Helicobacter pylori Eradication Therapy: Current Regimens
Dmitrii Andreev*
Department of Internal Diseases Propaedeutics and Gastroenterology, Moscow State University of Medicine and Dentistry, Russia
Submission: September 22, 2017; Published: September 27, 2017
*Corresponding author: Dmitrii N Andreev, Department of Internal Diseases Propaedeutics and Gastroenterology, Moscow State University of Medicine and Dentistry, Delegatskaya Street, 20/1, 127473 Moscow, Russia, Tel: +7-495-609-67-00; Email: dna-mit8@mail.ru
How to cite this article: Dmitrii Andreev. Helicobacter pylori Eradication Therapy: Current Regimens. Adv Res Gastroentero Hepatol 2017; 7(2): 555710. DOI:10.19080/ARGH.2017.07.555710
Abstract
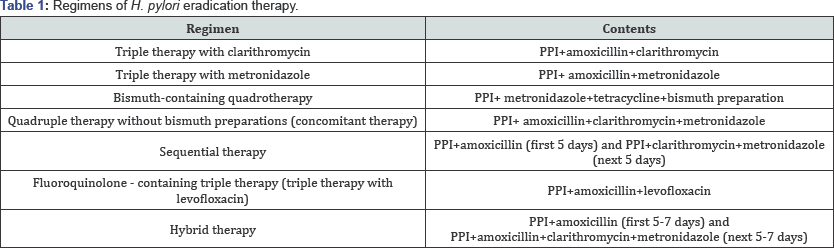
At the moment, 7 regimens of Helicobacter pylori (H. pylori) eradication therapy (ET) are used in clinical practice: triple therapy with clarithromycin, triple therapy with metronidazole, bismuth-containing quadrotherapy, bismuth-free quadrotherapy (concomitant therapy), sequential therapy, fluoroquinolone-containing triple therapy (triple therapy with levofloxacin) and hybrid therapy. According to the latest meta-analyzes, the most effective regimens of ET are sequential therapy, concomitant therapy and hybrid therapy. The highest incidence of adverse events is observed with the use of hybrid therapy
Keywords: Helicobacter pylori; Eradication therapy; Triple therapy; Bismuth-containing quadrotherapy; Sequential therapy; Concomitant therapy; Hybrid therapy\
Abbreviation: ET: Eradication Therapy; PPI: Proton Pump Inhibitor
Introduction
Helicobacter pylori (H. pylori) is the leading etiopathogenetic factor in the development of a number of gastroduodenal diseases, including chronic gastritis, gastric and duodenal ulcer, gastric MALT-lymphoma, and gastric adenocarcinoma of both intestinal and diffuse types [1-3]. In addition, to date, there is evidence of association of H. pylori infection with the development of several extragastroduodenal pathologies represented by iron deficiency anemia of unspecified etiology, idiopathic thrombocytopenic purpura and vitamin B12 deficiency [3-5].
To date, a large number of eradication therapy (ET) regimensare used in the treatment of H. pylori-associated diseases (Table 1). The current stage of the study of H. pylori infection is associated with a negative trend in the decline in the effectiveness of classical ET regimes, which correlates with the growth of antibiotic resistant strains of bacteria in the population [1,3,6]. Based on these data, modern recommendations, including the consensus of Maastricht V (2015), the Toronto Consensus (2016) and the consensus of the American College of Gastroenterologists (2017) regulate a differentiated approach to the appointment of a specific ET regimen depending on the level of regional resistance of the microorganism and local data on the effectiveness of various modes of ET [3,7,8].
Eradication Therapy Regimens
Triple therapy with clarithromycin
Triple therapy with clarithromycin remains the most popular mode of ET in most regions of the world. At the same time, in recent years, the effectiveness of the above regime has significantly decreased [9,10]. According to the latest meta- analyzes, the effectiveness of triple ET is about 69-77% [11-13]. Given this negative trend, consensus Maastricht V and Toronto consensus recommend the use of this protocol only in regions with low resistance to clarithromycin [3,7,8]. In addition, the use of this regimen in persons previously treated with macrolides in the treatment of other diseases is not recommended [8]. The incidence of side effects with the use of triple therapy with clarithromycin reaches 24% with 14 days of therapy [14]. The most common side effects that develop in patients are dysgeusia (impaired taste perception), nausea and diARGHhea.
