohen’s kappa test was used to analyze intra-group correlations. Receiver operating characteristics (ROC) curve analysis was used to identify optimal cutoff values of MPV and NLR levels to identify maximum sensitivity and specificity for the detection of H. pylori infection. P-value <0.05 was set as statistically significant. This study was approved by the local ethics committee. All data were entered and analyzed using the Statistical Package for Social Sciences, version 19.0 (SPSS Inc., Chicago, IL, USA). P-values less than 0.05 were considered statistically significant.
Results
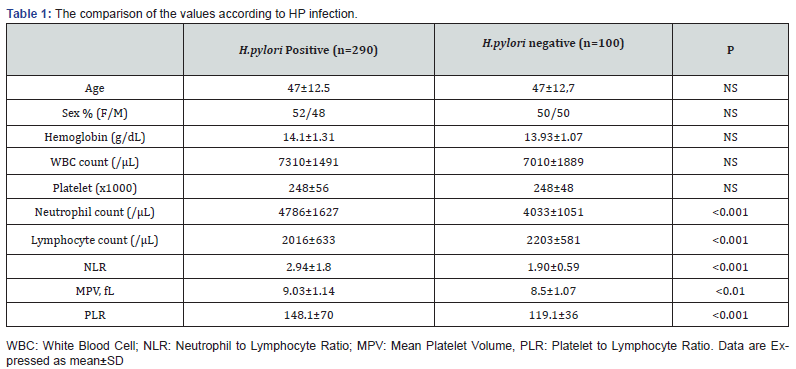
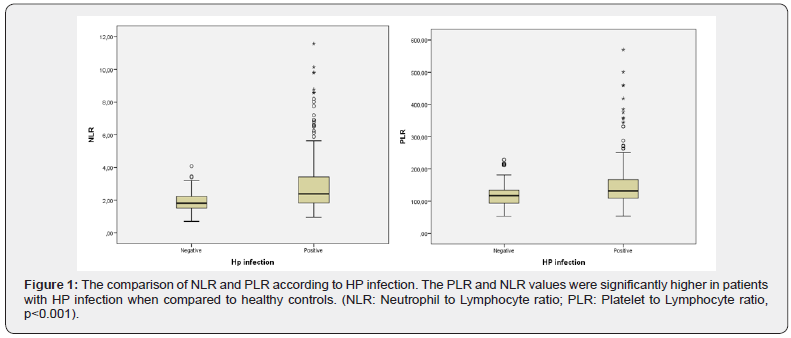
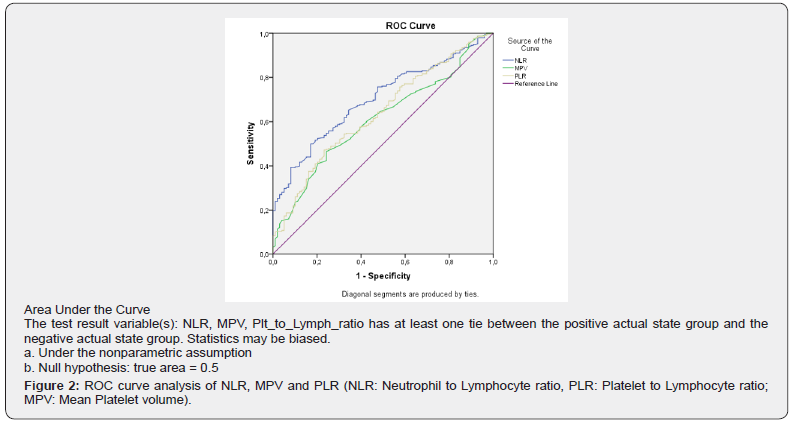
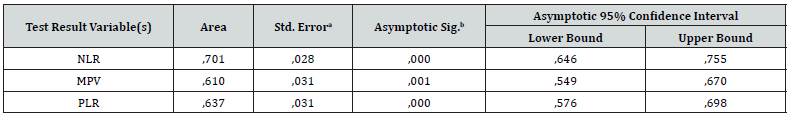
Of the 390 consequent cases, 290 (74.4%) were HP positive and 100 (25.6%) were HP negative. Patients’ characteristics and laboratory results are shown in table 1. In HP positive patients, the MPV, NLR and MPV-platelet ratio were significantly different from HP negative patients (Table 1). HP positive patients had significantly higher MPV (9.03±1.14 vs. 8.5±1.07, p<0.001), PLR (148.1±70 vs119.1±36, p<0.001) and NLR (2.94±1.8 vs. 1.90±0.59, p<0.001) than HP negative patients (Figure 1). ROC curve analysis for the diagnostic performance of MPV, PLR and NLR in identifying H. pylori infection is shown in figure 2. Area under the curve (AUC) values for MPV, PLR and NLR were 0.610 (0.549-0.670, p<0.01), 0.637(0.576-0.698, p<0.001) and 0.701 (0.646-0.755, p<0.001), respectively. Additionally, ROC curve analysis suggested that the optimum MPV cut-off point for H. pylori positive patients was 8.54 fl with 65% sensitivity and 52% specificity. The cut-off value of 1.81 for NLR was associated with a strong correlation with 76% sensitivity and 52% specificity. Moreover, for PLR, the cut-off value of 117.6 was associated with 65% sensitivity and 51% specificity.
