Carvedilol Versus Propranolol for Secondary Prophylaxis of Variceal Hemorrhage in Patients with Liver Cirrhosis
Hamal AB1, KC S1, Thapa P1, Sharma D1, Karki ND1, Khadka S1, Jaishi B1, Shrestha JK1, Prajapati S1, Budhathoki SS2 and Tiwari PS1
1 Liver Unit, National Academy of Medical Sciences, Nepal
2 School of Public Health & Community Medicine, B. P. Koirala Institute of Health Sciences, Nepal
Submission:July 03, 2020; Published:August 17, 2020
*Corresponding author:Achyut Bikram Hamal, Liver Unit, National Academy of Medical Sciences, Bir Hospital, Nepal
How to cite this article:Hamal AB, KC S, Thapa P, Sharma D, Karki N, et al. Carvedilol Versus Propranololol for Secondary Prophylaxis of Variceal Hemorrhage in Patients with Liver Cirrhosis. Adv Res Gastroentero Hepatol, 2020;15(4): 555920. DOI: 10.19080/ARGH.2020.15.555920.
Abstract
Introduction: Portal Hypertension in cirrhosis can have complication of variceal bleeding in 30-40 % of cases. The risk of index variceal bleeding is about 5-15 % per year. Prevention for index bleeding include non-selective beta blockers and endoscopic variceal ligation (EVL). Though propranolol is used as secondary prophylaxis in variceal bleeding, carvedilol is not commonly used. This study compares the efficacy of carvedilol and propranolol in preventing rebleed from esophageal varices in cirrhotic patients.
Methods: It is an open label prospective comparative study. Cirrhotic patients with index variceal bleeding were treated with EVL and Propranolol or Carvedilol. They were followed up and mean arterial pressure (MAP), Heart Rate (HR) and number of EVL sessions needed were analyzed in both the groups at 2, 6 and 12 weeks. The change in MAP and HR from the baseline was seen at 6 weeks. The adverse effect and overall mortality were seen in both the groups.
Results: There were 25 patients in propranolol group and 22 patients in carvedilol group. The decrease in MAP and HR at 2 weeks were higher in carvedilol than propranolol however not statistically significant. The decrease in HR at 6 weeks was significantly higher in carvedilol than propranolol group (p=0.036). The rebleeding at least once within 6 months was also higher in propranolol group than carvedilol group (32 vs 22.7%). The overall mortality in 6 months in carvedilol group was 18% which was higher than that in propranolol group (8%).
Conclusion:This shows that carvedilol was as efficacious as propranolol for secondary prophylaxis of variceal bleeding.
Keywords: Acute Variceal bleeding; Carvedilol; Propranolol Secondary prophylaxis; Variceal bleeding;
Abbreviations: EVL: Endoscopic Variceal Ligation; MAP: Mean Arterial Pressure; HR: Heart Rate; AASLD: American Association for the Study of Liver Diseases; HCV: Hepatitis C Virus; LEV: Large Esophageal Varices; NASH: Non- Alcoholic Steatohepatitis; PHG: Portal Hypertensive Gastropathy; SEV: Small Esophageal Varices; SI: Splenic Index
Introduction
Bleeding occurs in 30% - 40% of cirrhotic patients once varices have formed [1]. The incidence of first variceal bleeding in cirrhosis is about 5-15% per year [2] that occurs at a threshold of Hepatic venous pressure gradient (HVPG) > 12mm Hg [3] with mortality rate of 17-57 percent [4]. Nonselective beta blocker is considered for secondary prophylaxis to further decrease rebleeding from 38% to 14% (P =.006) [5]. Carvedilol, a nonselective beta and alpha-1 blocker decreases the intrahepatic resistance and is 2-4 times potent than propranolol [6]. Three-fourth of patients in carvedilol and half of the patients in propranolol were HVPG responders (decrease in HVPG < 12 mm Hg) when used for secondary prophylaxis in variceal bleeding and percentage of decrease in mean arterial pressure (MAP) is more in carvedilol than that in propranolol [7]. We aimed to compare the efficacy of carvedilol and propranolol in secondary prophylaxis of variceal hemorrhage and identify the side effects of carvedilol and propranolol in cirrhotic patients.
