Ensuring Adequate Essential Fatty Acid Status in Vegetarians and Vegans
Gilles RG Monif*
Infectious Diseases Incorporated, Georgia
Submission:January 23, 2020; Published: February 21, 2020
*Corresponding author:Gilles RG Monif, Infectious Diseases Incorporated, is 17121 Lakewood Drive Bellevue Nebraska 68123, Georgia
How to cite this article:Gilles RG Monif. Ensuring Adequate Essential Fatty Acid Status in Vegetarians and Vegans. Adv Res Gastroentero Hepatol, 2020;14(5): 5558967. DOI: 10.19080/ARGH.2020.14.5558967.
Abstract
Omega-3 and omega-6 fatty acids are essential in the human diet, in that they cannot be synthesized physiologically. The Omega-3 fatty acid, DHA, is highly concentrated in the brain and is important for brain function. Omega-6 fatty acids are also important. They lower harmful LDL cholesterol, boost HDL, and help keep blood sugar in check by improving the body’s sensitivity to insulin. The latest evidence shows that both omega 3 and omega 6 fatty acids are healthy. Therefore omega 6 fatty acids intake does not need to be reduced. However, an increase in Omega 3 fatty acids (ALA) consumption may be necessary in some patients.
Omega-3 fatty acids are present in some plant foods as alpha-linolenic acid (ALA), which can be converted by the body into DHA. Omega-6 fatty acids are found in many plant foods in the form of linolenic acid (LA). Evidence suggests that ALA-derived DHA is sufficient to maintain brain DHA levels and preserve function. There is no evidence of adverse effects on health or cognitive function with lower DHA ingestion levels in vegans. While fish oils provide a source of EPA and DHA which don’t require conversion, the most recent science doesn’t confirm the benefits of fish oil supplements for the prevention and treatment of coronary artery disease. A good supply of ALA is essential for a healthy plant-based diet. This can easily be obtained from plant foods. Patients should warned about the unsubstantiated cardiovascular health claims of fish oil products
Keywords:ALA; DHA; Essential fatty acids; Fish oil; LA; Omega-3; Omega-6; Plant-based; Vegan; Vegetarian
Abbreviations: PUFAs: Polyunsaturated Essential Fatty Acids; Omega-3s: Omega-3 Fatty Acids; ALA: Alpha-Linolenic Acid; EPA: Eicosapentaenoic Acid; DHA: Docosahexaenoic Acid; AHA: American Heart Association; CHD: Coronary Heart Disease; EAR: Estimated Average Requirements; AI: Adequate Intake; RDA: Recommended Dietary Allowance
Introduction
The two major classes of polyunsaturated essential fatty acids (PUFAs) are the omega-3 and omega-6 fatty acids. Like all fatty acids, PUFAs consist of long chains of carbon atoms with a carboxyl group at one end of the chain and a methyl group at the other. PUFAs are distinguished from saturated and monounsaturated fatty acids by the presence of two or more double bonds between carbons within the fatty acid chain [1-3].
Both omega-3 and omega-6 fatty acids are essential in that they cannot be synthesized physiologically. Omega-3 fatty acids (omega-3s) have a carbon–carbon double bond located three carbons from the methyl end of the chain. Omega-3s, sometimes referred to as “n-3s,” are present in some plant foods such as soy, flaxseed oil, canola oil, and walnuts, in the form of alpha-linolenic acid (ALA). In animal foods such as oily fish, they are found in the form of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). These are not considered to be essential since they can be converted from ALA [4]. Humans can synthesize DHA from ingested ALA, although this is not an efficient process. The human conversion rate of ALA to EPA and DHA is about 5%–8% [1-3], which seems to be sufficient provided and adequate amount of ALA is ingested.
Omega-6 fatty acids have a carbon-carbon double bond located six carbons from the methyl end of the chain. Omega-6s, “n-6s,” are found in plant foods such as soy, corn, safflower and sunflower oils, nuts and seeds, in the form of linolenic acid (LA). Most humans (except those with inborn errors of metabolism) can convert LA to arachidonic acid (ARA or AA).
