All-oral Treatment with Daclatasvir and Asunaprevir for HCV Genotype 1 and Impact of Add-on Therapy with Lipid Modulators
Motoyuki Kohjima1,2, Kenta Motomura2, Toshimasa Koyanagi2, Seiya Tada2, Naoki Yamashita2, Takeaki Sato2, Rie Sugimoto2, Masaki Yokota2, Kotaro Uchimura2, Hironori Sakai2, Nobuhiko Higashi2, Shusuke Morizono2, Masami Kuniyoshi2, Makoto Tokumatsu2, Masanao Honda2, Tsuyoshi Yoshimoto1,2, Nobito Higuchi1,2, Kunitaka Fukuizumi1, Kenji Ohe3, Kazuhiro Kotoh2,4, Munechika Enjoji2,3*, Masaki Kato2,4 and Makoto Nakamuta1,2
1Department of Gastroenterology and Clinical Research Center, National Hospital Organization Kyushu Medical Center, Japan
2Fukuoka Kanzo Treatment Research Group, Japan
3Health Care Center, Fukuoka University, Japan
4Department of Medicine and Bioregulatory Science, Kyushu University, Japan
Submission: September 26, 2016; Published: October 04, 2016
*Corresponding author: Munechika Enjoji, Health Care Center, Fukuoka University, 8-19-1 Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan.
How to cite this article: Motoyuki K, Kenta M, Toshimasa K, Seiya T, Naoki Y. et al. All-oral Treatment with Daclatasvir and Asunaprevir for HCV Genotype 1 and Impact of Add-on Therapy with Lipid Modulators. Adv Res Gastroentero Hepatol. 2016; 2(1): 555579. DOI: 10.19080/ARGH.2016.02.555579
Abstract
Objective: Despite improved treatment options, many patients with hepatitis C virus (HCV) infection remain HCV-positive. The all-oral therapy with daclatasvir and asunaprevir has recently been approved for treatment of patients with HCV. We conducted a prospective study to investigate the effectiveness and safety of this therapy.
Methods: We treated 696 patients with HCV genotype 1 with daclatasvir and asunaprevir for 24 weeks. Resistance-associated substitutions (RASs) in HCV were analyzed by direct sequencing of the HCV NS3 and NS5A domains.
Results: HCV RNA declined rapidly after treatment initiation, and 90.9% of patients achieved a sustained virological response at 12 weeks after treatment termination (SVR12). Elevation of serum transaminases and alkaline phosphatase, pyrexia, headache, malaise, and skin eruption were common adverse events. In multivariate analysis, treatment history of simeprevir and HCV RASs were selected as adverse predictive factors, meanwhile addition of pitavastatin and eicosapentaenoic acid (EPA) was selected as a favorable predictive factor associated with SVR12.
Conclusion: Treatment response of HCV was favorable enough during the daclatasvir and asunaprevir therapy. HCV RASs and prior treatment history with simeprevir could weaken the efficacy of this therapy, whereas, the lipid modulators, pitavastatin and EPA, could enhance it through a synergistic antiviral effect.
Keywords: Hepatitis C virus; Eicosapentaenoic acid; Statin; Daclatasvir; Asunaprevir
Introduction
Approximately 170 million people are infected with hepatitis C virus (HCV) worldwide and natural history studies have shown that 5%–20% of patients develop cirrhosis after 20 years of infection [1,2]. People who test positive for HCV antibodies account for 1.4%–1.7% of the general population in Japan, and a few million individuals are estimated to have chronic HCV infection. The majority of patients with HCV in Japan are older than those in the United States and Europe, and ≥60% of the population is aged ≥60 years in Japan [3]. This aging population is characterized by an increasing incidence of progressive liver disorders.
Pegylated-interferon (peg-IFN) plus ribavirin (RBV) combination therapy was the standard of care for chronic hepatitis C until the 2000s. However, in patients infected with genotype 1 HCV (HCV-1 patients) with high viral load, at most, 50% of patients achieve a sustained virological response (SVR) after the therapy [4,5]. Response to treatment based on IFN is influenced by virus-related factors including viral load, genotype, and amino acid substitutions at core 70 and 91; hostrelated factors, such as sex, age, insulin resistance, disease stage, response to previous antiviral therapy, and IL28B polymorphism; as well as therapeutic factors, such as dose and duration of treatment [6-16].
The direct-acting antiviral agents (DAAs) have made a huge impact on hepatitis C therapy. The HCV NS3 protease inhibitor telaprevir (TVR), in combination with peg-IFN and RBV, was approved for the treatment of serogroup 1 chronic hepatitis C in September 2011. This combination has achieved SVR rates of 80%–90% for HCV-1 patients [17,18]. The second-generation protease inhibitors simeprevir (SMV) and vaniprevir were approved and also showed SVR rates of 80%–90% [19,20]. These treatments was not sufficient in some cases, and SVR rates for DAA-based peg-IFN/RBV treatment in patients with intractable IL28B polymorphism were still 50%–70%, and only 30%–50% of null responders achieved SVR [21]. Furthermore, these treatments were associated with severe anemia, skin disorder, renal dysfunction, pyrexia, general malaise, hematological abnormalities, and psychiatric symptoms, and many patients were ineligible for IFN treatment because of age or advanced liver fibrosis [17-21].