Discussion
The present study aimed to determine a possible relationship between inflammatory markers MPV, PLR and NLR in HP positive and negative patients. A strong correlation between HP infection and NLR values but weaker correlation with MPV and PLR were found. Findings from this study support the notion that HP infection is a cause of systemic inflammation.
To date, very few studies have investigated a correlation between inflammatory markers and the presence of HP infection, and the results were contradictory [9,10]. Although novel disease biomarkers have been identified, most of them are either expensive or nonspecific. The MPV is known as a predictor of inflammation and its intensity [4]. In addition, elevated MPV levels have been shown to be associated with inflammatory diseases such as hepatitis B, thrombocytopenia, acute pulmonary embolism, congestive heart failure, and autoimmune disorders [11-13]. In current literature, there are conflicting results about the correlation between serum MPV levels and HP infection [7-10]. In a study by Dogan et al., no difference between MPV levels and HP positivity was identified [8]. However, Umit et al. found elevated MPV levels in HP positive patients in a recent study [6]. Additionally, Umit et al. mentioned in their study that this elevation might be due to the effect of HP infection on the process of platelet destruction. Similarly, we found significantly higher MPV levels in HP positive patients when compared to their negative counterparts, but different from these studies, we also analyzed another platelet function marker the MPV/platelet ratio and found similar values between groups. The MPV is thought to be an indicator of rapid thrombopoiesis and the levels may increase because of platelet destruction. Elevated MPV levels can also be due to the increased amount of young platelets in the blood stream and this may be associated with inflammation in H. pylori infection. The normal MPV/platelet ratio and higher NLR results from our study suggest that MPV increase is due to inflammation in H. pylori positive patients instead of platelet destruction.
The NLR and PLR are simple and easily available markers of inflammatory response, which correlates with prognosis in advanced disease states. NLR integrates data from two distinct pathways, lymphocytes, which portray the regulatory pathway, and neutrophils, which cause ongoing inflammation [14,15]. NLR ratio has been studied in various inflammatory diseases such as Behçet’s disease, inflammatory bowel diseases, hepatocellular cancer, chronic hepatitis B, and various cancers [16-21]. Although the correlation between NLR and HP infection has been shown in previous studies [5,9], a recent study from Korea did not find any correlation between inflammatory markers such as NLR and PLR with HP infection. Due to these conflicting results, we analyzed PLR and NLR ratios in our patients, and found that HP infection was associated with inflammatory markers NLR and PLR. This significance seems to be the result of both higher neutrophil count and lower lymphocyte count in HP positive patients.
Additionally, they found that there was a significant correlation between the presence of HP infection and NLR with an optimal cut-off level of 1.81 for NLR with high sensitivity and specificity. In our study, although the cut-off level for NLR was calculated as 1.81, sensitivity and specificity were found to be lower when compared to the previous study [5].
We analyzed the NLR, PLR and MPV according to histopathological inflammation degree of H. pylori inflammation. However, we did not find any difference between patients according to the degree of gastric inflammation. This result was contradictory to the study of Farah et al. [5]. However, our strict and detailed inclusion and exclusion criterion may cause this contradictory. Thus, more studies are needed to confirm or refute the association between gastric inflammation degree and MPV, PLR and NLR levels.
In this current research, we assessed the association between HP infection and inflammation by reliable blood inflammation indicators such as MPV, PLR and NLR, and found that HP infection seems to be associated with systemic inflammation. Additionally, in comparison of NLR, PLR and MPV levels, NLR was found to be strongly correlated with the presence of HP infection. This study has some limitations. First, we did not include other inflammatory markers such as C-reactive protein (CRP) and fibrinogen into this comparative analysis of the groups. In addition, this study is a retrospective study thus the findings would have to be confirmed in prospectively designed studies. In conclusion, we showed in this study that NLR, PLR and MPV significantly changes irrelevant of the inflammation degree in patients with HP infection. Furthermore, elevated MPV levels maybe more favorable predictor for HP infection rather than markers in case of dyspepsia. Further prospective studies required to determine the diagnostic efficacy of serum MPV, PLR and NLR levels in determination of HP infection.
References
- Suzuki S, Esaki M, Kusano C Chika K, Hisatomo I, Takuji G (2019) Development of Helicobacter pylori treatment: How do we manage antimicrobial resistance? World J Gastroenterol25(16):1907-1912.