Benefits of Omega-3 and Omega-6 Fatty Acids
The omega-3 fatty acid, Docosahexaenoic acid (DHA), is highly concentrated in the brain and is important for brain function, in part by regulation of cell survival and neuroinflammation [5-9]. DHA is the main n-3 PUFA in the brain as it is concentrated at levels of about 10,000 nmol/g brain (10–15% of brain fatty acids or about 5g in an adult brain) [10], at least 50-fold more than EPA and 200-fold more than ALA [11-13].
Omega-6 fatty acids are also important. They lower harmful LDL cholesterol and boost protective HDL. They help keep hyperglycemia in check by improving the body’s sensitivity to insulin [14]. Some linolenic acid is converted to arachidonic acid, a building block for molecules that can promote inflammation, blood clotting, and the constriction of blood vessels. This fact led to concern that the consumption of omega-6 fatty acids should be limited. However, it turns out that very little LA is converted into ARA, even when LA is abundant in the diet, and ARA is also converted into molecules that calm inflammation and fight blood clots [15].
In a science advisory by the American Heart Association (AHA), nine independent researchers from around the country found that data from dozens of studies support the cardiovascular benefits of consuming omega-6 fatty acids [15]. This advisory was undertaken to summarize the current evidence on the consumption of omega-6 PUFAs, particularly LA, with respect to coronary heart disease (CHD) risk. Aggregate data from randomized trials, case-control and cohort studies, and long-term animal feeding experiments indicate that the consumption of at least 5% to 10% of energy from omega-6 PUFAs reduces the risk of CHD relative to lower intakes. The data also suggest that higher intakes appear to be safe and may be even more beneficial (as part of a low–saturated-fat, low-cholesterol diet). In summary, the AHA supports an omega-6 PUFA intake of at least 5% to 10% of energy in the context of other AHA lifestyle and dietary recommendations. To reduce omega-6 PUFA intakes from their current levels would be more likely to increase than to decrease risk for CHD. The AHA reviewers found that eating more omega-6 fatty acids didn’t promote inflammation. Instead, eating more omega-6 fatty acids either reduced markers of inflammation or left them unchanged. Omega-6 fatty acids also lower LDL cholesterol and are protective against heart disease. So, both omega-6 and omega-3 fatty acids are healthful [15].
Many other studies have showed that rates of heart disease went down as consumption of omega-6 fatty acids went up. A metaanalysis of six randomized trials found that replacing saturated fat with omega-6 fatty acids reduced the risk of heart attacks and other coronary events by 24%. A separate report published in the American Journal of Clinical Nutrition, that pooled the results of 11 large cohorts, showed that replacing saturated fatty acids with polyunsaturated fatty acids (including omega-6 and omega-3 fatty acids) reduced heart disease rates more than did replacing them with monounsaturated fatty acids or carbohydrates [16].
While there is a theory that omega-3 fatty acids are better for our health than omega-6 fatty acids, this is not supported by the latest evidence. Some people have incorrectly thought that the ratio of n-3 to n-6 fatty acids is important. However, the omega-3 to omega-6 ratio is basically the “good divided by the good,” so it is of no value in evaluating diet quality or predicting disease [17]. In the Health Professionals Follow-up Study, for example, the ratio of omega-6 to omega-3 fatty acids wasn’t linked with risk of heart disease because both of these were beneficial [18]. Rather than cutting down on beneficial omega 6, the patient would be better served by simply increasing their intake of ALA (omega 3).
Nutritional Requirements
Since the National Academy of Sciences concluded that there is inadequate information to set Estimated Average Requirements (EAR) or the Recommended Dietary Allowance (RDA) for either LA or ALA for healthy individuals, the Adequate Intake (AI) is used. The present essential fatty acid AI is based on “the highest median intake of LA and ALA in United States adults, where a deficiency is basically nonexistent in non-institutionalized populations” [19] (Table 1 & 2).
