Awareness Survey of Prejudice and Discrimination in Hepatitis B and C Virus- Infected Individuals
Yumiko Nagao1*, Yuji Kawahigashi1, Kanae Kimura1, Haruhiko Nobayashi2 and Michio Sata3,4
1Department of Organ System Interactions and Information, Faculty of Medicine, Saga University, Japan
2Community and Culture Department, Hokuriku Gakuin Junior College, Japan
3Research Center for Innovative Cancer Therapy, Kurume University School of Medicine, Japan
4Nishinihon Hospital, Kumamoto, Japan
Submission: August 25, 2017; Published: August 30, 2017;
*Corresponding author: Yumiko Nagao, Department of Organ System Interactions and Information, Faculty of Medicine, Saga University, Nabeshima, Saga, 849-8501, Japan, Tel: +81-952-34-2516; Fax: +81-952-34-2516; Email: nagaoyu@cc.saga-u.ac.jp
How to cite this article: Yumiko N, Yuji K, Kanae K, Haruhiko N, Michio S. Awareness Survey of Prejudice and Discrimination in Hepatitis B and C Virus- Infected Individuals. Adv Res Gastroentero Hepatol 2017; 7(1): 555703. DOI: 10.19080/ARGH.2017.07.555703
Abstract
Background: In Japan, an appropriate understanding of hepatitis C virus (HCV) and hepatitis B virus (HBV) infection is not sufficiently prevalent among the public. Furthermore, there are few survey studies on prejudice and discrimination of HBV- and HCV-infected patients with liver disease by healthcare workers. The aims of this study were to perform a survey on healthcare worker prejudice and discrimination of HBV- and HCV-infected patients.
Materials and Methods: We administered a questionnaire survey to a total of 131 persons who participated in a lecture open to the public entitled the 26th 'Seminar for Digestive Disease'. The questionnaire addressed the following: background, psychological burden, experience of prejudice and discrimination from a healthcare worker, and clinical departments where patients experienced prejudice.
Results: We collected information from 127 of 131 anonymous individuals (96.9%). Of the 127 individuals, 69 had viral liver disease, 42 had no viral liver disease, and 16 had unknown status. Of the 69 with viral liver disease, 53 individuals revealed a psychological burden (76.8%) and 14 experienced prejudice and discrimination by healthcare workers (20.3%). Prejudice was most prevalent within the dental clinic setting (7/14, 50%). Significant factor involved in psychological burden was presence or absence of experience prejudice by a healthcare worker (P= 0.0255).
Conclusions: It is necessary for all healthcare workers to promote public awareness and accurate information relating to prevention and treatment of hepatitis, particularly dental professionals.
Keywords: Hepatitis C virus; Hepatitis B virus; Prejudice and discrimination; Dental professionals
Abbreviations: HCV: Hepatitis C Virus; HBV: Hepatitis B Virus; CH-C: Chronic Hepatitis C; LC-C: Liver Cirrhosis Type C; HCC: Hepatocellular Carcinoma; IFN: Interferon; SVR: Sustained Virological Response; DAA: Direct-Acting Antivirals
Introduction
Approximately three million Japanese people are infected with hepatitis C virus (HCV) or hepatitis B virus (HBV) [1,2]. Eradicating the virus by antiviral therapy can reduce the likelihood of hepatocellular carcinoma (HCC), advanced liver disease, and liver-related mortality [3,4]. Recently, the development of a direct-acting antiviral drug (DAA) on HCV has drastically improved liver-related morbidity and mortality [5,6].
However, an appropriate understanding of HCV and HBV infection is not sufficiently prevalent among the public. It has been reported that 23.7% of individuals expressed prejudiced opinions towards HBV/HCV-infected Japanese colleagues, although HCV/HBV cannot be transmitted through casual contact in the workplace [7]. The authors of that study concluded that assimilation of accurate knowledge might decrease individuals' negative attitudes towards HCV- and HBV-infected colleagues.
We previously analyzed factors, which motivated HCV- infected patients to accept interferon (IFN) therapy and demonstrated the importance of effort and strength of explanations or recommendations given by physicians to the patients [8]. Therefore, we have been holding regional seminars entitled "Seminars for Digestive Disease", since October 2005 that offer accurate medical information relating to liver disease and extrahepatic manifestations. These were initiated to help patients, their families, and citizens understand these diseases. A total of 5,161 people had participated in seminars by September 2016. We previously demonstrated that people who participated in more than 5 seminars had improved knowledge of liver disease as well as increased awareness and health-promoting behavior [9].
In this study, we conducted a survey on prejudice and discrimination among participants to whom medical information was offered in seminars for digestive disease.