Triple therapy with metronidazole
The use of triple therapy with metronidazole is in demand in regions with high resistance to clarithromycin, but low resistance to metronidazole [3]. According to the latest metaanalysis, the effectiveness of this treatment protocol is 70.1% he use of triple therapy with metronidazole develop in 30% of patients [13]. In this case, severe side effects that require the termination of the course of ET, are observed only in 1.4% of patients.
Bismuth-containing quadrotherapy
Bismuth-containing quadruple therapy, along with triple therapy with clarithromycin, is the most common protocol for the eradication of H. pylori worldwide [15]. In general, it is believed that the effectiveness of quadrotherapy with bismuth preparations slightly exceeds 80% threshold [1]. In two independent meta-analyzes, it was shown that the effectiveness of this treatment protocol as a first-line regimen is at the level of 77.6-78.3%, and this is quite comparable with the effectiveness of classical triple therapy [12,16]. One of the limiting factors to the wide use of this therapy is the inaccessibility of bismuth and tetracycline preparations in a number of countries [17].
The incidence of side effects in the context of 10-day and 14-day courses of bismuth-containing quadrotherapy is 23%[14].The use of this mode of ET leads to the risk of developing side effects such as headache, nausea, discoloration of teeth and metallic taste in the mouth.
Quadrotherapy without bismuth preparations (concomitant therapy)
A number of researchers consider concomitant therapy as one of the most promising modes of ET in the era of growth of antibiotic resistance [17-19]. Within the framework of this ET, three antibacterial drugs are applied at once, causing a different altering effect on H. pylori. The meta-analysis, which included 19 studies involving 2090 patients, demonstrated high efficacy of the treatment regime, equal to 88% [19]. An updated meta-analysis of 2015 confirms the high level of H. pylori eradication (86.7%) [20]. According to North American consensus, concomitant therapy on a par with bismuth-containing quadratherapy are priority protocols for the first-line ET [7,8].
The use of concomitant therapy is usually characterized by a moderate incidence of side effects, averaging 24% [14]. Patients may experience nausea, dysgeusia, metallic taste in the mouth, dry mouth, diARGHhea, headache and increased AST and ALT in the serum.
Sequential therapy
Sequential therapy remains one of the most studied modes of ET throughout the world, despite the fact that the resistance to clarithromycin has a significant effect on its effectiveness [3]. Interest in sequential therapy is due to its complex mechanism of action on the microorganism. During the first phase of the protocol, clarithromycin-resistant strains of H. pylori and most of the bacteria on the surface of the mucosa are eliminated, and during the second stage -others, including in the depth of the gastric pits and adhered to the epithelium [21,22]. In addition, amoxicillin during the first stage of the application of this protocol leads to a significant reduction in bacterial load and a reduction in the formation of transmembrane efflux channels in the bacterial cell for the removal of antibiotics, which significantly increases the effectiveness of subsequent use of clarithromycin and metronidazole/tinidazole [2 3,24]. According to the results of two meta-analyzes, the effectiveness of sequential therapy is about 84% [11,25].
With the use of sequential therapy, the risk of side effects, in spite of the presence of three antibacterial drugs in its composition, is somewhat lower in comparison with the classical regimens, since each of these drugs is used no more than 5 days. The total incidence of adverse events is 22% [14]. In this case, to the most frequent side effects in the application of this regime can be attributed dysgeusia, metallic taste in the mouth, nausea and headache.
Triple therapy with levofloxacin
Triple therapy with levofloxacin is quite effective in the framework of ET both in the first line and in the second line, but the rapidly progressing pattern of resistance of the microorganism to fluoroquinolones limits the wide use of this protocol [3,8]. According to the latest meta-analysis, the effectiveness of this mode of ET as first-line therapy is 80.7% [26].