Methods
This was a hospital based open label prospective comparative study carried out in the Liver Unit of Bir hospital from September 2019 to May 2020.
Consecutive patients of Child’s A and B liver cirrhosis (LC) with index presentation of acute variceal bleeding either esophageal or type 1 gastroesophageal varices (GOV) [1] were included. Acute variceal bleeding was defined as hematemesis within last 24 hours of presentation, and/or ongoing melena, with last melanic stool within last 24 hours in a known or suspected case of portal hypertension [8]. Patients not giving consent, with spontaneous bacterial peritonitis, hepatocellular carcinoma or portal vein thrombosis and other comorbid illness such as acute kidney injury, chronic kidney diseases, diagnosed coronary artery disease (need for cardio selective beta blockers), bronchial asthma, chronic obstructive pulmonary diseases, bradycardia, hypotension, congestive heart failure or uncontrolled diabetes were excluded.
The patients with first acute variceal bleeding were admitted resuscitated and treated with somatostatin analogue (octreotide) or terlipressin for 3 days along with endoscopic variceal ligation (EVL). Variceal hemorrhage was confirmed by upper GI endoscopy that was done within 12- 24 hours of admission. Esophageal varices were categorized as large (> 5mm) or small (< 5mm) as per American Association for the Study of Liver Diseases (AASLD) 2007 guidelines [9]. EVL consists of the placement of rubber rings on variceal columns which are sucked into a plastic hollow cylinder attached to the tip of the endoscope. Nonselective beta blocker was added after the stabilization of blood pressure on the 6th day of EVL.
The dose of propranolol for secondary prophylaxis was started as 20 mg twice daily with increment as needed up to maximum of 160mg and carvedilol was started with 3.125mg twice daily with increment of 3.125mg every 3rd day to achieve the target heart rate between 55 and 60 beats/min or decrease in the heart rate by 25% from the baseline or intolerance to the b blockers whichever happened earlier. The maximum dose of 160 mg daily for propranolol and 25 mg daily for carvedilol was planned. These drugs were continued until there were any serious side effects. MAP and Heart Rate (HR) of the patients with the lab parameters were studied in follow up at second, sixth and twelfth weeks. The patients were followed up every month till the eradication of the varices during which the liver function tests were done. Any variceal rebleeding was assessed with the help of history of hematemesis or melena along with fall in hemoglobin and clinical examination. The patients were followed up for 6 months and mortality was noted in both the groups. The data from the proforma was entered in Microsoft excel software. The data was cleaned, and coding was done. The data was then exported to SPSS version 20 software for analysis.
Descriptive analysis consisted for presenting the continuous data in mean and standard deviation, while frequency and percentages were mere mentioned for categorical data. Inferential statistics consisted of comparing the groups using chi-square test or Fischer exact test for categorical data; and unpaired t-test or Mann-Whitney test for continuous data. For statistical significance, p value of <0.05 was considered.
Results
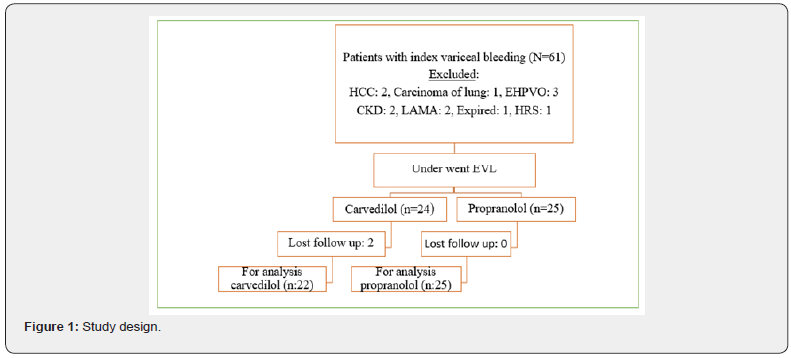
The total number of patients with index acute variceal bleeding was sixty-one. Out of 61, forty-nine patients were eligible for the enrollment. Two patients of hepatocellular carcinoma (HCC), one patient of Carcinoma of lung, 3 patients of extrahepatic portal vein obstruction (EHPVO), 2 patients of chronic kidney disease (CKD), 2 patients who left against medical advice (LAMA), one patient of Hepatorenal syndrome (HRS) and one patient expired, were excluded. Among them, 24 patients received carvedilol and 25 of them received propranolol by simple random sampling. Two patients in the carvedilol group lost in follow up. The study design of the patients is shown in Figure 1.