Materials and Methods
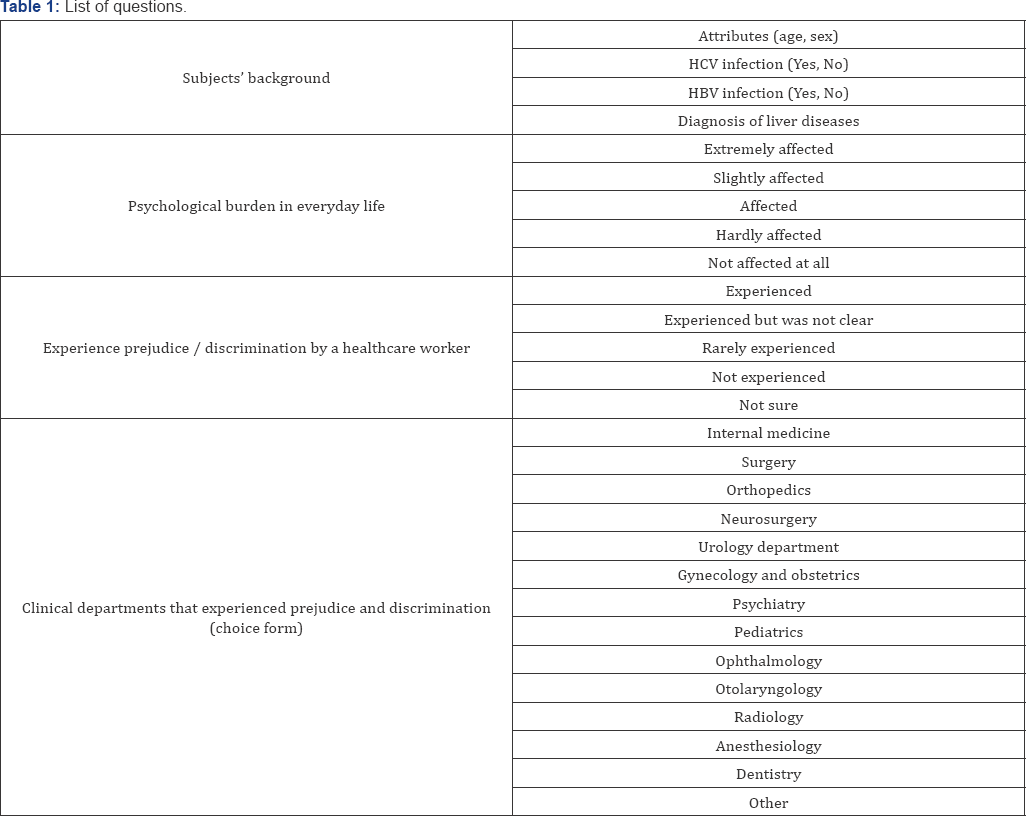
We conducted a questionnaire survey on a total of 131 Japanese individuals that participated in the 26th Seminar for Digestive Disease, held on September 24, 2016. On the seminar date, we handed out a questionnaire form to 131 participants and collected these on an anonymous basis. The list of questions is given in Table 1. We received questionnaires from 127 of 131 individuals (96.9%). Of the 12 7, 69 had viral liver disease, 42 had no viral liver disease, and 16 were of unknown status.
This investigation was undertaken with the understanding and consent of each participant and was conducted in full accordance with the ethical principles of the World Medical Association Declaration of Helsinki.
Statistical Analysis
All data are expressed as mean ± standard error. Differences between 2 groups were analyzed using the Wilcoxon's test and Fisher's exact test. Differences were deemed significant at p<0.05 (2-tailed). All statistical analyses were conducted using JMP Version 11.1.1 software (SAS Institute, Cary, NC, USA). The level of statistical significance was defined as p<0.05.