The use of triple therapy with levofloxacinis characterized by a good safety profile. With 7-day courses of therapy, adverse events develop in only 15% of patients [14]. The most common side effects when using this mode of ET include nausea, diARGHhea, headache, insomnia, as well as an increase in AST and ALT in the serum.
Hybrid therapy
Hybrid ET is considered as one of the most effective regimens along with concomitant therapy. The mechanism of complex antihelicobacter action of hybrid therapy is similar to sequential therapy and is determined simultaneously by three antibacterial drugs [27]. According to several meta-analyzes, the effectiveness of hybrid therapy is 88.5-91.2% [28-30]. However, this indicator has significant regional differences and requires further validation in different populations.
Despite the high efficiency, hybrid therapy has a suboptimal safety profile. The incidence of adverse events with this mode of ET varies from 26 to 32.9%, depending on the duration of the course of treatment [14,28-30]. However, only 2.5% of cases require discontinuation of the course of ET due to the development of severe side effects [28]. Typically, patients have nausea, dysgeusia, metallic taste or dry mouth, as well as diARGHhea.
Conclusion
At present, 7 regimens of H. pylori ET are used in clinical practice: triple therapy with clarithromycin, triple therapy with metronidazole, bismuth-containing quadrotherapy, quadruple therapy without bismuth preparations (concomitant therapy), sequential therapy, fluoroquinolone - containing triple therapy (triple therapy with levofloxacin), and hybrid therapy. According to the latest meta-analyzes, the most effective regimens of ET are sequential therapy, quadruple therapy without bismuth preparations ("simultaneous therapy”) and hybrid therapy The highest incidence of adverse events is observed with the use of hybrid therapy. Summary data on the effectiveness and safety of ET regimes are given in Table 2.

References
- Morgan DR, Crowe SE (2015) Helicobacter pylori infection. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management.
- Maev IV, Samsonov AA, Andreev DN, Grechushnikov VB, Korovina TI (2013) Clinical significance of Helicobacter pylori infection. Klin Med (Mosk) 91(8): 4-12.
- Malfertheiner P, Megraud F, O'Morain CA, Gisbert JP, Kuipers EJ, et al. (2017) Management of Helicobacter pylori infection-the Maastricht V/ Florence Consensus Report. Gut 66(1): 6-30.
- Maev IV, Andreev DN, Kucheryavyi YA (2015) Helicobacter pylori infection and extragastroduodenal diseases. Ter Arkh 87(8): 103-110.
- Kyburz A, Müller A (2017) Helicobacter pylori and extragastric diseases. Curr Top Microbiol Immunol 400: 325-347.
- Sugano K, Tack J, Kuipers EJ, Graham DY, El-Omar EM, et al. (2015) Kyoto global consensus report on Helicobacter pylori gastritis. Gut 64(9): 1353-1367.
- Fallone CA, Chiba N, van Zanten SV, Fischbach L, Gisbert JP, et al. (2016) The toronto consensus for the treatment of helicobacter pylori infection in adults. Gastroenterology 151(1): 51-69.e14
- Chey WD, Leontiadis GI, Howden CW, Moss SF (2017) ACG clinical guideline: treatment of helicobacter pylori infection. Am J Gastroenterol 112(2): 212-239.
- Malfertheiner P, Link A, Selgrad M (2014) Helicobacter pylori: perspectives and time trends. Nat Rev Gastroenterol Hepatol 11(10): 628-638.
- Graham DY, Lee YC, Wu MS (2014) Rational Helicobacter pylori therapy: evidence-based medicine rather than medicine-based evidence. Clin Gastroenterol Hepatol 12(2): 177-186.
- Feng L, Wen MY, Zhu YJ, Men RT, Yang L (2016) Sequential therapy or standard triple therapy for helicobacter pylori infection: an updated systematic review. Am J Ther 23(3): e880-e893.
- Venerito M, Krieger T, Ecker T, Leandro G, Malfertheiner P (2013) Meta-analysis of bismuth quadruple therapy versus clarithromycin triple therapy for empiric primary treatment of Helicobacter pylori infection. Digestion 88(1): 33-45.