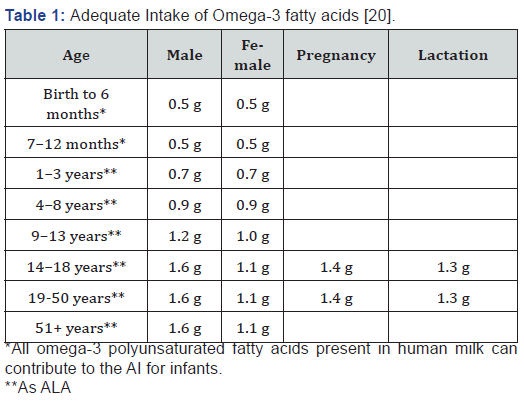
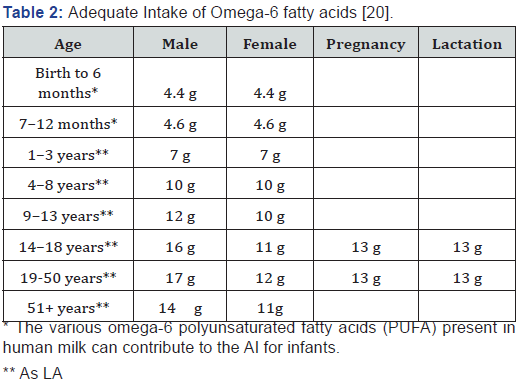
However, it is unknown if the AIs are beneficial or physiologically adequate because dose-response data studies are lacking, Essential fatty acid status is not usually clinically tested, and absence of deficiency symptoms is not necessarily evidence of adequacy. The rate of DHA uptake into the brain is assumed to be replacing DHA that is metabolized in the brain, and therefore, can be used as an estimate for the brain DHA requirement. It has been reported that the brain DHA uptake rate in humans is between 2.4 and 3.8 mg/day [4,21,22]. Based on current estimates of ALA consumption in adult males of 1700 mg/day, the percent conversion of ALA to DHA would need to be 0.14–0.22% to match the brain DHA requirement [22]. Therefore, it is possible that even a small amount of DHA synthesis may be sufficient to meet adult brain DHA uptake demands.
In pre-menopausal women, there is evidence that significant changes in DHA status can occur independent of changes in n-3 PUFA intake, likely through increased synthesis of DHA from ALA. For example, women have higher DHA in plasma phospholipids and erythrocytes compared with men [23], which is associated with much higher rates of DHA synthesis in women [1,2,24]. Studies of premenopausal women reported a higher capacity of ALA conversion, and a more efficient conversion of ALA to EPA and DHA compared to men [1]. In 21 days, women incorporated 700 mg of radioactive labeled [U-13C]-ALA, and resulted in a net fractional ALA interconversion of 21% of EPA, 6% of docosapentaenoic acid (can be converted to DHA), and 9% of DHA in plasma which led the researchers to postulate that increased conversion was due to either an estrogen catalyzed conversion or an increased need for EPA and DHA during pregnancy and fetal development [1].
One study did not find any associations between dietary EPA, DHA, or the n–6 PUFA and birth weight. In contrast, the results indicate a growth-promoting effect of ALA intake, with the increase in birth weight being independent of gestational age at birth. It is noteworthy that no specific function has been assigned to ALA itself other than serving as a source of energy or conversion to EPA and DHA. Therefore, any mechanisms of improvement in birth weight are most likely via desaturation and elongation to its longer-chain derivatives. Although conversion rates of ALA into the longer-chain EPA and DHA are modest with the estimated fractional conversion reported to be less than 5% [3], increased ALA intake has demonstrated to increase proportions of longchain n–3 fatty acids in plasma and cell lipids to reproduce beneficial effects [25]. Specifically, in pregnancy, the levels of DHA and ARA increase in cord blood in relation to circulating levels of ALA and LA in maternal blood [26].