Results
Characteristics of the 69 subjects
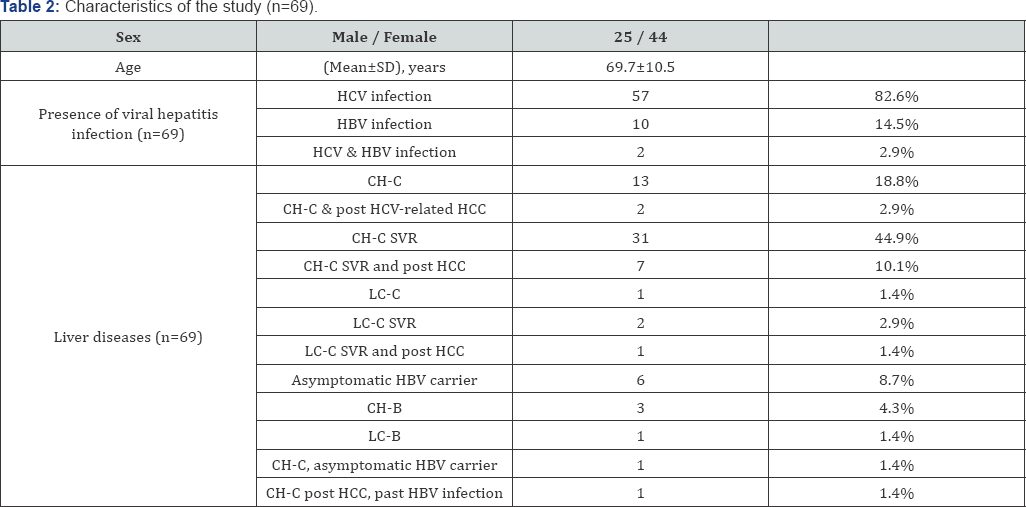
The 69 individuals comprised 25 men and 44 women with a mean age of 69.7±10.5 years (Table 2). The diagnosis of liver disease among 69 persons was: chronic hepatitis C (CH-C)(n=13, 18.8%), CH-C post HCC (n=2, 2.9%), CH-C sustained virological response (SVR) (n=31, 44.9%), CH-C SVR post HCC (n=7, 10.1%), liver cirrhosis (LC-C) type C (n=1, 1.4%), LC-C SVR (n=2, 2.9%), LC-C SVR post HCC (n=1, 1.4%), asymptomatic HBV cARGHier (n=6, 8.7%), chronic hepatitis B (CH-B) (n=3, 4.3%), liver cirrhosis type B (LC-B) (n=1, 1.4%), CH-C & asymptomatic HBV cARGHier (n=1, 1.4%), and CH-C post HCC &past HBV infection (n=1, 1.4%).
Psychological burden experienced by those with viral liver disease in everyday life
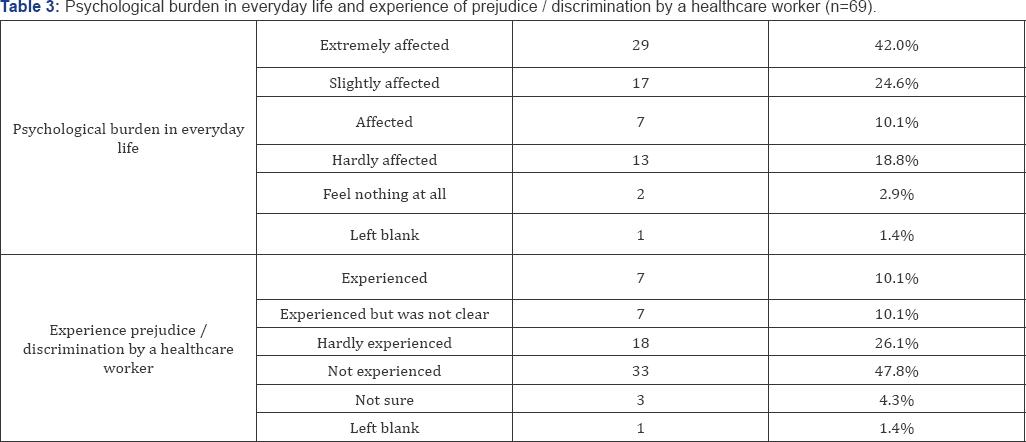
In 69 individuals with viral liver disease, 29 (42.0%) experienced extreme psychological burden in everyday life relating to their condition until time of survey. 17 (24.6%) had experienced significant psychological burden and 7 (10.1%) had a degree of psychological burden (Table 3). We compared the characteristics of 53 individuals with psychological burden and 15 without psychological burden in 68 subjects who blanks answer (one) is excluded. The characteristics of the 68 subjects are shown in Table 4. Significant factor was presence or absence of experience prejudice by a healthcare worker (P= 0.0255). In 57 individuals only for HCV infection, SVR group and non- SVR were 40 and 17 subjects, respectively. Rate of experienced psychological burden was higher in the non-SVR group (15, 88.2%) than in the SVR (30, 75.0%), although there was no significant difference between the two groups.

*Blanks answer (one) is excluded
NS, not significant
Experience of prejudice/discrimination from a healthcare worker by those with viral liver disease
In 69 individuals with viral liver disease, 7 (10.1%) had experienced prejudice and discrimination by a healthcare worker; 7 (10.1%) had experienced a form of prejudice and discrimination but it was not clear (Table 3). Of those 14 people who had experienced prejudice and discrimination, the clinical departments where they experienced these events were as follows: dental clinic, n=7 (50%); orthopedic surgery clinic, n=1 (7%); otolaryngology clinic, n=1 (7%); ophthalmic clinic, n=1 (7%); gynecology and obstetrics clinic, n=1 (7%); surgical clinic, n=1 (7%); and blood collection room, n=1 (7%).