There was no difference in baseline characteristics except age of the patients in the two groups (Table 1).
Effects on hemodynamic parameters
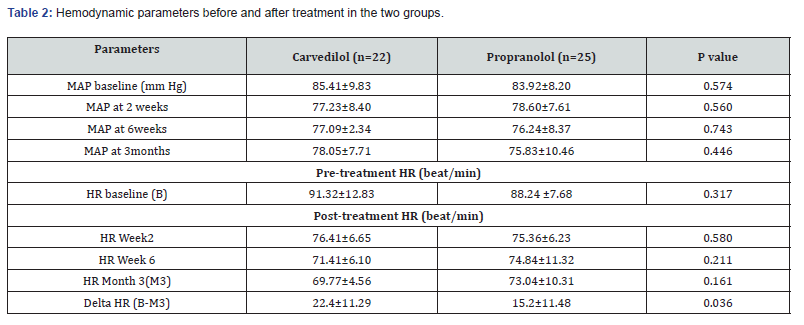
The MAP and HR in the two study groups were not significant at baseline and subsequently at 2 weeks and 6 weeks (Table 2).
The maximum dose used for carvedilol was 12.5mg/day and it was 60mg/day for propranolol to achieve a decrease of heart rate of by 25% from the baseline or heart rate of 60/min or titrated as per tolerability of the patients and lab parameters The median dose of propranolol was 40mg/day (40-60mg) and that of carvedilol was 6.25mg/day (6.25-12.5mg).
The mean decrease in MAP and HR at 2 weeks were higher in carvedilol than propranolol group however not significant. Similarly, the decrease in MAP at 3 months was comparable in both the groups. The mean decrease in HR at 3 months was significantly higher in carvedilol group than that in the propranolol group (p=0.036) Table 2.
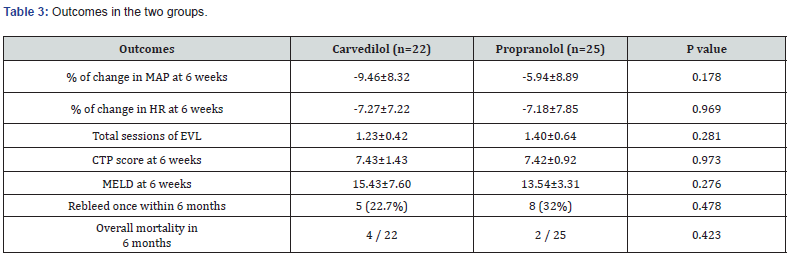
The percentage of change in MAP and HR at 6 weeks in both the groups in overall were not significant. The total frequency of EVL to eradicate the varices was higher in propanolol group than that of carvedilol group though not significant (1.4 vs 1.2). The rebleeding at least once within 6 months was also higher in propranolol group than carvedilol group (32 vs 22.7%). The overall mortality in 6 months in carvedilol group was 18% which was higher than that in propranolol group (8%) But on further analysis, it was found that the deaths were not due to complications of re-bleeding and were mostly due to other complications of liver cirrhosis (Table 3).
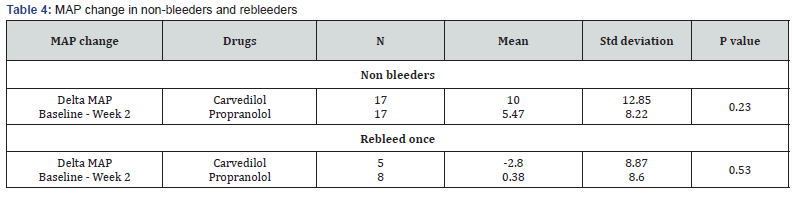
The mean change in MAP in non-bleeders was higher in carvedilol than propranolol (10 vs 5.47 %) at 2 weeks. Similarly, the change in MAP in rebleeder was low in both the two groups.