Combination therapy with first-in-class selective NS5A replication complex inhibitor daclatasvir (DCV; BMS-790052) and potent NS3 protease inhibitor asunaprevir (ASV; BMS- 650032) was approved for HCV-1 patients with chronic hepatitis or compensated cirrhosis in July 2013 in Japan. Monotherapy with each drug is associated with treatment refractoriness because of the emergence of resistant virus. However, DCV and ASV have different modes of action and different characteristics that cause resistance-associated substitutions (RASs) in HCV, combined use of both drugs is expected to yield a high SVR rate of at least 80%–90% [22,23]. Although the combination therapy is also indicated for compensated cirrhosis, a low incidence of adverse events and high treatment tolerability is expected, which is explained by the lack of IFN and RBV use [24-29].
HCV life cycle is closely correlated with lipid metabolism in hepatocytes. It has been suggested that serum cholesterol and statin use predict virological response to combination therapies [30]. Recent studies have shown that virological response is improved by addition of fluvastatin or pitavastatin to peg-IFN/ RBV treatment [31-33]. Moreover, statins were associated with a reduced risk of hepatocellular carcinoma (HCC) in a large cohort of patients with diabetes [34]. In other studies, it has been demonstrated that polyunsaturated fatty acids (PUFAs) inhibit HCV replication by a mechanism that is independent of their roles in regulating lipogenesis [35-38]. Recently, we have shown that addition of pitavastatin and EPA to peg-IFN/RBV treatment improved SVR rates in HCV-1 patients, especially in those with the intractable IL28B genotype, and addition of pitavastatin and EPA might activate innate immunity, block viral entry into hepatocytes, and suppress lipogenesis in the liver [39]. However, little is known about the additive effect of lipid modulators in inhibiting HCV replication during DAA treatment.
We conducted a prospective multicenter study to investigate the efficacy of dual oral therapy with DCV and ASV. We also present here post-marketing efficacy and safety assessment of dual oral combination therapy with DCV and ASV in HCV-1 patients. The predictors of treatment efficacy were investigated and are discussed, including addition of lipid modulators, pitavastatin and EPA.
Methods
Fukuoka Kanzo Treatment Research Group conducted a prospective multicenter study to investigate the efficacy and safety of all-oral treatment with DCV and ASV in HCV-1 patients. Eligible patients were men and women aged ≥20 years with genotype 1 chronic hepatitis C or compensated cirrhosis. Patients were excluded if they had evidence of hepatic decompensation, suspected HCC or active cancer at entry, pregnancy in progress or planned during the study period, organic obstruction of the digestive tract, serious cardiovascular lesions, severe infection, serious trauma, or severe or unstable complications, such as other organ failure. From September 2014 to May 2016, 696 patients were enrolled, but the study was restricted to 649 patients for whom data were available for 12 weeks post-treatment follow-up. The physician in charge gave the patients a full explanation of the study objectives and methods, adverse reactions and risks and countermeasures for them, and protection of private information. Patients who provided consent received treatment with DCV 60 mg once daily and ASV 100 mg twice daily. The duration of treatment was 24 weeks, and patients were followed up for ≥12 weeks after the last treatment dose. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and was approved by the Ethics Committee of each hospital. Written informed consent was obtained from all patients before enrollment.
Hematological, biochemical and virological parameters were determined by the clinical laboratory at each hospital. Serum HCV RNA concentrations were determined by the COBAS TaqMan PCR HCV test (Roche Diagnostics, Tokyo, Japan). SVR was defined as undetectable HCV RNA at week 12 after completion of therapy (SVR12), and rapid virological response (RVR) was defined as undetectable HCV RNA at week 4 of treatment. Genotyping for the IL28B (rs8099917) polymorphisms was performed when practically possible by TaqMan SNP Genotyping Assays (Applied Biosystems, Tokyo, Japan) that used polymerase chain-reactionbased restriction fragment length polymorphism assays. HCV RASs were analyzed by direct sequencing of the HCV NS3 protease and NS5A domains.
Statistical analysis was performed using JMP version 10.0.0 software (SAS Institute, Cary, NC, USA). Differences between categorical variables were analyzed using Fisher’s exact test or χ2-test. Mann–Whitney U test was used for continuous variables. Multivariate analysis was used to identify factors independently associated with achievement of SVR12. The odds ratio (OR) and 95% confidence intervals were also calculated. P values <0.05 were considered to be statistically significant.
