Arthritis as a Presenting Feature of IBD-A Study from Eastern India
Bhaswati C Acharyya1*, Mandira roy2, Souvik Guha2 and Priyankar Pal2
1Department of Paediatric Gastroenterology, Institute of Child Health, India
2Department of Paediatrics, Institute of Child Health, India
Submission: May 01, 2018; Published: May 16, 2018
*Corresponding author: > Bhaswati C Acharyya, Department of Paediatric Gastroenterology, Institute of Child Health, Kolkata, India, Email: bukuli2@hotmail.com
How to cite this article: Bhaswati C A, Mandira r, Souvik G, Priyankar P. Arthritis as a Presenting Feature of IBD-A Study from Eastern India. Adv Res Gastroentero Hepatol 2018; 9(4): 555766.DOI:10.19080/argh.2018.09.555766
Abbreviation
Abbreviation: > IBD: Inflammatory Bowel Disease; CD: Crohn's Disease; IBDU: Inflammatory Bowel Disease Unclassified; LNH: Lymphoid Nodular Hyperplasia
Introduction
Arthropathy is one of the extraintestinal manifestations of IBD. Arthritis associated with Inflammatory Bowel disease (IBD) is a subset of arthritis in the Enteropathic arthritis family. The aim of the present study is to find out the patients who presented with arthropathy as presenting feature preceeding the GI symptoms and study their clinical profile.
Materials and Methods
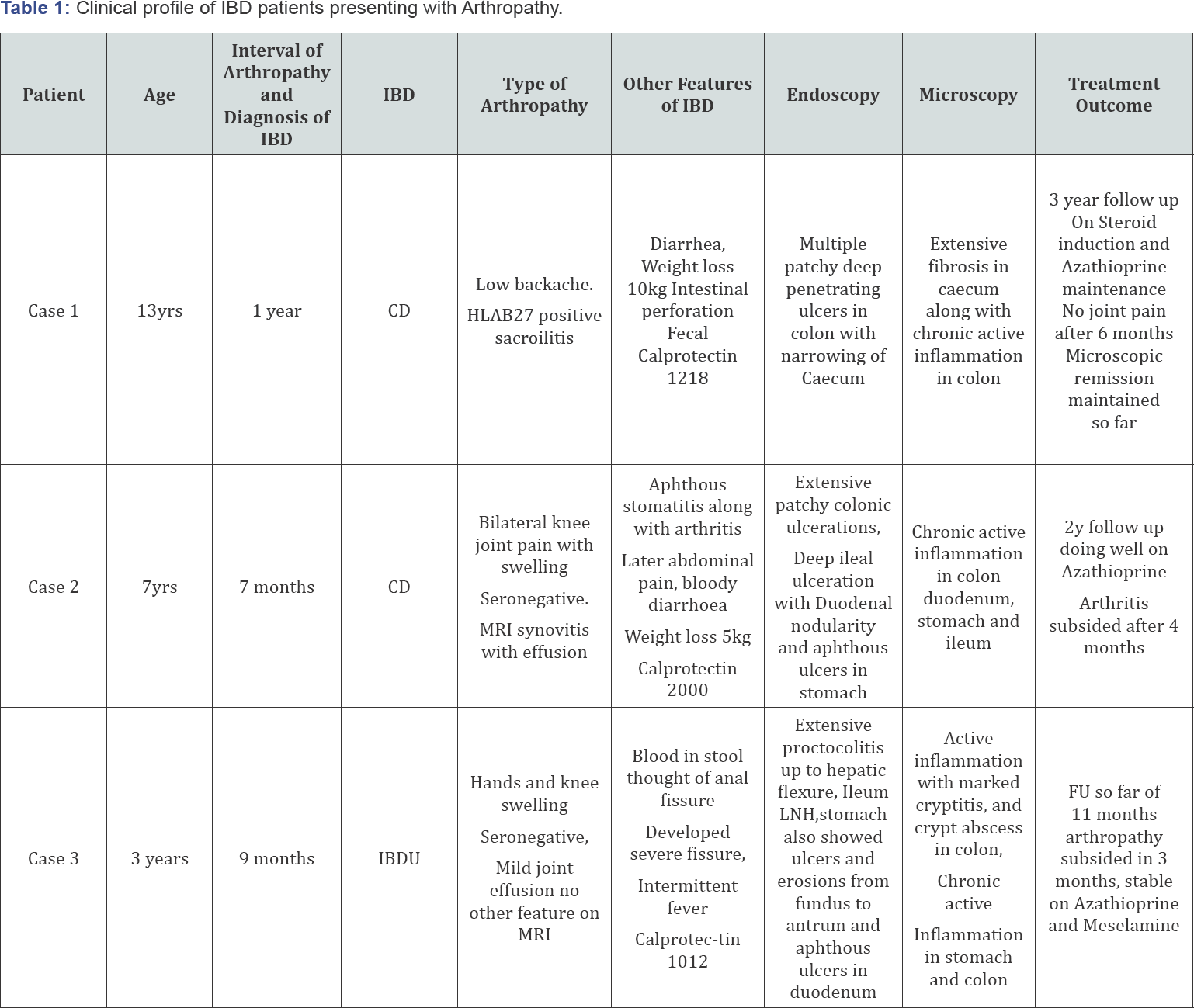
Case records of patients of IBD diagnosed between May 2010 and May 2017 in two tertiary centres of Kolkata were analysed to find out the patients presenting with Arthropathies. Case records of those patients were reviewed to find out the clinical profile of those children. Clinical data was analysed under the headings of 1) Age at presentation 2) Interval of onset of arthropathy and diagnosis of IBD, 3) Type of IBD, 4) Type of Arthropathy 5) Other features of IBD, 6) Endoscopic features of IBD 7) Microscopy of IBD and 8) treatment outcome.
Result
Total case records of 55 patients with IBD were analysed. 3 patients were found to have arthropathy as presenting feature. Clinical profiles of these patients were as follows: (Table 1) so prevalence of arthropathy as presenting features in this specified IBD populationwas 5.45%. It was associated with CD or IBD U. All arthritis preceded abdominal symptoms. All arthropathic patients had colitis (patchy or pancolitis). Only one had seropositivity of HLA B27 and rest 2 were seronegative. Average period to diagnosis from onset of arthropathy was 9.3 months. In all cases Fecal Calprotectin was markedly raised.