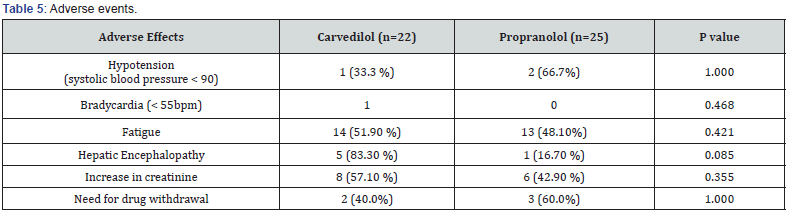
Both the drugs were not free from side effects. Patients treated with Propranolol and carvedilol had hypotension though only one patient had bradycardia in carvedilol group. Fatigue, hepatic encephalopathy, and increased creatinine were higher in carvedilol group than propranolol group though not significant. (Table 4). The need for drug withdrawal was also comparable between the two groups (Table 5).
Discussion
Although both the drugs have been used for primary prophylaxis, carvedilol is less commonly used than propranolol for secondary prophylaxis of variceal bleeding. Propranolol reduces the portal pressure by lowering the portal blood flow through decreased cardiac output and decreased azygous blood flow as a result of ß-1 receptor blockade and vasoconstriction because of unopposed alpha vasoconstriction effect which leads to arteriolar splanchnic vasoconstriction (beta 2 blockade) but it is not always enough for preventing rebleeding [7]. The inability of propanolol to prevent rebleeding may be attributed to the fact that it has no action that decreases the intrahepatic resistance, which is raised in cirrhosis of liver. However, carvedilol decreases the intrahepatic resistance and thus has a greater portal hypotensive effect than propranolol5. It can have more reduction in MAP and be more potent than propranolol. The use of carvedilol for primary prophylaxis was found to achieve a hemodynamic response with improved outcome in terms of prevention of variceal bleeding, hepatic decompensation, and mortality in 56% of propranolol non-responders [12]. Moreover, it is rapidly absorbed orally with absolute bioavailability of around 25 %. It has a rapid onset of action of 1–2 hours and an elimination half-life of 6–10 hours. It is excreted mainly through bile and does not require dose adjustment in renal failure [13]. Carvedilol which decreases significant portal pressure and intrahepatic resistance suggests a greater therapeutic potential though it is less commonly used for secondary prophylaxis. Therefore, based on this benefit of carvedilol which was used for secondary prophylaxis of variceal bleeding in our study, has shown an effective comparable benefit using carvedilol though it is not superior to propranolol.
In our study, carvedilol or propranolol decreased HR and MAP at 6 weeks and 3 months that is similar to the results of the study done by Gupta V et al [7]. The mean decrease in HR in carvedilol group was higher than that in propranolol group (22 + 11 vs 15 + 11) with significant p value 0.034 and this was higher as compared to other studies [14,15]. The mean reduction of MAP in the non bleeders was higher than that of re-bleeders. Among the nonbleeders the mean decrease in MAP at 2 weeks higher in carvedilol than propranolol group (10 vs 5.47%).
Fatigue and hepatic encephalopathy were the common side effects associated with use of both the drugs. There was 10 percent lower rate of rebleed in patients with carvedilol group as compared to propranolol group though not significant. Rebleeding within 6 months was more in propranolol than in carvedilol group (32 vs 22.7%). This is comparable to the rebleeding rate i.e. 61% (37 out of 61) in carvedilol after a median follow up of 30 months done by Lo GH et al. [16]. Another study done by Faust Feu et al, 25 out of 69 patients (36%) treated with propranolol had rebleeding at least once during follow up period of 28 months [17]. The need for transient withdrawal of drug for few days was comparable between the two groups.
The overall mortality was higher in carvedilol as compared to propranolol group though not significant. This was attributed to other complications of cirrhosis but not due to rebleeding or side effects of carvedilol. Our study has few limitations. The change in HVPG which could have added the beneficial role in comparison of efficacy of both the drugs, could not be done because of unavailability of this facility at our center. The decrease in the MAP and HR in both the groups may not be translated into the significant clinical outcomes of decreased rebleeding. Moreover, active alcoholism in the two groups were not considered into account.