Results
Patient characteristics
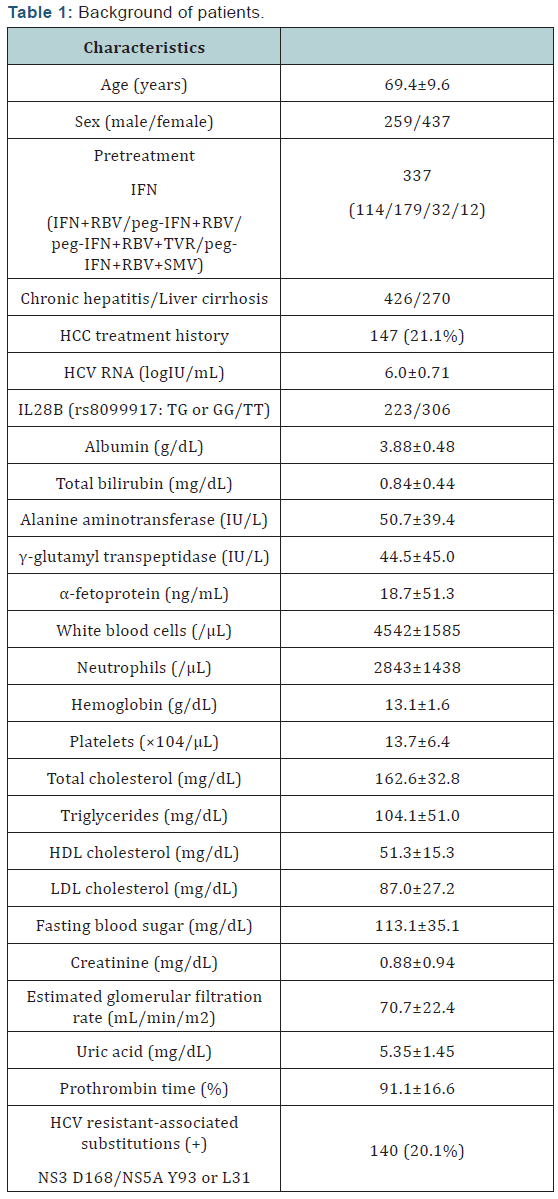
HCV-1 patients with chronic hepatitis or compensated cirrhosis (n=696) were enrolled and started treatment (Table 1). The enrolled population was older (median 70 years) than patients with previous IFN-based therapy (early 60s), reflecting HCV epidemiology in Japan, and predominantly female (63%) [5,40]. All patients were Asian and 39% had advanced liver fibrosis (compensated cirrhosis) and 147 (21%) had prior treatment for HCC. Most of the enrolled patients had genotype 1b infection (only 2 patients had genotype 1a), consistent with the high proportion of this subtype in Japan. About 40% of patients had the intractable IL28B genotype GT/GG (rs8099917), which was higher than the proportion of individuals with IL28B genotype in Japan. This might have resulted from the high number of patients with failure to previous IFN-based treatment. A total of 359 patients were treatment-naïve and 44 were previously exposed to DAAs (32 to TVR and 12 to SMV) with peg-IFN and RBV. Baseline serum albumin and total cholesterol levels, and platelet count were lower, reflecting the older age and advanced liver fibrosis in the enrolled population. A total of 140 patients had HCV with RASs (16 with NS3 D168 and 124 with NS5A Y93 or L31) at baseline.
A total of 649 of the 696 enrolled patients reached follow-up of 12 weeks after treatment. Sixty-nine patients discontinued the study treatment: 29 dropped out because of viral breakthrough, and study drugs were suspended in 40 because of ALT elevation (n=11), onset of HCC (n=9), general fatigue or illness (n=8), exacerbation of hepatic encephalopathy (n=3), skin eruption (n=3), brain infarction (n=1), brain hemorrhage (n=1), and patient request (n=4). All patients remained in the study for assessment of SVR.
Virological response
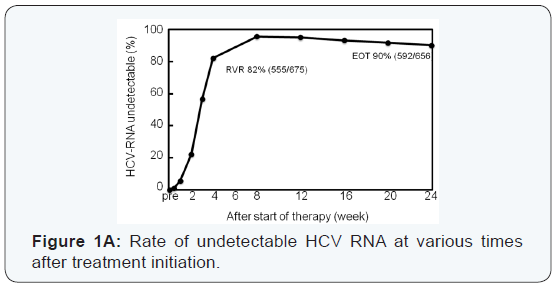
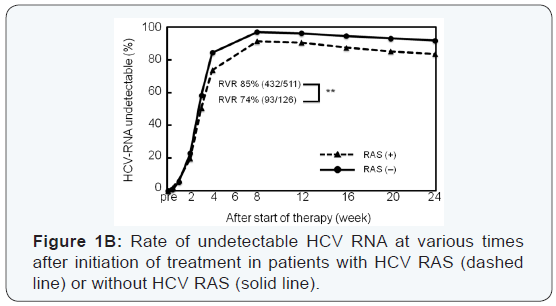
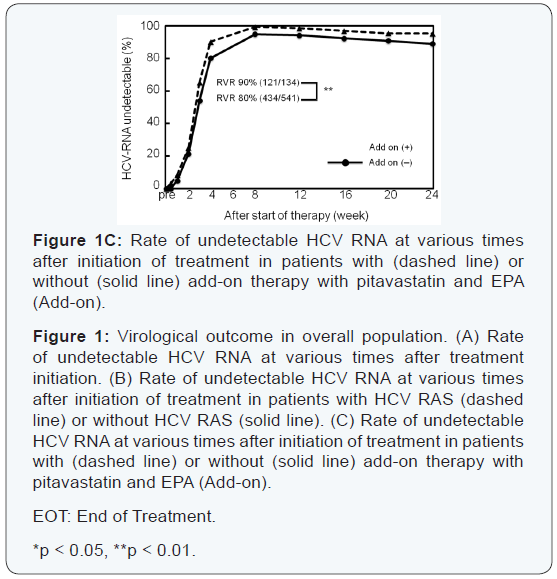
High rates of virological response were obtained at all time points. HCV RNA declined rapidly and was lower than the sensitivity limit in 67% of patients after 2 weeks, and 83% of patients achieved RVR (Figure 1A). Mean reductions of HCV RNA from baseline at 4 weeks after treatment initiation were –5.8 log IU/mL, and the response of HCV was not affected by age, sex, liver fibrosis, or previous treatment response. HCV RNA positivity at 4 weeks was significantly higher in patients with HCV with RAS in NS3 D168, NS5A L31, or NS5A Y93, and RVR rate was significantly higher in patients with add-on lipid modulators, pitavastatin and EPA (Figure 1B, C).
