Ayurveda Aetiology, Pathogenesis & Holistic Management of Inflammatory Bowel Disease
Nishant Shukla*
Head of Kayachikitsa (Ayurved medicine), Gujarat Ayurved University, India
Submission: August 09, 2018; Published: September 17, 2018
*Corresponding author: Nishant Shukla, Professor & Head of Kayachikitsa (Ayurved medicine), Shri V. M. Mehta Ayurveda College, Anandpar Rajkot, Ex. Head of Kayachikitsa Gulabkunverba Ayurved Mahavidyalaya, Anil 3 Patel Colony, Jamnagar, India, Tel: +91-9426984260; Email: nishantvd@rediffmail.com
How to cite this article: Nishant Shukla. Ayurveda Aetiology, Pathogenesis & Holistic Management of Inflammatory Bowel Disease. Adv Res Gastroentero Hepatol. 2018; 10(4): 555794. DOI: 10.19080/ARGH.2018.10.555794.
Keywords: Inflammation; Colon; Large intestine; Abdominal pain; Diarrhoeal disease
Abbrevations:MRCP: Magnetic Resonance Cholangiopancreatography; ERCP: Endoscopic Retrograde Cholangiopancreatography; DIA: Digital Image Technique; EUS: Endoscopic Ultrasonography; SOC: Single Operator Cholangioscopy; CT: Cross Section Imaging
Introduction
HBiliary strictures are traditionally classified as ‘indeterminate’ when basic work up, including transabdominal imaging and endoscopic retrograde cholangiopancreatography (ERCP) with conventional brush cytology, is non-diagnostic for its etiology.
Etiology of Biliary Strictures

Evaluation of Patients with Biliary Strictures
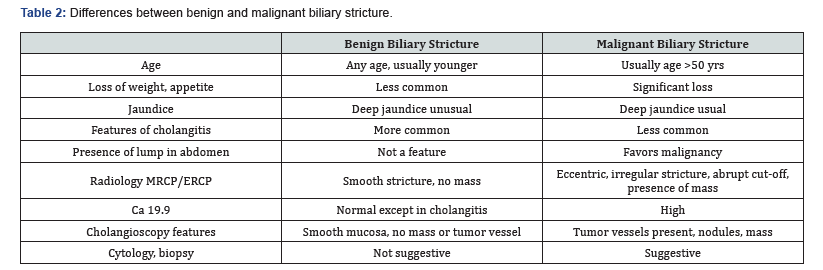
The clinical approach to the patient with indeterminate biliary stricture includes a thorough history and physical examination. By and large, strictures of the bile duct in patients with obstructive jaundice should be considered malignant unless a benign etiology is ascertained. The significance of biliary strictures without jaundice is less certain.
Biomarkers
The most common biomarkers for suspected biliary tract malignancies in clinical use are serum CA 19-9 and carcinoembryonic antigen. In patients with PSC, using cut-off value of 129U/ml, the sensitivity and specificity of CA 19-9 for the diagnosis of cholangiocarcinoma are 79% and 98% respectively [2]. In patients without PSC, the sensitivity is only 53% with a cutoff value 100 U/ml [3]. Elevated serum carcinoembryonic adenocarcinoma has also been shown to have a sensitivity of 33- 68% and specificity of 79-95% for cholangiocarcinoma.
Radiological Work-Up
Ultrasound is helpful in patients with biliary stricture by demonstrating intrahepatic biliary radical dilatation and the level of obstruction. However, the distal part of the common bile duct is not properly evaluated because of the interference of bowel gas. Moreover, it has a very low yield for actual detection of strictures on biliary ductal masses [4]. The development of multi- detector helical scanners, used in conjunction with rapid injection of contrast media, accurate depiction of extension of the tumor, locoregional lymphadenopathy and encasement of blood vessels to determine operability of the tumor can be picked up easily.
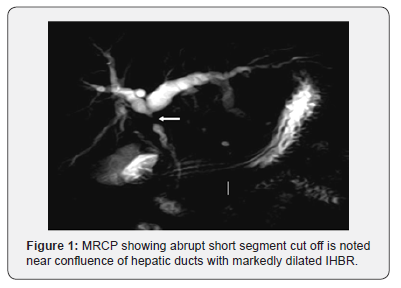
Magnetic resonance cholangiopancreatography (MRCP) has a high sensitivity for bile duct lesions and has got comparable diagnostic accuracy in comparison to ERCP. Ductal features at MRCP which may suggest malignancy include long (>10mm), asymmetrical and irregular strictures. The presence of mass lesion is highly suggestive of malignancy, especially in the hilar region. Abrupt cut-off of the CBD in contrast to a smooth tapering has traditionally been considered to be a sign of malignancy (Figure 1). The sensitivity and specificity of MRCP to differentiate malignant from benign strictures are reported to be 38%-90% and 70%-85% respectively [5]. MRCP is 88-96% accurate in predicting the extent of involvement of the bile duct in cholangiocarcinoma.