Conclusion
Our study shows that carvedilol was equally efficacious if not superior to the propranolol in preventing the rebleed. The MAP reduction in nonbleeders was higher in carvedilol group than that in the rebleeders. This shows that future larger studies may be needed to conclude whether carvedilol is superior to propranolol or not. Nevertheless, carvedilol may be preferred over propranolol due to lower rate of rebleeding than the latter. The rate of side effects was seen more in carvedilol group than that of propranolol group without statistical significance. The side effects seen in the carvedilol group were attributed to the complications of cirrhosis itself rather than the direct effects of carvedilol.
References
- Habib A, Sanyal AJ (2007) Acute variceal hemorrhage. Gastrointestinal endoscopy clinics of North America 17(2): 223–52.
- (2018) European Association for Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. Journal of Hepatology 69(2): 406-60.
- Groszmann R J, Bosch J, Grace N D, Conn H O, Garcia-Tsao G, et al. (1990) Hemodynamic events in a prospective randomized trial of propanolol versus placebo in the prevention of a first variceal hemorrhage. Gastroenterology 99(5): 1401-1407.
- Zaman A (2003) Current Management of Esophageal Varices. Current Treatment Options in Gastroenterol 6(6): 499-507.
- Pena J, Brullet E, Sanchez-Hernandez E, Rivero M, Vergara M (2005) Variceal ligation plus nadolol compared with ligation for prophylaxis of variceal rebleeding: a multicenter trial. Hepatology 41(3): 572-578.
- Banares R, Moitinho E, Piqueras B, Casado M, Garcia-Pagan JC (1999) Carvedilol, a new nonselective beta-blocker with intrinsic anti- alpha1-adrenergic activity, has a greater portal hypotensive effect than propranolol in patients with cirrhosis. Hepatology 30(1): 79-83.
- Gupta V, Rawat R, Shalimar, Saraya A (2017) Carvedilol versus propranolol effect on hepatic venous pressure gradient at 1 month in patients with index variceal bleed: RCT. Hepatol International 11(2): 181-187.
- SarinS K, Kumar A, Angus P W, Sanjay Saran Baijal, Soon Koo Baik, et al. (2011) Diagnosis and management of acute variceal bleeding: Asian Pacific Association for Study of the Liver recommendations. Hepatol Int 5(2): 607-624.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey WD (2007) Practice Guidelines Committee of the American Association for the Study of Liver Diseases. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 46(3): 922-938.
- Villanueva C, Colomo A, Aracil C, Guarner C (2008) Current endoscopic therapy of variceal bleeding. Best Practice & Research Clinical Gastroenterology 22(2): 261-278.
- Antil N, Sureka B, Mittal M K, Malik A, Gupta B, Thukral B B (2016) Hepatic Venous Waveform, Splenoportal and Damping Index in Liver Cirrhosis: Correlation with Child Pugh’s Score and Oesophageal Varices. Journal of Clinical and Diagnostic Research 10(2): TC01-05.
- Reiberger T, Ulbrich G, Ferlitsch A, Payer B A, Trauner M, et al. (2013) Carvedilol for primary prophylaxis of variceal bleeding in cirrhotic patients with hemodynamic non-response to propranolol. Gut 62(11): 1634-1641.
- Ruffolo R R Jr, Gellai M, Hieble J P, Willette R N, Nichols A J (1990) The pharmacology of carvedilol. Eur J Clin Pharmacol 38(2): S82–88.
- Hobolth L, Møller S, Grønbæk H, Roelsgaard K, Bendtsen F (2012) Carvedilol or propranolol in portal hypertension? A randomized comparison. Scandinavian Journal of Gastroenterology 47(4): 467-474.
- Banares R, Moitinho E, Matilla A, Garcia-Pagan J C, Lampreave J L (2002) Randomized comparison of long-term carvedilol and propranolol administration in the treatment of portal hypertension in cirrhosis. Hepatology 36:1367-1373.
- Lo G H, Chen W C, Wang H M, Yu H C (2012) A randomized, controlled trial of carvedilol vs. nadolol plus isosorbide mononitrate for the prevention of variceal rebleeding. Journal of Gastroenterology and Hepatology 27(11): 1681-1687.
- Feu F, Garcia Pagan J C, Bosch J, Luca A, Escorsell A et al. (2005) Relation between portal pressure response to pharmacotherapy and risk of recurrent variceal hemorrhage in patients with cirrhosis. The Lancet 346(8982): 1056-1059.






