Thirty-eight patients experienced viral breakthrough. The timing of viral breakthrough was spread over each treatment period, and no specific trend was found. Eighteen patients with viral breakthrough had HCV with RAS in NS3 D168, NS5A L31, or NS5A Y93 at baseline, and six patients had prior exposure to the protease inhibitor SMV. Twenty-one patients relapsed: 11 at post-treatment week 4, eight at post-treatment week 12, and two at post-treatment week 24. Ten patients who relapsed had HCV with RASs, but only one patient with a history of SMV treatment had relapse (data not shown).
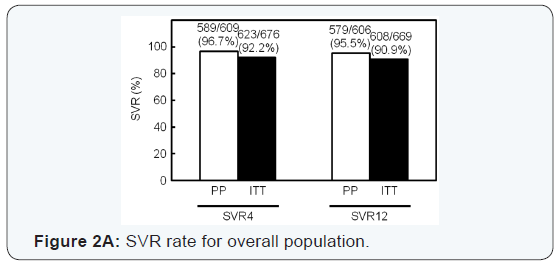
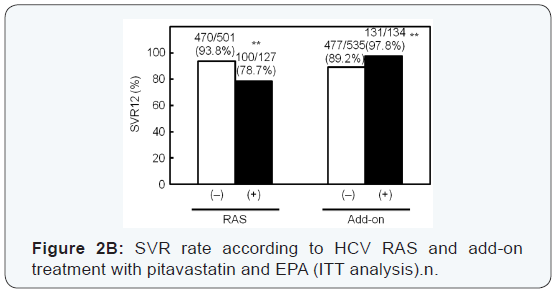
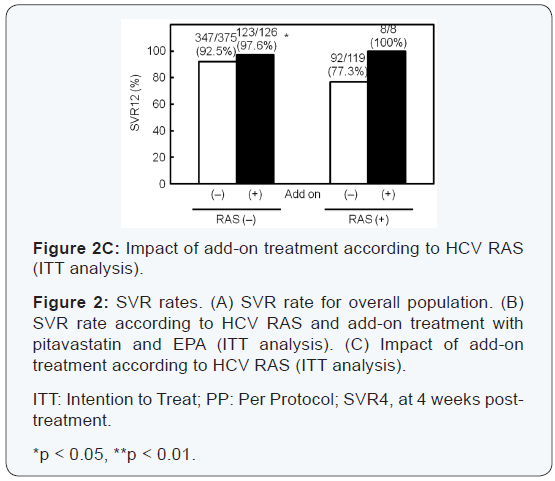
A total of 608 of 669 (91%) enrolled patients achieved SVR12 (Figure 2A). HCV RASs had the largest impact on SVR; 94% of patients with HCV without RASs achieved SVR12, while SVR12 rate was only 79% for patients with HCV with RASs (Figure 2B). Only five of 12 patients (42%) who had prior exposure to SMV achieved SVR12; by contrast, SVR12 rate was high (97%) for patients with a history of TVR treatment. Among patients who had prior exposure to SMV, all five who had HCV with RASs at baseline and two with HCV without RASs failed the treatment. SVR12 rate for patients with pitavastatin and EPA was higher (131/134, 98%) than that for patients with standard treatment (477/535, 89%) (Figure 2B). Add-on treatment with pitavastatin and EPA improved SVR12 rate for patients with HCV with RASs, and all the patients achieved SVR12. SVR rate for the addon group was also significantly higher than in patients in the standard treatment group with HCV without RASs (Figure 2C). SVR12 rate for patients with liver cirrhosis was significantly lower than that of patients with chronic hepatitis; 228/261 (87%) versus 380/408 (93%). Age, sex, or previous treatment response did not affect SVR12 rate. Patients with intractable IL28B TG/GG genotype (rs8099917) showed a poor response at weeks 3 and 4 of treatment; however, SVR12 rate was similar between patients with IL28B TT and TG/GG (data not shown).