- Wong F, Rayner-Hartley E, Byrne MF (2014) Extraintestinal manifestations of Helicobacter pylori: a concise review. World J Gastroenterol20(34):11950-11961.
- Pellicano R, Oliaro E, Fagoonee S, Astegiano M, Berrutti M, et al. (2009) Clinical and biochemical parameters related to cardiovascular disease after Helicobacter pyloriInt Angiol28(6):469-473.
- Karagöz E, Tanoğlu A, Ülçay A, Hakan E, Vedat T,et al. (2016) Mean platelet volume and red cell distribution width to platelet ratio for predicting the severity of hepatic fibrosis in patients with chronic hepatitis C. Eur J Gastroenterol Hepatol28(7):744-748.
- Farah R, Khamisy-Farah R (2014) Association of neutrophil to lymphocyte ratio with presence and severity of gastritis due to Helicobacter pylori J Clin Lab Anal28(3):219-223.
- Umit H, Umit EG (2015) Helicobacter pylori and mean platelet volume: a relation way before immune thrombocytopenia? Eur Rev Med Pharmacol Sci19(15):2818-2823.
- Topal F, Karaman K, Akbulut S, Dincer N, Dölek Y, et al. (2010) The relationship between mean platelet volume levels and the inflammation in Helicobacter pylori J Natl Med Assoc102(8):726-730.
- Dogan Z, Filik L, Ergul B (2013) Association between Helicobacter pylori and liver-to-spleen ratio: a randomized-controlled single-blind study. Eur J Gastroenterol and Hepatol 25(1):107-110.
- Kaplan M, Ates I, Yuksel M, Arikan MF, Aydog G, et al. (2018)The role of the PLR-NLR combination in the prediction of the presence of Helicobacter pylori and its associated complications.Saudi J Gastroenterol24(5):294-300.
- Kim TJ, Pyo JH, Lee H, Baek SY, Ahn SH, et al. (2018)Lack of Association between Helicobacter pylori Infection and Various Markers of Systemic Inflammation in Asymptomatic Adults.Korean J Gastroenterol72(1):21-27.
- Demirin H, Ozhan H, Ucgun T, Celer A, Bulur S, Cil H,et al. (2011) Normal range of mean platelet volume in healthy subjects: insight from a large epidemiologic study. Thromb Res128(4):358-360.
- Ommen SR, Hodge DO, Rodeheffer RJ, McGregor CG (1998) Thomson SP, Gibbons RJ. Predictive power of the relative lymphocyte concentration in patients with advanced heart failure. Circulation97(1):19-22.
- Avanzas P, Quiles J, López de Sá E, Sánchez A, Rubio R, et al. (2004) Neutrophil count and infarct size in patients with acute myocardial infarction. Int J Cardiol97(1):155-156.
- Kekilli M, Tanoglu A, Sakin YS, Kurt M, Ocal S, et al. (2015) Is the neutrophil to lymphocyte ratio associated with liver fibrosis in patients with chronic hepatitis B? World J Gastroenterol21(18):5575-5581.
- Azab B, Jaglall N, Atallah JP, Lamet A, Raja-Surya V, et al. (2011)Widmann WD. Neutrophil-lymphocyte ratio as a predictor of adverse outcomes of acute pancreatitis. Pancreatology11(4):445-452.
- Azab B, Bhatt VR, Phookan J, Murukutla S, Kohn N, et al. (2012) Usefulness of the neutrophil-to-lymphocyte ratio in predicting short- and long-term mortality in breast cancer patients. Ann Surg Oncol19(1):217-224.
- Cedrés S, Torrejon D, Martínez A, Martinez P, Navarro A, et al. (2012) Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancer. Clin Transl Oncol14(11):864-869.
- Gomez D, Farid S, Malik HZ, Young AL, Toogood GJ, et al. (2008) Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J Surg32(8):1757-1762.
- Markar SR, Karthikesalingam A, Falzon A, Kan Y (2010) The diagnostic value of neutrophil: lymphocyte ratio in adults with suspected acute appendicitis. Acta ChirBelg110(5):543-547.
- Torun S, Tunc BD, Suvak B, Yildiz H, Tas A, et al. (2012) Assessment of neutrophil-lymphocyte ratio in ulcerative colitis: a promising marker in predicting disease severity. Clin Res Hepatol Gastroenterol36(5):491-497.
- Duffy BK, Gurm HS, Rajagopal V, Gupta R, Ellis SG, et al. (2006) Usefulness of an elevated neutrophil to lymphocyte ratio in predicting long-term mortality after percutaneous coronary intervention. Am J Cardiol97(7):993-996.






