Discussion
There have been some reports that have assessed stigma and discrimination in relation to HCV infection within the healthcare setting [10,11]. However, there are few studies that have described the experiences of HCV/HBV-infected patients who experience discriminatory treatment by a healthcare worker.
In this study, among 69 individuals with HCV/HBV-driven liver disease, 76.8% experienced the psychological burden of disease in everyday life and 20.3% experienced prejudice and discrimination from a healthcare worker. The most common clinical department where such discrimination occurred was dentistry (50%). We were able to obtain an act of definite discrimination from the contents of the free answer to anonymous questionnaire in some subjects. In such dental clinics, viral infected individuals received non-treatment decisions, experienced a discriminatory manner, or when their personal information was not considered. The rate of experience prejudice by a healthcare worker was higher in group with psychological burden (26.4%) than in group without psychological burden (0%, P= 0.0255).
We previously reported self-disclosure of HCV or HBV infection to dentists [12]. We cARGHied out a questionnaire survey of 209 patients to determine whether patients with HCV or HBV disclosed their disease status to dental clinic personnel. 59.8% stated that they always did, 12.0% sometimes did, and 28.2% never self-disclosed. The main reason (71.2%) for non-disclosure was failure of dental healthcare workers to ask whether patients had systemic disease. Other reasons included fear of negative reactions from healthcare workers (11.9%) and not wanting dentists or staff to know their specific liver ailment (10.2%). When HCV/HBV-infected patients received a negative response from a healthcare worker, the patient tended to hide their viral hepatitis infection in all clinical departments. Such behavior can result in nosocomial infections as well as inappropriate treatment.
Yoshikawa et al. [13] conducted a nationwide survey on the factors inhibiting the acceptance of dental care for 1,462 HIV patients at dental clinics in Japan. The authors showed that inadequate infection control and a lack of information about dental care made dental care for HIV patients difficult. According to this questionnaire survey, 80.5% of dental clinics provided dental care for HCV/HBV-infected patients but the remainder did not.
Eguchi et al. [7] evaluated the association between higher levels of knowledge and negative attitudes toward HBV- and HCV- infected colleagues among the Japanese working population. The authors concluded that an increase in knowledge was associated with an improvement in individuals' negative attitudes towards HBV- and HCV-infected colleagues.
There are several reasons why patients with HCV/HBV hepatitis experience both prejudice and discrimination. Tatsuoka et al. [14] reported three factors relating to prejudice and discrimination experienced by patients with viral hepatitis. The first was negative discrimination from a layperson because they had awareness that HBV/HCV infection can progress to liver cirrhosis and HCC, and HCV/HBV have the potential to infect other people (including themselves presumably). The second reason why discrimination and prejudice occur is an emotional response from the laypers on, where they believe that viral hepatitis is a dreadful disease because of insufficient knowledge of viral hepatitis. The third form of discrimination and prejudice is the ending of a relationship, where individuals around those diagnosed with HCV/HBV no longer wish to become involved with HBV/HCV-affected individuals.
HCV infection induces liver disease as well as extrahepatic manifestations. In the oral conditions, it is well known that lichen planus, Sjogren's syndrome and oral cancer are associated with HCV infection [15,16]. Lately, IFN-free DAA with SVR DAA with SVR rates and few side effects have changed the treatment of hepatitis C markedly [5,6,17]. However, in Japan, the latest information about hepatitis is hardly offered to dentists and dental students. The still unsolved dental education of Japan seems to influence an act to discriminate against hepatitis- infected individuals.
This study has some limitations. Firstly, limitations to our study include the small sample size. Further research with a large-scale is required. A second limitation of our study is that we did not interview the subjects because of an anonymous basis. However, this is the significant study to investigate prejudice and discrimination from healthcare workers among viral infected patients in Japan.
Conclusion
We performed a survey on prejudice and discrimination experienced by HCV/HBC-infected individuals from healthcare workers. In Japan, there is not enough accurate knowledge relating to HCV/HBV infection amongst the general population. It is necessary to promote public awareness and information services in order to improve understanding of prevention, pathology, and treatment of hepatitis. Close cooperation and support from dental and medical clinics, correct disclosure of information, and education are necessary to provide appropriate medical care to patients with hepatitis without being unfairly discriminated against.