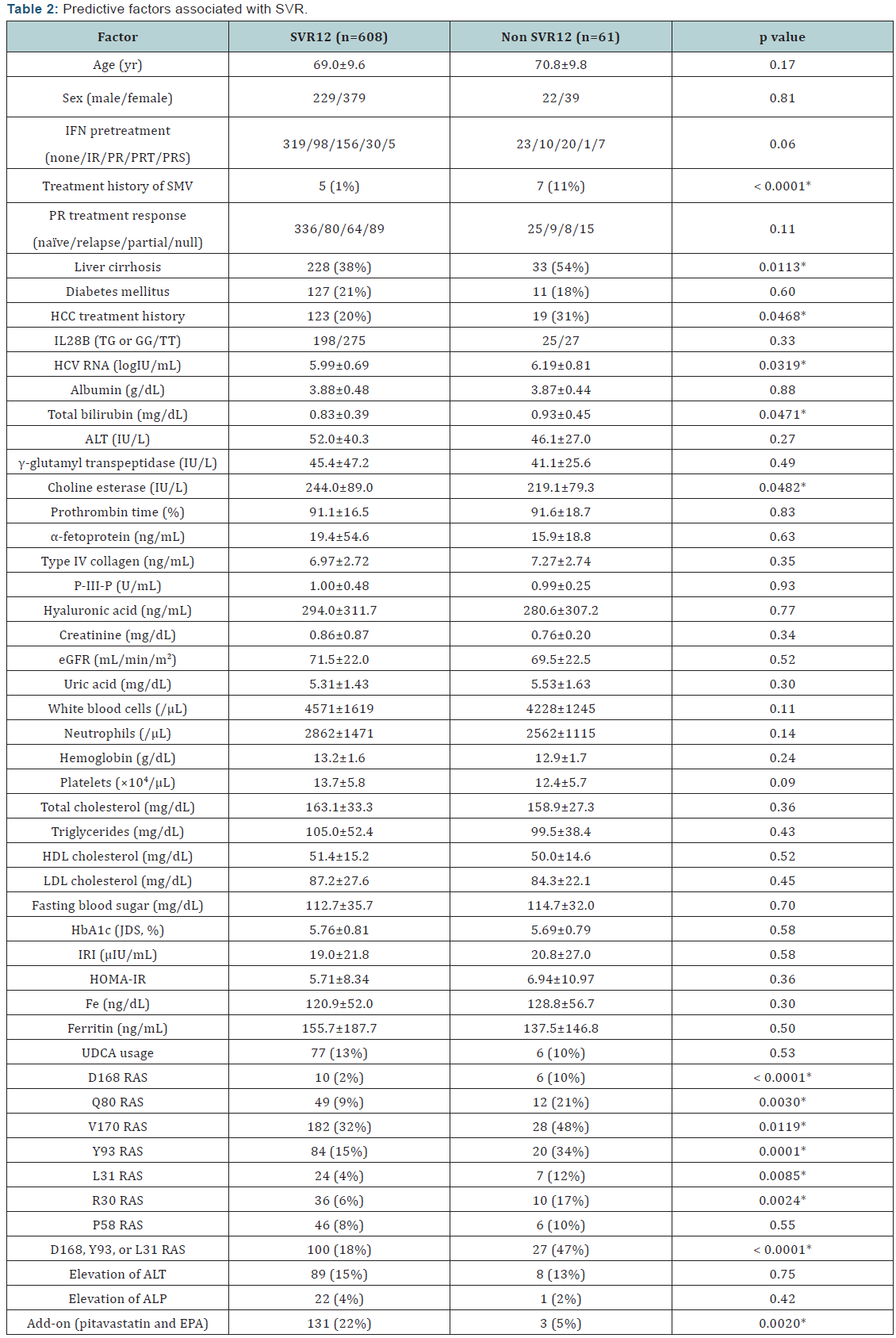
Predictive factors associated with SVR
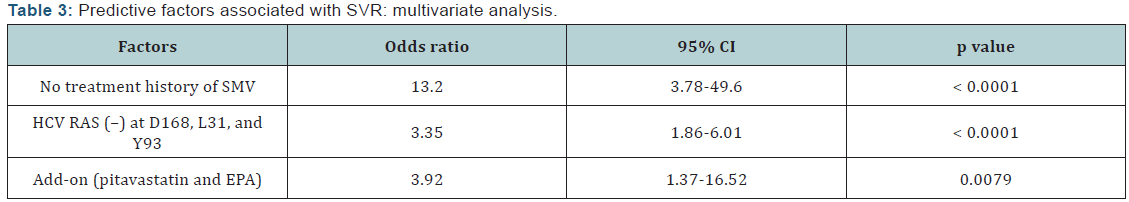
Predictive factors associated with SVR were examined in all patients (Table 2). Univariate analysis identified some parameters that correlated significantly with SVR12: prior exposure to SMV (p<0.0001); liver cirrhosis (p=0.0113); HCV RNA at baseline (p=0.0319); serum total bilirubin (p=0.0471); serum choline esterase (p=0.0482); RAS at NS3 D168 (p<0.0001); RAS at NS3 Q80 (p=0.003); RAS at NS3 V170 (p=0.0119); RAS at NS5A Y93 (p=0.0001); RAS at NS5A L31 (p=0.0085); RAS at NS5A R30 (p=0.0024); RAS at NS3 D168, NS5A L31, or NS5A Y93 (p<0.0001); and add-on therapy (p=0.002). In multivariate logistic regression analysis, significant contributory factors for SVR12 were no prior exposure to SMV (OR 13.2, p<0.0001), no RAS at NS3 D168, NS5A L31, or NS5A Y93 (OR 3.35, p<0.0001), and add-on treatment with pitavastatin and EPA (OR 3.92, p=0.0079) (Table 3).
Adverse events
Adverse events were evaluated according to the Common Terminology Criteria for Adverse Event Version 4.0. The frequently reported adverse events were ALT elevation, alkaline phosphatase (ALP) elevation, pyrexia, headache, malaise, and skin eruption. One hundred patients developed ALT elevation (≥Grade 2), and 24 ALP elevation (≥Grade 2). Pyrexia and headache were Grade 1. The frequencies of adverse events were similar between patients with liver cirrhosis and those with chronic hepatitis, and unaffected by age.
Discussion
In this study, HCV RNA rapidly became undetectable after initiation of all-oral treatment with DCV and ASV, and 82% of patients achieved RVR. A high SVR rate of 90.9% was achieved after 24 weeks all-oral DAA treatment, which is clearly higher than previous IFN-based antiviral treatments [4,5,17-20]. Viral clearance was not affected by age, sex, previous treatment response, or IL28B single nucleotide polymorphisms, which were known to influence the outcome of IFN-based antiviral treatment.