Fish Oil Supplements
Sales of fish oil supplements reached $1.84 billion in 2018 indicating widespread use. However, the most recent science doesn’t confirm the benefits of fish oil supplements for the prevention and treatment of coronary artery disease. The initial reasoning for recommending fish oil supplements was based on studies of the Eskimo. It was mistakenly thought that the Eskimo suffered less from atherosclerosis and from coronary artery disease in particular. However, it is now known that the Eskimo do not have lower rates of coronary artery disease. One study concluded that the “Greenland Eskimos and the Canadian and Alaskan Inuit have CAD as often as the non-Eskimo populations [27].” Another study showed “Eskimos have CHD despite high consumption of omega-3 fatty acids [28].” A meta study of the efficacy of fish oil summarizes their results as follows: “All of the studies included were the gold-standard kind of clinical trial -- with people assigned at random to either take fish oil or a placebo. The studies ranged in length from one to nearly five years. The authors detected no reduction in any cardiovascular events, such as heart attacks, sudden death, angina, heart failures, strokes, or death, no matter what dose of fish oil used [29].”
EFA Status in Vegans
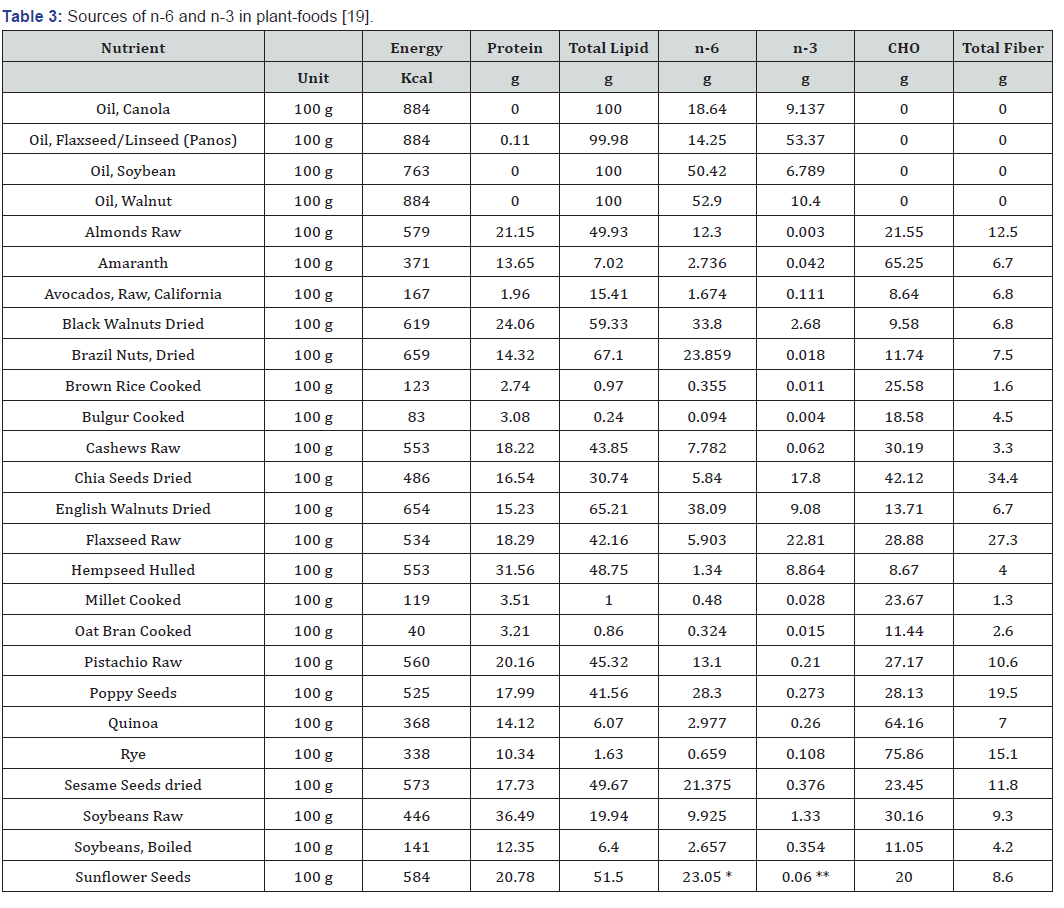
The most plentiful dietary n-6 polyunsaturated essential fatty acid is LA. Omega-6 fatty acid food sources commonly consumed by vegans include nuts, seeds, certain vegetables, and vegetables oils such as soybean oil, safflower oil, and corn oil among others. Therefore, any diet that is plant-based leads to a high dietary intake of LA [19]. Ensuring adequate essential fatty acids in vegans therefore focuses on obtaining an adequate intake of the omega 3 fatty acid, ALA. There is evidence that DHA synthesis from ALA can be sufficient to maintain brain function. For example, vegetarians and vegans, in which DHA derived from ALA is the sole source of DHA, have DHA levels comparable to omnivores [30]. Some studies show that their DHA levels are lower than omnivores [31-33] but have neurological disease rates comparable to omnivores [34-37], suggesting that ALA-derived DHA is sufficient to maintain brain function in these individuals. In addition, dietary ALA, with no DHA, is sufficient to completely restore brain DHA in rats [38] and non-human primates [39]. Taken together, evidence suggests that ALA-derived DHA is sufficient to maintain brain DHA levels and preserve function [40]. There is no evidence of adverse effects on health or cognitive function with lower DHA ingestion levels in vegans [31].