- Puig I, Baylina M, Sanchez-Delgado J, Lopez-Gongora S, Suarez D, et al. (2016) Systematic review and meta-analysis: triple therapy combining a proton-pump inhibitor, amoxicillin and metronidazole for Helicobacter pylori first-line treatment. J Antimicrob Chemother 71(10): 2740-2753.
- Li BZ, Threapleton DE, Wang JY (2015) Comparative effectiveness and tolerance of treatments for Helicobacter pylori: systematic review and network meta-analysis. BMJ 351: h4052.
- Lee JY, Park KS (2016) Optimal First-Line Treatment for Helicobacter pylori Infection: Recent Strategies. Gastroenterol Res Pract 2016: 9086581.
- Luther J, Higgins PD, Schoenfeld PS, Moayyedi P, Vakil N, et al. (2010) Empiric quadruple vs. triple therapy for primary treatment of Helicobacter pylori infection: Systematic review and meta-analysis of efficacy and tolerability. Am J Gastroenterol 105(1): 65-73.
- Ermis F, Senocak Tasci E (2015) Current Helicobacter pylori treatment in 2014. World J Methodol 5(2): 101-107.
- Essa AS, Kramer JR, Graham DY, Treiber G (2009) Meta-analysis: four- drug, three-antibiotic, non-bismuth-containing "concomitant therapy” versus triple therapy for Helicobacter pylori eradication. Helicobacter 14(2): 109-118.
- Gisbert JP, Calvet X (2012) Update on non-bismuth quadruple (concomitant) therapy for eradication of Helicobacter pylori. Clin Exp Gastroenterol 5: 23-34.
- He L, Deng T, Luo H (2015) Meta-analysis of sequential, concomitant and hybrid therapy for Helicobacter pylori eradication. Intern Med 54(7): 703-710.
- Maev IV, Kucheryavyi YuA, Andreev DN, Barkalova EV (2014) Eradication therapy for Helicobacter pylori infection: review of world trends. Ter Arkh 86(3): 94-99.
- Gisbert JP, Calvet X, O'Connor JP, Megraud F, O'Morain CA (2010) The sequential therapy regimen for Helicobacter pylori eradication. Expert Opin Pharmacother 11: 905-918.
- Vaira D, Zullo A, Hassan C, Fiorini G, Vakil N (2009) Sequential therapy for Helicobacter pylori eradication:The time is now! Therap Adv Gastroenterol 2: 317-322.
- Zullo A, De Francesco V, Hassan C, Morini S, Vaira D (2007) The sequential therapy regimen for Helicobacter pylori eradication: A pooled-data analysis. Gut 56: 1353-1357.
- Gatta L, Vakil N, Vaira D, Scarpignato C (2013) Global eradication rates for Helicobacter pylori infection: systematic review and meta-analysis of sequential therapy. BMJ 347: f4587.
- Chen PY, Wu MS, Chen CY (2016) Systematic review with meta-analysis: the efficacy of levofloxacin triple therapy as the first- or second-line treatments of Helicobacter pylori infection. Aliment Pharmacol Ther 44(5): 427-437.
- Andreev DN, Dicheva DT, Maev IV (2017) Possibilities for optimization of eradication therapy for Helicobacter pylori infection in modern clinical practice.Ter Arkh 89(2): 84-90.
- Song ZQ, Liu J, Zhou LY (2016) Hybrid Therapy Regimen for Helicobacter Pylori Eradication. Chin Med J (Engl) 129(8): 992-999.
- Hsu PI, Lin PC, Graham DY (2015) Hybrid therapy for Helicobacter pylori infection: A systemic review and meta-analysis. World J Gastroenterol 21(45): 12954-12962.
- Song ZQ, Zhou LY (2016) Hybrid, sequential and concomitant therapies for Helicobacter pylori eradication: A systematic review and meta-analysis. World J Gastroenterol 22(19): 4766-4775.






