The rate for cessation of DCV and ASV treatment was low (40 cases, 6%) and the severity of adverse events was mild. Frequently reported adverse events were ALT elevation, ALP elevation, pyrexia, headache, malaise, and skin eruption, as published previously [24-29], and the frequency of adverse events was not affected by age or liver fibrosis. Hence, this alloral DAA treatment could be an adequate option for older or cirrhotic patients. The highest complication during DCV and ASV treatment was ALT elevation (100 cases, 14%), and 11 had terminated therapy. Body weight was positively associated with ALT elevation during DCV and ASV combination therapy (data not shown), suggesting that serum and hepatic concentrations of ASV are involved in liver damage during therapy. Likewise, patients with liver cirrhosis had a significantly higher risk of ALP elevation (data not shown). DCV and ASV are mainly metabolized in the liver [30], and it is possible that metabolism of DCV and/ or ASV in hepatocytes is involved in ALP elevation during DAA treatment.
HCV with RASs at NS3 D168, NS5A L31, or NS5A Y93 were detected in 131 patients in our study, and SVR rate for patients with HCV with RASs was significantly lower than in those with wild-type virus (Figure 2). However, the SVR rate for patients with HCV with RASs was clearly higher than in the previous study [29]. This might be partly because the physician tried to avoid discontinuation of the treatment when encountering adverse events. By sequencing the HCV RASs in patients who failed the treatment, multiple HCV RASs were detected in most patients with virological failure (data not shown), as previously reported [26,29]. Furthermore, no RAS at NS3 D168, NS5A L31, or NS5A Y93 before treatment was selected as one of the independent significant contributory factors for SVR in multivariate logistic regression analysis. Recently, fixed-dose treatment with ledipasvir and sofosbuvir in patients with HCV genotype 1b achieved a higher SVR rate than DCV and ASV treatment, even for patients with HCV with RASs [31]. Examination for pretreatment RAS and selection of patients might be important for future adoption of treatment with DCV and ASV.
Prior exposure to SMV was also involved in response to DCV and ASV treatment. SMV and ASV are both NS3/4 protease inhibitors of the second generation and have similar therapeutic and resistance profiles [23]. Therefore, even patients with HCV without RASs who had prior SMV treatment might be predisposed to acquire HCV with RASs for ASV. Thus, we need to take history of treatment with the same DAA or ones with identical drug potency into consideration for future DAA treatment.
In the present study, patients with advanced fibrosis achieved a significantly lower SVR rate compared with those with chronic hepatitis; however, this association disappeared in multivariate analysis (Tables 2 & 3). Thus, liver fibrosis could affect the outcome of DCV and ASV treatment for the following reasons. (1) Drug delivery: patients with liver cirrhosis had portosystemic or intrahepatic shunt and drug delivery could be inhibited and/or drug concentration reduced in some part of the liver. (2) Immune response: immunological disorder was observed in patients with advanced liver fibrosis. Some patients with advanced liver fibrosis with esophageal varices did not achieve SVR, and insufficient drug delivery into the cirrhotic liver could affect viral clearance. Furthermore, patients with intractable IL28B genotype showed a poor response to treatment with DCV and ASV at weeks 3 and 4, suggesting that immune response might have some impact on viral clearance during DCV and ASV treatment.
Previous studies on hepatic lipid metabolism have shown that, in the liver with HCV infection, synthesis of cholesterol and fatty acids is still activated, regardless of over-accumulation of lipids [32-35]. Suppressive effects against HCV replication by statins and EPA, and their synergistic action with IFN have already been demonstrated in some HCV replicon systems [36- 39,41-46]. PUFAs including EPA inhibit HCV replication, which may be independent of the regulating lipogenesis [38,39]. In this study, patients with add-on therapy of pitavastatin and EPA showed a significantly higher biological response rate to DCV and ASV compared with those without add-on treatment (Figure 2). Negative modulation of lipid synthesis by pitavastatin and EPA, activation of the antiviral host response to HCV infection by pitavastatin, repression of HCV entry/infection through suppression of low-density lipoproteins receptor expression by EPA is thought to be involved in viral clearance during peg-IFN/ RBV treatment [46]. The mechanism of action is independent of the antiviral effect of DAAs [30]. Therefore, addition of pitavastatin and EPA could be useful to enhance the antiviral effect on HCV infection via different mechanisms during future DAA treatment. For reliable assessment, further accumulation of clinical data is necessary for patients treated with this add-on therapy.
Response of HCV RNA to treatment with DCV and ASV was sufficiently favorable, even for women, older patients, patients with liver cirrhosis or patients with intractable IL-28B polymorphisms. HCV RASs and history of treatment with SMV could be involved in antiviral host response and viral clearance. Moreover, the lipid modulators, pitavastatin and EPA, enhanced the efficacy of all-oral DCV and ASV combination therapy through synergistic antiviral effect. It is possible that addition of pitavastatin and EPA is effective for patients with treatmentresistant HCV, which may increase SVR rates in patients treated with DAAs in the future.
Acknowledgment
Supported in part by Bristol–Myers Squibb and the Japan Agency for Medical Research and Development, AMED (grant number: 15fk0210017h003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding was received for this study.
Disclosure Statement
Makoto Nakamuta received research funding from Bristol– Myers Squibb. All other authors have no conflicts of interest to declare. All procedures followed were in accordance with the ethical standards of the committees responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or equivalent was obtained from all patients for inclusion in the study.
References
- Alter HJ (2005) HCV natural history: the retrospective and prospective in perspective. J Hepatol 43(4): 550-552.
- Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, et al. (2006) The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med 144(10): 705-714.
- Tanaka J, Koyama T, Mizui M, Uchida S, Katayama K, et al. (2011) Total numbers of undiagnosed cARGHiers of hepatitis C and B viruses in Japan estimated by age- and area- specific prevalence on national scale. Intervirology 54(4): 185-195.
- Aghemo A, Rumi MG, Colombo M (2009) Pegylated IFN-α2a and ribavirin in the treatment of hepatitis C. Expert Rev Anti Infect Ther 7(8): 925-935.
- Kumada T, Toyoda H, Honda T, Kuzuya T, Katano Y, et al. (2006) Treatment of chronic hepatitis C with interferon alone or combined with ribavirin in Japan. Intervirology 49(1-2): 112-118.
- Shiffman ML (2002) Retreatment of patients with chronic hepatitis C. Hepatology 36(5 Supp 1): S128-134.
- Backus LI, Boothroyd DB, Phillips BR, Mole LA (2007) Prediction of response of US veterans to treatment for the hepatitis C virus. Hepatology 46(1): 37-47.
- Kanwal F, Hoang T, Spiegel BM, Elsen S, Dominitz JA, et al. (2007) Predictions of treatment in patients with chronic hepatitis C infection – role of patient versus nonpatient factors. Hepatology 46(6): 1741- 1749.
- Bortoletto G, Scribano L, Realdon S, Marcolongo M, Mirandola S, et al. (2010) Hyperinsulinemia reduces the 24-h virological response to PEG-interferon therapy in patients with chronic hepatitis C and insulin resistance. J Viral Hepat 17(7): 475-480.
- Suppiah V, Moldovan M, Ahlenstiel G, Berg T, Weltman M, et al. (2009) IL28B is associated with response to chronic hepatitis C interferonalpha and ribavirin therapy. Nat Genet 41(10): 1100-1104.
- Tanaka Y, Nishida N, Sugiyama M, Kurosaki M, Matsuura K, et al. (2009) Genome-wide association of IL28B with response to pegylated interferon-alpha and ribavirin therapy for chronic hepatitis C. Nat Genet 41(10): 1105-1109.
- Ge D, Fellay J, Thompson AJ, Simon JS, Shianna KV, et al. (2009) Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature 461(7262): 399-401.
- Hayes CN, Kobayashi M, Akuta N, Suzuki F, Kumada H, et al. (2011) HCV substitutions and IL28B polymorphisms on outcome of peg-interferon plus ribavirin combination therapy. Gut 60(2): 261-267.
- Akuta N, Suzuki F, Sezaki H, Suzuki F, Hosaka T, et al. (2005) Association of amino acid substitution pattern in core protein of hepatitis C virus genotype 1b high viral load and non-virological response to interferonribavirin combination therapy. Intervirology 48(6): 372-380.
- Akuta N, Suzuki F, Kawamura Y, Yatsuji H, Sezaki H, et al. (2007) Prediction of response to pegylated interferon and ribavirin in hepatitis C by polymorphisms in the viral core protein and very early dynamics of viremia. Intervirology 50(5): 361-368.
- El-Shamy A, Kim SR, Ide YH, Sasase N, Imoto S, et al. (2012) Polymorphism of hepatitis C virus non-structural protein 5A and core protein and clinical outcome of pegylated-interferon/ribavirin combination therapy. Intervirology 55(1): 1-11.
- Jacobson IM, McHutchison JG, Dusheiko G, Di Bisceglie AM, Reddy KR, et al. (2011) Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med 364(25): 2405-2416.
- Kumada H, Toyota J, Okanoue T, Chayama K, Tsubouchi H, et al. (2012) Telaprevir with peginterferon and ribavirin for treatment-naïve patients chronically infected with HCV of genotype 1 in Japan. J Hepatol 56(1): 78-84.
- Fried MW, Buti M, Dore GJ, Flisiak R, Ferenci P, et al. (2013) Once-daily simeprevir (TMC435) with peginterferon and ribavirin in treatmentnaïve genotype 1 hepatitis C: the randomized PILLAR study. Hepatology 58(6): 1918-1929.
- Hayashi N, Nakamuta M, Takehara T, Kumada H, Takase A, et al. (2016) Vaniprevir plus peginterferon alfa-2b and ribavirin in treatmentnaive Japanese patients with hepatitis C virus genotype 1 infection: a randomized phase III studies. J Gastroenterol 51(4): 390-403.
- Mechie NC, Röver C, Cameron S, Amanzada A (2014) Predictability of IL-28B-polymorphism on protease-inhibitor-based triple-therapy in chronic HCV-genotype-1 patients: A meta-analysis. World J Hepatol 6(10): 759-765.
- Fridell RA, Qiu D, Wang C, Valera L, Gao M (2010) Resistance analysis of the hepatitis C virus NS5A inhibitor BMS-790052 in an in vitro replicon system. Antimicrob Agents Chemother 54(9): 3641-3650.
- McPhee F, Friborg J, Levine S, Chen C, Falk P, et al. (2012) Resistance analysis of the hepatitis C virus NS3 protease inhibitor asunaprevir. Antimicrob Agents Chemother 56(7): 3670-3681.
- Chayama K, Takahashi S, Toyota J, Karino Y, Ikeda K, et al. (2012) Dual therapy with the NS5A inhibitor BMS-790052 and the NS3 protease inhibitor BMS-650032 in HCV genotype 1b-infected null responders. Hepatology 55(3): 742-748.