One study showed that vegetarians give birth to infants with less DHA in their plasma and cord artery phospholipids but this did not appear to be independently related to the outcome of pregnancy [41].
Clinical Considerations
(Table 3) Generally, if a patient’s food history doesn’t include good sources of ALA then foods that are good sources of ALA should be prescribed. If the patient isn’t compliant, then supplements can be prescribed. While the conversion of ALA to DHA rates in women are higher, if the intake of rich sources of ALA are not being consumed then supplements should be prescribed. Infant formula is available enriched with DHA. Plant-based sources of omega- 3s from algal oil usually provide around 100–300 mg DHA and some contain EPA as well. These supplements typically contain omega-3s in the triglyceride form [42]. According to a small study, the bioavailability of DHA from algal oil is equivalent to that from cooked salmon [43]. In one study vegans responded robustly to a relatively low dose of a vegan DHA and EPA supplement [30].
Discussion
A good supply of ALA is essential for a healthy plant-based diet. This can easily be obtained from plant foods. Patients should warned about the unsubstantiated cardiovascular health claims of fish oil products.
References
- Burdge GC, Wootton SA (2002) Conversion of alpha-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women. Br J Nutr 88(4): 411-420.
- Burdge GC, Jones AE, Wootton SA (2002) Eicosapentaenoic and docosapentaenoic acids are the principal products of alpha-linolenic acid metabolism in young men. Br J Nutr 88(4): 355-363.
- Brenna JT (2002) Efficiency of conversion of alpha-linolenic acid to long chain n-3 fatty acids in man. Curr Opin Clin Nutr Metab Care 5(2): 127-132.
- Umhau JC, Zhou W, Carson RE, Rapoport SI, Polozova A, et al. (2009) Imaging incorporation of circulating docosahexaenoic acid into the human brain using positron emission tomography. J Lipid Res 50(7): 1259-1268.
- Orr SK, Palumbo S, Bosetti F, Mount HT, Kan JX, et al. (2013) Unesterified docosahexaenoic acid is protective in neuroinflammation. J Neurochem 127(3): 378-393.
- Bazan NG, Molina MF, Gordon WC (2011) Docosahexaenoic acid signalolipidomics in nutrition: significance in aging, neuroinflammation, macular degeneration, Alzheimer's, and other neurodegenerative diseases. Annu Rev Nutr 31: 321-351.
- Desai A, Kevala K, Kim HY (2014) Depletion of brain docosahexaenoic acid impairs recovery from traumatic brain injury. PLoS One 9(1): e86472.
- Lukiw WJ, Cui JG, Marcheselli VL, Bodker M, Botkjaer A, et al. (2005) A role for docosahexaenoic acid-derived neuroprotectin D1 in neural cell survival and Alzheimer disease. J Clin Invest 115(10): 2774-2783.