Acknowledgements
This study was supported in part by a Grant-in-Aid for Scientific Research (C) (No.25463274 and No.17K12012) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
We thank our volunteers who helped organize the seminars: Mr. Kazuki Tsunoda, Mr. Junjirou Rikitake, Ms. Mayumi Tsuji, Ms. Akari Sugimoto, Mr. Yoshihiko Otsuji, Mr. Isamu Suzuki, Mr. Kousho Nishimura, Ms. Mako Okumoto, Ms. Yuna Furuta, Ms. Yuka Watanabe, Ms. Yuki Nakao, Ms. Rikako Kobayashi, Mr Kengo Shigenaga, Mr. Koushi Toyoizumi, Mr. Kenta Nakayama, Mr. Yohei Mizunoe, Ms. Mako Ishibashi, Ms. Junna Kimura, Ms. Haruka Nakamura, Ms.Kaori Seo, and Ms. Yuka Yoshimoto (Kurume University)
Conflict of interest
YN, KK, and YK belong to a department funded by Nishinihon Hospital. The remaining authors disclose no conflicts.
References
- Higuchi M, Tanaka E, Kiyosawa K (2002) Epidemiology and clinical aspects on hepatitis C. Jpn J Infect Dis 55(3): 69-77.
- Lavanchy D (2009) The global burden of hepatitis C. Liver Int 29(Suppl 1): 74-81.
- Yoshida H, Shiratori Y, Moriyama M, Arakawa Y, Ide T, et al. (1999) Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of Hepatocarcinogenesis by Interferon Therapy. Ann Intern Med 131(3): 174-181.
- Yamasaki K, Tomohiro M, Nagao Y, Sata M, Shimoda T, et al. (2012) Effects and outcomes of interferon treatment in Japanese hepatitis C patients. BMC Gastroenterol 12(1): 139.
- Kumada H, Suzuki Y, Ikeda K, Toyota J, Karino Y, et al. (2014) Daclatasvir plus asunaprevir for chronic HCV genotype 1b infection. Hepatology 59(6): 2083-2091.
- Horsley-Silva JL, Vargas HE (2017) New therapies for hepatitis C virus infection. Gastroenterol Hepatol (N Y) 13(1): 22-31.
- Eguchi H, Wada K (2013) Knowledge of HBV and HCV and individuals' attitudes toward HBV- and HCV-infected colleagues: a national cross-sectional study among a working population in Japan. PLoS One 8(9): e76921.
- Nagao Y, Sata M (2008) Analysis of factors interfering with the acceptance of interferon therapy by HCV-infected patients. Med Sci Monit 14(11): Pi45-52.
- Nagao Y, Kawahigashi Y, Sata M, Nobayashi H (2015) Effect of patient education seminars on awareness and behavior of individuals with viral liver disease. Med Sci Tech 56: 120-126.
- Crofts N, Louie R, Loff B (1997) The next plague: stigmatization and discrimination related to hepatitis C virus infection in Australia. Health Hum Rights 2(2): 87-97.
- Treloar CJ, Hopwood MN, Loveday SK (2002) Hepatitis C-related discrimination in healthcare. Report of the Third Australasian Conference on Hepatitis C, Melbourne, Med J Aust 177(5): 233-234.
- Nagao Y, Kawaguchi T, Ide T, Sata M (2008) HCV or HBV infection self-disclosure to dentists. Kansenshogaku Zasshi 82(3): 213-219.
- Yoshikawa H, Tagami T, Yamaguchi Y (2008) A study of the dental- care collaboration system for HIV infected patients (in Japanese). The Journal of AIDS research 10(1): 41-49.
- Tatsuoka S (2015) A study on prejudice and discrimination against patients with viral hepatitis (in Japanese). Gakushuin Houmu Study 9: 1-15.
- Nagao Y, Sata M, Tanikawa K, Itoh K, Kameyama T, et al. (1995) High prevalence of hepatitis C virus antibody and RNA in patients with oral cancer. J Oral Pathol Med 24(8): 354-360.
- Nagao Y, Nishida N, Toyo-Oka L, Kawaguchi A, Amoroso A, et al. (2017) Genome-wide association study identifies risk variants for lichen planus in patients with hepatitis C virus infection. Clin Gastroenterol Hepatol 15(6): 937-944.e5.
- Nagao Y, Kimura K, Kawahigashi Y, Sata M, et al. (2016) Successful treatment of hepatitis C virus-associated oral lichen planus by interferon-free therapy with direct-acting antivirals. Clin Transl Gastroenterol 7(7): e179.






























