Esophageal Leiomyoma as Unexpected Finding during Laparoscopic Hiatal Hernia Repair
Ivanov K1*, Ignatov V1, Shterev S1, Zlatarov A1, Tonev A1, Petrov D1, Naydenova B2 and Kolev N1
1Department of General and Operative Surgery, Medical University of Varna, Bulgaria
2Department of Anesthesiology, Medical University of Varna, Bulgaria
Submission: September 09, 2017; Published: November 16, 2017
*Corresponding author: Ivanov K, Department of General and Operative Surgery, Medical University of Varna, 55 Main Drinov Street, Bulgaria, Email: kdi@abv.bg
How to cite this article: Ivanov K, Ignatov V, Shterev S, Zlatarov A, Tonev A, et al. Esophageal Leiomyoma as Unexpected Finding during Laparoscopic Hiatal Hernia Repair. Adv Res Gastroentero Hepatol 2017; 7(4): 555718. DOI: 10.19080/ARGH.2017.07.555718
Abstract
Leiomyoma is the most common benign esophageal tumour. Although hiatal hernia is another common esophageal disease its association with leiomyoma is very rare. A case of leiomyoma in the lower third of the esophagus missed during preoperative diagnosis and revealed intraoperatively during simultaneous laparoscopic surgery for hiatal hernia and chronic calculus cholecystitis was reported.
Introduction
Leiomyoma is the most common benign esophageal tumour. Although hiatal hernia is another common esophageal disease its association with leiomyoma is very rare [1-4]. We report a case of simultaneous laparoscopic surgery for hiatal hernia and chronic calculus cholecystitis during which intramural leiomyoma has been detected in the lower third of the esophagus. Esophagogastric resection and cholecystectomy were performed.
Case Report
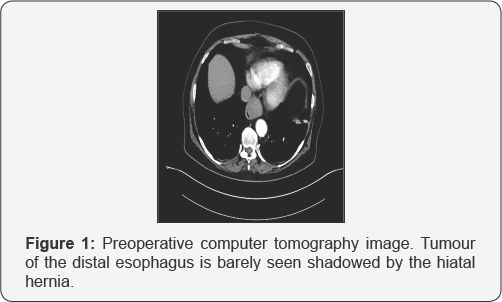
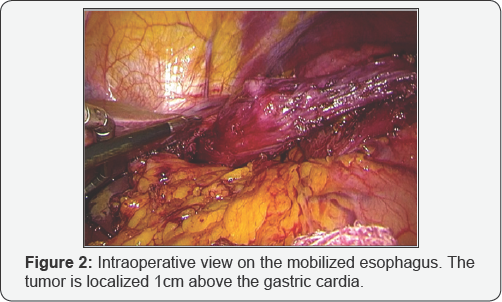
We report a case of 70-year-old woman which presents with complains of pain in the upper right quadrant and epigastrium, heartburn, nausea and constipation. Laboratory results are normal. Esophagogastroscopy reveals a hiatal hernia and reflux esophagitis confirmed by computer tomography along with calculus cholecystitis (Figure 1). Elective laparoscopic hiatal hernia repair and cholecystectomy is planned. Laparoscopy detects hiatus of 3x4cm and axial hiatal hernia of 39x43x45mm fixed in the lower mediastinum, further mediastinal dissection revealed a tumour (Figure 2). Intraoperative endoscopic ultrasound confirms the presence of intramural round tumour with well-defined borders originating from the muscle layer. After upper median laparotomy, we perform a resection of the distal esophagus and the gastric cardia followed by termino-lateral esophagogastric anastomosis with circular stapler, intrathoracic fundoplication above the anastomosis as well as crural repair. Nutritional jejunostomy is placed. Enteral feeding starts on the 24th postoperative hour, oral intake for liquids is restored after the 48th hour and solid foods are allowed after the 72nd hour. The postoperative course is uneventful and the patient is discharged on the 5th postoperative day.
Discussion
Leiomyomas remain asymptomatic in 50% ofthe patients, while the most common symptom is dysphagia combined with chest pain, pyrosis and retrosternal discomfort [5]. Esophageal leiomyoma could be expected to occur from time to time in association with hiatal hernia, the most common lower oesophageal lesion [2]. This author describes two rare cases of hiatal hernia and leiomyoma of the esophagus that remain undetected during preoperative studies. A patient with unexpected intraoperative diagnosis of a large distal esophageal leiomyoma found during laparoscopic repair of a type III hiatal hernia complicated by Cameron ulcer and chronic anemia is also reported [6]. The largest series of leiomyoma in combination with associated esophageal disorders, including hiatal hernia, epiphrenic diverticulum and achalasia is published [4]. Tumour enucleation is successfully performed in 63 patients, esophageal resection in three, and videothoracoscopic enucleation in six ones. Unfortunately, small leiomyomas with intramural growth could be easily missed on esophagoscopy and barium study [2].
Conclusion
Diagnosing the frequent esophageal pathology such as hiatal hernia should not overshadow other rare findings such as benign esophageal tumours. During the laparoscopic hiatal hernia repair, the surgeon should be cautious for other disorders that may change the course of surgery. Esophageal leiomyoma management is well-studied and several minimally invasive options are available, however, the primary cause of surgery should not be ignored.
References
- Beek FA (1957) [A patient with a hiatal hernia, a diverticulum & a leiomyoma of the esophagus]. Belg Tijdschr Geneesk 13(24): 12201222.
- Borrie J (1960) Unsuspected oesophageal leiomyoma found at hiatal herniorrhaphy. Br Med J 1(5178): 1018-1020.
- Cherniavskii AA, Teplova GS (1987) Combined angioleiomyoma of the esophagus with duodenal ulcer and hiatal hernia. Vestn Khir Im I I Grek 139(11): 77-79.
- Bonavina L, Segalin A, Rosati R, Pavanello M, Peracchia A (1995) Surgical therapy of esophageal leiomyoma. J Am Coll Surg 181(3): 257262.
- Pinheiro FA, Campos AB, Matos JR, Araripe DP (2013) Videoendoscopic surgery for the treatment of esophagus' leiomyoma. Arq Bras Cir Dig 26(3): 234-237.
- Holzinger F, Giachino D, Diamantis KE, Birrer S (2007) Unerwarteter, intraoperativer Befund im Bereiche des distalen Osophagus. Der Chirurg 78(6): 548-551.






