Role of Endoscopy
Endoscopic retrograde cholangipancreatography
ERCP remains the first line approach for tissue sampling of biliary strictures. The reported sensitivity of conventional brush cytology is 25% to 55% [6]. Different techniques have been employed to improve the sensitivity of conventional brush cytology including novel brushes, biliary stricture dilation with subsequent brushings and repeated brushings. The pluricellular nature and submucosal pattern of tumor growth in cholangicarcinoma or extrinsic malignancy involving the bile ducts attributes to the low sensitivity of biliary brushings. Inadequate biliary cytology specimens are one of the main reasons for non-diagnostic samples. This may be overcome by the presence of an onsite cytopathologist. Several other strategies include cutting the entire brush, creation of slides by the endoscopy team and placing them in a fixative solution prior to submission to pathology are being used to overcome inadequate sampling. The fluorescence in situ hybridization analysis detects chromosomal polysomy using fluorescent probes, whereas the Digital Image Technique (DIA) quantifies nuclear DNA with special stains to assess the presence of aneuploidy.
In patients with PSC these chromosomal abnormalities can be seen without the presence of malignancy. Thus, the specificity of FISH in this setting is lower than routine cytology. Thus, FISH increases the sensitivity of brush cytology of indeterminate biliary strictures without much improvement in the specificity. FISH should be reserved for patients with high pre-test probability for malignant strictures. Using endobiliary forceps, the malignancy detection rates ranges from 44% to 89% for cholangiocarcinoma and 33% to 71% for pancreatic cancer [7]. Triple sampling with brushing, transpapilary biopsy and endoluminal FNA has shown the highest sensitivity. Risk of biliary ductal perforation after endobiliary biopsy, however, remains a concern.
Endoscopic ultrasound
Endoscopic ultrasonography (EUS) has emerged as an important method for evaluating indeterminate biliary stricture. It provides an excellent alternative method for visualizing and sampling the extra-hepatic biliary tree, hilar masses, gallbladder and peri-hilar lymph nodes and vessels. Sensitivity is significantly better in distal compared to proximally located tumors.
Cholangiscopy

The technique has recently gained attention with the development of a single operator cholangioscopy (SOC) system known as the SpyGlass (Boston Scientific, Natick, MA, USA). Visually directed biopsies can be obtained using biopsy forceps (SpyBite). Overall sensitivity and specificity of SOC examination for differentiating malignant and benign ductal abnormalities have been seen to be 78% and 82% respectively, higher than the 51% and 54% of ERCP alone [8]. Among the cholangiscopic features, the presence of abnormal tumor vessels due to neovascularization within the biliary stricture is suggestive of biliary malignancy. Intraductal nodules and masses can be visualized during cholangiscopy and are indicative of malignancy (Figure 2). Using these features, good concordance has been seen between cholangioscopic appearance and histopathology.
Intraductal ultrasound
ERCP with IDUS improves the diagnostic yield of biliary strictures. A small and high-frequency ultrasound probe provides high resolution images of ductal and periductal tissues. IDUS features which suggest malignancy include eccentric wall thickening with an irregular surface, a hypoechoic mass, heterogenicity of the internal echo pattern, a papillary surface, disruption of the normal three-layer sonographic structure of the bile duct, presence of lymph nodes, and vascular invasion. It is, however, not commonly available and expertise is needed for a successful outcome.
Chromoendoscopy, autofluorescence and narrowband imaging
For better characterization of biliary strictures, several techniques have been employed during cholangioscopy. In chromoendoscopy, different stains are topically applied to the surface of the mucosa. Methylene blue can successfully differentiate malignant lesions and ischemic strictures from normal mucosa. Biliary narrow band imaging enhances the vascular pattern of the mucosal surface and delineates tumor extent effectively. Initial cholangioscopic studies with autofluorescence have been less promising; poor specificity and high rates of false positivity were observed [9].
Confocal laser endomicroscopy (The cellvizio system)
Cellvizio is a probe-based CLE system which generates optical biopsies, providing physicians with microscoping images of tissue instantaneously and in a minimally invasive manner. This technique produces specific patterns that correlate with standard histology and differentiate between malignancy, inflammation and normal mucosa. In a recent multicentre study CLE was found to provide significantly higher diagnostic accuracy for malignant biliary strictures than standard ERCP (90% vs 73%) [10].