- Lok AS, Gardiner DF, Lawitz E, Martorell C, Everson GT, et al. (2012) Preliminary study of two antiviral agents for hepatitis C genotype 1. N Engl J Med 366(3): 216-224.
- Suzuki Y, Ikeda K, Suzuki F, Toyota J, Chayama K, et al. (2013) Dual oral therapy with daclatasvir and asunaprevir for patients with HCV genotype 1b infection and limited treatment options. J Hepatol 58(4): 655-662.
- Lok AS, Gardiner DF, Hézode C, Lawitz EJ, Bourlière M, et al. (2014) Randomized trial of daclatasvir and asunaprevir with or without PegIFN/RBV for hepatitis C virus genotype 1 null responders. J Hepatol 60(3): 490-499.
- Manns M, Pol S, Jacobsen IM, Marcellin P, Gordon SC, et al. (2014) Alloral daclatasvir plus asunaprevir for hepatitis C virus genotype 1b: a multinational, phase 3, multicohort study. Lancet 384(9954): 1597- 1605.
- Kumada H, Suzuki Y, Ikeda K, Toyota J, Karino Y, et al. (2014) Daclatasvir plus asunaprevir for chronic HCV genotype 1b infection. Hepatology 59(6): 2083-2091.
- Hill L (2015) Hepatitis C virus direct-acting antiviral drug interactions and use in renal and hepatic impairment. Top Antivir Med 23(2): 92- 96.
- Reddy KR, Bourlière M, Sulkowski M, Omata M, Zeuzem S, et al. (2015) Ledipasvir and sofosbuvir in patients with genotype a hepatitis C virus infection and compensated cirrhosis: an integrated safety and efficacy analysis. Hepatology 62(1): 79-86.
- Nakamuta M, Fujino T, Yada R, Aoyagi Y, Yasutake K, et al. (2011) Expression profiles of genes associated with viral entry in HCV-infected human liver. J Med Virol 83(5): 921-927.
- Fujino T, Nakamuta M, Yada R, Aoyagi Y, Yasutake K, et al. (2010) Expression profile of lipid metabolism-associated genes in HCVinfected human liver. Hepatol Res 40(9): 923-929.
- Nakamuta M, Yada R, Fujino T, Yada M, Higuchi N, et al. (2009) Changes in the expression of cholesterol metabolism-associated genes in the HCV-infected liver: a novel target for therapy? Int J Mol Med 24(6): 825-828.
- Kohjima M, Enjoji M, Higuchi N, Kato M, Kotoh K, et al. (2009) The effects of unsaturated fatty acids on lipid metabolism in HepG2 cells. In Vitro Cell Dev Biol Anim 45(1-2): 6-9.
- Simons K, Ehehalt R (2002) Cholesterol, lipid lafts, and disease. J Clin Invest 110(5): 597-603.
- Kushner DB, Lindenbach BD, Grdzelishvili VZ, Noueiry AO, Paul SM, et al. (2003) Systematic, genome-wide identification of host genes affecting replication of a positive-strand RNA virus. Proc Natl Acad Sci USA 100(26): 15764-15769.
- Leu GZ, Lin TY, Hsu JTA (2004) Anti-HCV activities of selective polyunsaturated fatty acids. Biochem Biophys Res Commun 318(1): 275-280.
- Kapadia SB, Chisari FV (2005) Hepatitis C virus RNA replication is regulated by host geranylgeranylation and fatty acids. Proc Natl Acad Sci USA 102(7): 2561-2566.
- Ogawa E, Furusyo N, Kajiwara E, Nomura H, Kawano A, et al. (2015) Comparative effectiveness and safety of triple therapy with simeprevir or telaprevir for non-cirrhotic patients with chronic hepatitis C virus genotype 1b infection. J Gastroenterol Hepatol 30(12): 1759-1767.
- Huang H, Chen Y, Ye J (2007) Inhibition of hepatitis C virus replication by peroxidation of arachidonate and restoration by vitamin E. Proc Natl Acad Sci USA 104(47): 18666-18670.
- Ikeda M, Abe K, Yamada M, Dansako H, Naka K, et al. (2006) Different anti-HCV profiles of statins and their potential for combination therapy with interferon. Hepatology 44(1): 117-125.
- Ikeda M, Kato N (2007) Life style-related diseases of the digestive system: cell culture system for the screening of anti-hepatitis C virus (HCV) reagents: suppression of HCV replication by statins and synergistic action with interferon. J Pharmacol Sci 105(2): 145-150.
- Ye J, Wang C, Sumpter R, Brown MS, Goldstein JL, et al. (2003) Disruption of hepatitis C virus replication through inhibition of host protein geranylgeranylation. Proc Natl Acad Sci USA 100(26): 15865- 15870.
- Wang C, Gale M, Keller BC, Huang H, Brown MS, et al. (2005) Identification of FBL2 as a geranylgeranylated cellular protein required for hepatitis C virus RNA replication. Mol Cell 18(4): 425-434.
- Kohjima M, Enjoji M, Yoshimoto T, Yada R, Fujino T, et al. (2013) Add-on therapy of pitavastatin and eicosapentaenoic acid improves outcome of peginterferon plus ribavirin treatment for chronic hepatitis C. J Med Virol 85(2): 250-260.






