Discussion
Prevalence of spondylitis and peripheral arthritis is similar in UC and CD [1]. But the extra-intestinal
manifestations tend to be more frequent with colonic involvement [2]. All 3 of our cases had colonic involvement. It is of note that children with arthritis tended to have more severe IBD than those without arthritis [3]. According to some authors, CD may remain subclinical for years or even for life, and therefore the arthritis can be the only clinical expression of the disease [4]. Before onset of GI symptoms all the above 3 cases did not have relief of symptoms and cause of arthritis remained undiagnosed (except the HLAB27 positive case). Except mild relief of pain with supportive therapy they did not have any real remission.
It should be of note that Fecal Calprotectin was markedly raised in all these three patients. Calprotectin is a good noninvasive marker for gut inflammation which is still not very widely available and used tool in eastern side of the Globe. That's why we recommend monitoring of all patients with joint pain in Rheumatology clinic with fecal Calprotectin to detect gut involvement early and to decide endoscopic requirement for avoidance of delay in detecting IBD. Though this is a regular practice in the Western world, is still not a routine in the developing world.
Conclusion
It was shown that the symptoms and signs of CD in children are often subtle and nonspecific. CD should be considered in the differential diagnosis of children with arthralgia to reduce the latent period to diagnose IBD. Fecal Calprotectin can highlight the presence of bowel inflammation. It can be effectively used as an early marker to suspect IBD and to proceed for endoscopic studies.
References
- Mader R, Segol O, Adawi M, Trougoboff P, Nussinson E (2005) Arthritis or vasculitis as presenting symptoms of Crohn's disease. Rheumatol Int 25(6): 401-405.
- Greenstein AJ, Janowitz HD, Sachar DR (1976) The extraintestinal complications of Crohn's disease and ulcerative colitis: a study of 700 patients. Medicine 55(5): 401-412.
- Burbige EJ, Huang SS, Bayless TM (1975) Clinical manifestations of Crohn's disease in children and adolescents. Pediatrics 55(8): 866-871.
- Mielants H, Veys E (1984) Ileal inflammation in B27 positive reactive arthritis. Lancet 1(8371): 288.






