The Miami classification system has been proposed to characterize pCLE findings for biliary strictures. The presence of thick white bands (>20 micrometer), thick dark bands (>40 micrometer), dark clumps, epithelial structures and contrast leakage were the factors which could differentiate malignant from benign strictures [11]. Another newer classification system called the Paris classification was recently described. This includes additional features such as vascular congestion, dark glandular patterns, increased interglandular space and thickened reticular structures [12].
Suggested Approach to Indeterminate Biliary Strictures (Figure 3)
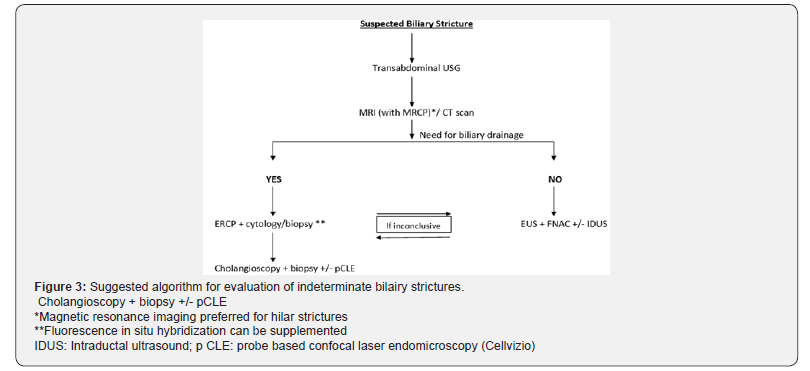
The choice of diagnostic workup should be individualized, depending to a great extent on local expertise and availability of the particular technology. Cross section imaging (CT or MRI) is useful to assess the respectability in patients with suspected malignancy. Table 2 outlines differences between benign and malignant strictures.
References
- Clatton RA, Clarke DL, Currie EJ, KK Madhavan, RW Parks, et al. (2003) Incidence of benign pathology in patients undergoing hepatic resection for suspected malignancy. Surgeon 1(1): 32-38.
- Levy C, Lymp J, Angulo P, Gores GJ, Larusso N, et al. (2005) The value of serum CA 19-9 in predicting cholangiocarcinoma in patients with primary sclerosing cholangitis. Dig Dis Sci 50(9): 1734-1740.
- Patel AH, Harnois DM, Klee GG, La Russo NF, Gores GJ et al. (2000) Utility of CA 19-9 in the diagnosis of Cholangiocarcinoma in patients without primary sclerosing cholangitis. Am J Gastroenterol 95(1): 204- 207.
- Sainani NI, Catalano OA, Holalkere NS, Zhu AX, Hahn PF, et al. (2008) Cholangiocarcinoma: current and novel imaging techniques. Radiographics 28: 1263-1287.
- Saluja SS, Sharma R, Pal S, Sahni P, Chattopadhyay TK (2007) Differentiation between benign and malignant hilar obstructions using laboratory and radiological investigations: a prospective study. HPB 9(5): 373-382.
- Lee JG, Leung JW, Baille J, et al. (1995) Benign dysplastic, or malignant- Making sense of endoscopic bile duct brush cytology: Results in 149 consecutive patients. Am J Gastroenterol 90(5): 722-726.
- De Bellis M, Sherman S, Fogel EL, et al. (2002) Tissue samples at ERCP in suspected malignant biliary strictures (Part 2). Gastrointest Endosc 56(5): 720-730.
- Chen YK, Parsi MA, Binmoeller KF, Hawes RH, Pleskow DK, et al. (2011) Single operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones. Gastrointest Endosc 74(4): 805-814.
- Itoi T, Neuhaus H, Chen YK (2009) Diagnostic value of image enhanced video cholangiopancreatoscopy. Gastrointest Endosc Clin N Am 19(4): 557-566.
- Meining A, Chen YK, Pleskow D, Stevens P, Shah RJ, et al. (2011) Direct visualization of indeterminate pancreatobiliary strictures with probebased confocal laser endomicroscopy: A multicentre experience. Gastrointest Endosc 74(5): 961-968.
- Meining A, Shah RJ, Slivka A, et al. (2012) Classification of probe based confocal laser endomicroscopy in pancreatobiliary strictures. Endoscopy 44(3): 251-257.
- Callilol F, Filoche B, Gaidhane M, Kahaleh M (2013) Refined probe based confocal laser endomicroscopy classification for biliary strictures: the Paris Classification. Dig Dis Sci 58(6): 1784-1789.






