- Akbar M, Calderon F, Wen Z, Kim HY (2005) Docosahexaenoic acid: a positive modulator of Akt signaling in neuronal survival. Proc Natl Acad Sci U S A 102(31): 10858-10863.
- Martinez M (1992) Abnormal profiles of polyunsaturated fatty acids in the brain, liver, kidney and retina of patients with peroxisomal disorders. Brain Res 583(1-2): 171-182.
- Igarashi M, Ma K, Gao F, Kim H, Greenstein D, et al. (2009) Brain lipid concentrations in bipolar disorder. J Psychiatr Res 44(3): 177-182.
- Chen CT, Domenichiello AF, Trépanier MO, Liu Z, Masoodi M, et al. (2013) The low levels of eicosapentaenoic acid in rat brain phospholipids are maintained via multiple redundant mechanisms. J Lipid Res 54(9): 2410-2422.
- Brenna JT, Salem NJ, Sinclair AJ, Cunnane SC (2009) alpha-Linolenic acid supplementation and conversion to n-3 long-chain polyunsaturated fatty acids in humans. Prostaglandins Leukot Essent Fatty Acids 80(2-3): 85-91.
- Strombom A, Rose S (2017) The prevention and treatment of Type II Diabetes Mellitus with a plant-based diet. Endocrin Metab Int J 5(5): 00138.
- Harris WS, Mozaffarian D, Rimm E, Kris-Etherton P, Rudel L, et al. (2009) Omega-6 fatty acids and risk for cardiovascular disease: a science advisory from the American Heart Association Nutrition Subcommittee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Cardiovascular Nursing; and Council on Epidem. Circulation 119(6): 902-907.
- https://www.health.harvard.edu/newsletter_article/no-need-to-avoid-healthy-omega-6-fats
- https://www.hsph.harvard.edu/nutritionsource/2007/06/19/ask-the-expert-omega-3-fatty-acids/
- Mozaffarian D, Ascherio A, Hu FB, Stampfer M, Willett W, et al. (2005) Interplay between different polyunsaturated fatty acids and risk of coronary heart disease in men. Circulation 111(2): 157-164.
- Burns-Whitmore B, Froyen E, Heskey C, Parker T, Pablo GS (2019) Alpha-Linolenic and Linoleic Fatty Acids in the Vegan Diet: Do They Require Dietary Reference Intake/Adequate Intake Special Consideration? Nutrients 11(10): 2365.
- Institute of Medicine (IOM) (2005) Dietary fats: Total fat and fatty acids. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. National Academics Press, Washington, DC, USA.
- Umhau JC, Zhou W, Thada S, Demar J, Hussein N, et al. (2013) Brain Docosahexaenoic Acid [DHA] Incorporation and Blood Flow Are Increased in Chronic Alcoholics: A Positron Emission Tomography Study Corrected for Cerebral Atrophy. PLoS ONE 8(10): e75333.
- Barceló-Coblijna G, Murphy EJ (2009) Alpha-linolenic acid and its conversion to longer chain n-3 fatty acids: benefits for human health and a role in maintaining tissue n-3 fatty acid levels. Prog Lipid Res 48(6): 355-374.
- Lohner S, Fekete K, Marosvölgyi T, Decsi T (2013) Gender differences in the long-chain polyunsaturated fatty acid status: systematic review of 51 publications. Ann Nutr Metab 62(2): 98-112.
- Pawlosky R, Hibbeln J, Lin Y, Salem N (2003) n-3 fatty acid metabolism in women. Br J Nutr 90(5): 993-994.
- Finnegan Y, Minihane A, Leigh-Firbank E, Kew S, Meijer G, et al. (2003) Plant- and marine-derived n-3 polyunsaturated fatty acids have differential effects on fasting and postprandial blood lipid concentrations and on the susceptibility of LDL to oxidative modification in moderately hyperlipidemic subjects. Am J Clin Nutr 77(4): 783-795.
