The Profile of Food Protein Allergy in Children below 2 Years in Eastern India–An Observational Study
Bhaswati C Acharyya1, Chandrayee Bhattacharyya2 and Saumyabrata Acharyya2
1Dept of Paediatric Gastroenterology, AMRI Hospitals, India
2Dept of Paediatrics, AMRI Hospitals, India
Submission: February 05, 2017; Published: March 27, 2017
*Corresponding author: Bhaswati C Acharyya, Department of Pediatrics Gastroenterology, AMRI Hospitals, Kolkata, India, Email:bukuII2@hotmaiI.com
How to cite this article: Bhaswati C A, Chandrayee B, Saumyabrata A. The Profile of Food Protein Allergy in Children below 2 Years in Eastern India–An Observational Study. Adv Res Gastroentero Hepatol 2017; 4(3): 555638. DOI: 10.19080/ARGH.2017.04.555638
Abbreviations
Abbreviations:CMPA: Cow’s Milk Protein Allergy
Background and Aim
Food allergy has been referred to as the second wave of the allergy epidemic, asthma being the first [1]. Incidence of food protein allergy, especially cow’s milk protein allergy Is on a rise In India. The aim of this study was to find out the presentation, cross allergy and outcome after treatment of the infants and children below 2 years of age who had been diagnosed with food protein allergy, in a tertiary centre of Eastern India.
Materials and Methods
A retrospective study was undertaken where the case files of children below 2 years, who were diagnosed to have food protein allergy between the years March 2014 to Dec 2015, were analysed. These children were reviewed in the Paediatric Gastroenterology department of a tertiary centre in Kolkata. Upper GI Endoscopy, Sigmoidoscopy/colonoscopy and immunoglobulin E against Cow’s milk protein (using Immunocap Allergy test modality) were used as diagnostic modalities. Celiac screening was done in all patients above 6 months who were already exposed to wheat. Endoscopic diagnosis of food protein allergy was based on characteristic intestinal biopsy (>6 eosinophils/HPF in recto sigmoid and >20 eosinophils/HPF in duodenal and Gastric biopsies and >15 eosinophil /HPF in oesophageal biopsies).
Results
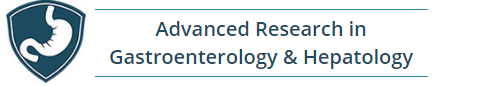
60 children (26 males and 36 below 1year of age) have been diagnosed with food protein allergy among a total of 120 children(less than 2 years) attending clinic with GI symptoms. Mean age was 9+2 months and median duration of symptoms ware 5.5 months. Vomiting and or severe gastro esophageal reflux disease was presentation in 15 (25% patients). Haematemesis was presentation in 5 (8.3%) infants. DiARGHhoea (watery and Bloody ) was present in 39(65%) children and amongst them 26(43.3%) had bloody diARGHhoea . 2(3.3%) infants presented with severe anaphylactic shock in neonatal age group and severe enterocolitis was presenting feature in 3 infants (5%). Duodenal lymphoid nodular hyperplasia was the finding in 80% cases presenting with vomiting. Ulcerative procto-colitis with or without lymphoid nodular hyperplasia was the finding in all cases (100%) of bloody diARGHhea (Figure 1& 2). IgE against cow’s milk protein (Immunocap) was positive in 3 patients (5%) (Evaluated in 12 patients). Cow’s milk was excluded from the diet for all children. Hydrolysed infant formula was used in infants below 6 months. Peptide based formula and soya formula were used in rest. 10 (16.6%) patients were found to be cross allergic to Soya protein. 2 were found allergic to Chicken protein. Celiac screen was positive in a boy of 20 months who also had eosinophilic proctocolitis and was kept on Peptide based formula and gluten free diet. Median duration of milk exclusion was 18 months. All patients were followed up monthly for 2 months, 2 monthly for three visits and 3 monthly thereafter until 18 months in total since diagnosis. Milk challenge was not done routinely. Accidental milk in mother's diet caused recurrence of symptoms in 5 patients when done within 1 year While 8 patients are still on milk exclusion rest 50 patients did well after gradual introduction of milk after 18 months of restriction. 2 were lost in follow up (Table 1, Figure 1& 2).
Discussion
Food allergies affect 68% of infants younger than 2 years. In a cohort of 1,749 newborns from the municipality of Odense in Denmark who were prospectively monitored for the development of cow’s milk protein intolerance during the first year of life, a 1 year incidence of 2.2% was reported [2]. Varying incidences of specific intolerances have been reported in different countries. Whether these differences are due to genetic or cultural factors is unclear [3].Cow’s milk, the commonest food has been shown to be the common cause of chronic diARGHhea in children <3 years of age in India [4].
DiARGHhoea was the commonest presentation of CMPA in our study (65% with 43.3% bloody diARGHhoea) which is similar to the study of Poddar et al who also showed diARGHhea as commonest presentation (90%) and 2/3rd was large bowel diARGHhea [4]. Rectal bleeding is a common manifestation of CMPA [5]. Therefore, CMPA should always be the first possibility in infants with rectal bleeding, over and above rectal polyp, as the latter is less common in infancy [6].
Sigmoidoscopy was diagnostic in 100% cases of bloody diARGHhea and about 82% cases of diARGHhea in our study which was similar to the other study [7]. It has been shown that on cow’s milk withdrawal there is rapid reversal of histopathological changes and on re-exposure to milk there is rapid deterioration in 24-48 hours [8].
In previous studies re-challenge with milk was done after 3 months in 80% of cases showing positive results [7]. But in our study routine re-challenge was not done but accidental milk in mother's diet caused recurrence of symptoms in 5 patients when done within 1 year. A total of 18 months restriction has been advocated for all patients.
Conclusion
Food protein allergy especially CMPA is now a common entity in India. This study also confirms that Cow’s Milk Protein Allergy is an existing entity in the young population below 2 years in the eastern part of India as well. High index of suspicion and appropriate referral can achieve early diagnosis and symptomatic relief. Gradual introduction of food protein after adequate period of restriction is successful in most of the cases.
References
- Prescott S, Allen KJ (2011) Food allergy: riding the second wave of the allergy epidemic. Pediatr Allergy Immunol 22(2): 155-160.
- Assa'ad A (2009) Eosinophilic gastrointestinal disorders. Allergy Asthma Proc 30(1): 1722.
- Hill DJ, Hosking CS, Heine RG (1999) Clinical spectrum of food allergy in children in Australia and SouthEast Asia: identification and targets for treatment. Ann Med 31(4): 27281.
- Poddar U, Shukla P, Yachha SK, Aggarwal R, Krishnani N (2008) Role of IgG anti-beta-lactoglobulin antibody in the diagnosis of cow's milk protein intolerance in India. Indian J Gastroenterol 27(5): 190-194.
- Xanthakos SA, Schwimmer JB, Melin-Aldana H, Rothenberg ME, Witte DP, et al. (2005) Prevalence and outcome of allergic colitis in healthy infants with rectal bleeding: a prospective cohort study. J Pediatr. Gastroenterol. Nutr 41(1): 16-22.
- Poddar U, Thapa BR, Vaiphei K, Singh K (1998) Colonic polyps: experience of 236 Indian children. Am J Gastroenterol 93(4): 619-22.
- Poddar U, Yachha S K, Krishnani N, Srivastava A (2010) Cow^s milk protein allergy: An entity for recognition in developing countries. J of Gastroenterol Hepatol 25(1): 178-182.
- Walker-Smith JA (1992) Cow^s milk-sensitive enteropathy: predisposing factors and treatment. J Pediatr 12(5 pt 2): S111-S115.