- Bobiński R, Mikulska M (2015) The ins and outs of maternal-fetal fatty acid metabolism. Acta Biochim Pol 62(3): 499-507.
- Fodor JG, Helis E, Yazdekhasti N, Vohnout B (2014) "Fishing" for the origins of the "Eskimos and heart disease" story: facts or wishful thinking? Can J Cardiol 30(8): 864-868.
- Ebbesson SOE, Risica PM, Ebbesson LOE, Kennish JM (2005) Eskimos have CHD despite high consumption of omega-3 fatty acids: the Alaska Siberia project. Int J Circumpolar Health 64(4): 387-395.
- Kwak S, Myung S, Lee Y, Seo H, Group KMaS (2012) Efficacy of omega-3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular disease: a meta-analysis of randomized, double-blind, placebo-controlled trials. Arch Intern Med 172(9): 686-694.
- Sarter B, Kelsey KS, Schwartz TA, Harris WS (2015) Blood docosahexaenoic acid and eicosapentaenoic acid in vegans: Associations with age and gender and effects of an algal-derived omega-3 fatty acid supplement. Clin Nutr 34(2): 212-218.
- Welch AA, Shakya-Shrestha S, Lentjes MA, Wareham NJ, Khaw KT (2010) Dietary intake and status of n-3 polyunsaturated fatty acids in a population of fish-eating and non-fish-eating meat-eaters, vegetarians, and vegans and the product-precursor ratio [corrected] of α-linolenic acid to long-chain n-3 polyunsaturated fatty ac. Am J Clin Nutr 92(5): 1040-1051.
- Rosell MS, Lloyd-Wright Z, Appleby PN, Sanders TA, Allen NE, et al. (2005) Long-chain n-3 polyunsaturated fatty acids in plasma in British meat-eating, vegetarian, and vegan men. Am J Clin Nutr 82(2): 327-334.
- Mann N, Pirotta Y, O'Connell S, Li D, Kelly F, et al. (2006) Fatty acid composition of habitual omnivore and vegetarian diets. Lipids 41(7): 637-646.
- Giem P, Beeson W, Fraser G (1993) The incidence of dementia and intake of animal products: preliminary findings from the Adventist Health Study. Neuroepidemiology 12(1): 28-36.
- McCarty MF (2001) Does a vegan diet reduce risk for Parkinson's disease? Med Hypothese 57(3): 318-323.
- Orlich MJ, Singh PN, Sabaté J, Jaceldo-Siegl K, Fan J, et al. (2013) Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med 173(13): 1230-1238.
- Beezhold BL, Johnston CS, Daigle DR (2010) Vegetarian diets are associated with healthy mood states: a cross-sectional study in seventh day adventist adults. Nutr J 9: 26.
- André A, Juanéda P, Sébédio JL, Chardigny JM (2005) Effects of aging and dietary n-3 fatty acids on rat brain phospholipids: focus on plasmalogens. Lipids 40(8): 799-806.
- Anderson GJ, Neuringer M, Lin DS, Connor WE (2005) Can prenatal N-3 fatty acid deficiency be completely reversed after birth? Effects on retinal and brain biochemistry and visual function in rhesus monkeys. Pediatr Res 58(5): 865-872.
- Domenichiello AF, Kitson AP, Bazinet RP (2015) Is docosahexaenoic acid synthesis from α-linolenic acid sufficient to supply the adult brain? Progress in Lipid Research 59: 54-66.
- Reddy S, Sanders T, Obeid O (1994) The influence of maternal vegetarian diet on essential fatty acid status of the newborn. Eur J Clin Nutr 48(5): 358-368.
- Product review: fish oil and omega-3 fatty acid supplements review (including krill, algae, calamari, green-lipped mussel oil).
- Arterburn LM, Oken HA, Hall EB, Hamersley J, Kuratko CN, et al. (2008) Algal-oil capsules and cooked salmon: nutritionally equivalent sources of docosahexaenoic acid. J Am Diet Assoc 108(7): 1204-1209.