Cytomegalovirus causing Haemorrhagic Colitis Requiring Hemicolectomy in a Kidney Transplant Recipient
Irtaqa Ali Hasnain1*, Mujtaba Ali Hasnain2 and Samrah Mujtaba2
1Bahria Town Hospital, Pakistan
2Saint Barnabas Medical Center, USA
Submission: August 28, 2016; Published: September 27, 2016
*Corresponding author: Irtaqa Ali Hasnain, Bahria Town Hospital, Lahore, Pakistan.
How to cite this article: Irtaqa A H, Mujtaba A H, Samrah M. Cytomegalovirus causing Haemorrhagic Colitis Requiring Hemicolectomy in a Kidney Transplant Recipient. Adv Res Gastroentero Hepatol. 2016; 2(1): 555577. DOI: 10.19080/ARGH.2016.02.555577
Abstract
71 year old lady with medical history of end stage renal disease due to hypertension received a living related kidney transplant. She received thymoglobulin induction at dose of 6mg/kg and her maintainence immunosuppression consisted of tacrolimus, prednisone and mycophenolic acid. She received valganciclovir for 3 months for CMV prophylaxis as both donor and recipient were positive for serum CMV IgG antibodies. She presented with melena and fevers 4 months post transplant. She developed hematochezia and went into hemorrhagic shock immediately after presentation and required multiple transfusions. Bleeding scitinography showed active bleeding in the region of the distal small bowel. Coiled embolization failed to control the bleeding and she underwent emergent right sided hemicolectomy. Her serum CMV virus result was 3,900,000 copies/ml. She was treated with valganciclovir and mycophenolic acid was stopped. Pathology report of the resected segment of colon showed severe ulceration of entire colon with cells containing viral cytopathic effects, confirmed by immunohistochemistry, as CMV.
Keywords: Kidney; Cytomegalovirus
Introduction
Cytomegalovirus (CMV) is one of the most common viral infections in post-transplant immunocompromised patients. It can present in a wide variety of ways including colitis, gastritis, hepatitis and leucopenia. We present a novel case of severe hemorrhagic colitis due to CMV infection.
Discussion
What is CMV
Cytomegalovirus is a common herpes virus [1]. CMV is the most common and single most important viral infection in solid organ transplant recipients. CMV infection usually develops during the first few months after transplantation and is associated with clinical infectious disease (e.g, fever, pneumonia, GI ulcers, hepatitis) and acute and/or chronic graft injury and dysfunction. Many people do not know they have it, because they may have no symptoms. But the virus, which remains dormant in the body, can cause complications during pregnancy and for people with a weakened immune system. Also known as HCMV, CMV, or Human Herpes virus 5 (HHV-5), cytomegalovirus is the virus most commonly transmitted to a developing fetus.
Transmission
The virus can spread in a number of ways [2]:.
Touching your eyes or the inside of your nose or mouth after coming into contact with the body fluids of an infected person. This is the most common way CMV is spread because it’s absorbed through the mucous membranes.
Through sexual contact with an infected person.
Through the breast milk of an infected mother [3].
Through organ transplantation or blood transfusions.
Through the placenta, from an infected mother to her unborn child, or during birth [4].
Pathogenesis
CMV has the potential to spread in the bloodstream to all organs, but only produces overt disease if the viral load increases to high levels. This is normally prevented by a robust immune response, so that the infected individual usually remains asymptomatic. However, this benefit comes at the cost of committing more and more immunological resources to controlling CMV with time, so that the overall function of the immune system is impaired [5].
The CMV genome is composed of lineal, double-stranded DNA, surrounded by a protein lining, called matrix, which contains phosphoproteins (pp65, pp150, etc.) that are highly immunogenic and capable of deregulating the cellular cycle of the host cell. This lining is surrounded by glycoproteins (gB, gN, gO, gH, gM, gL) necessary for the virus infectivity: entrance to the host cell, cell-to-cell dissemination, and maturing.
The fusion of the virus with the cell is mediated by the viral glycoprotein gB. The fusion is followed by the entrance of the nucleocapsid and the lining proteins to the host cell cytoplasm; the nuclei are translocated rapidly and pp65 antigen, a marker of infection, is detected in the serum in less than an hour. The main reservoirs of CMV are the fibroblasts, myeloid cells, and endothelial cells. The infection of endothelial cells and macrophages plays an important role in the latency, and this seems to be a critical point in the maintenance of CMV in the host.
The start of the replication takes about 12-24 hours after the infection of the cell, and the cytopathic effect in the viral culture could be seen after 7-14 days. As with other herpes viruses, CMV invades the host cell, inhibits protein synthesis, and liberates viral DNA to the nuclei, where the replication starts immediately. A strategy that it shares with other herpes viruses is the ability of stopping the immune response of the host by inhibiting RNA formation, blocking the presentation of antigenic peptides of the cell surface, and blocking apoptosis. These mechanisms prompt to a latent infection that may be reactivated in transplant recipients
Immunologic mechanism of rejection
The immune recognition of foreign antigens in the graft is mediated by MHC class I and II. Class I molecules are expressed in all nucleated cells and platelets, while class II are expressed by B lymphocytes, cells of the monocyte-macrophage system and dendritic cells. The T-cells and non lymphoid cells show class II proteins only when they are activated by cytokines. Rejection depends on the coordinated activation of T-cells and antigenpresenting cells [6].
For example, in kidney rejection, tubulitis is one of the major diagnostic criteria and consists of the invasion of the tubular epithelium by lymphoid cells. The CD8 lymphocytes are the cells mainly involved in tubulitis development. These cells are attracted by the β-chemokine secretion, especially, MCP-1 and MCP-1β (monocyte chemotactic peptides). Also participating are macrophage inflammatory protein MIP-1α and RANTES (activation regulated peptides expressed in T-cells and possibly secreted).
Something similar occurs in heart transplantation. The expression of self antigens to avoid being recognized and damaged is a constant mechanism.
Treatment
There’s no cure for CMV, and treatment for the virus generally isn’t necessary or recommended for healthy children and adults.
Newborns and people with compromised immune systems i.e. Patients after kidney transplantation, however, need treatment when they’re having symptoms of CMV infection, such as pneumonia. The kind of treatment depends on the symptoms and their severity.
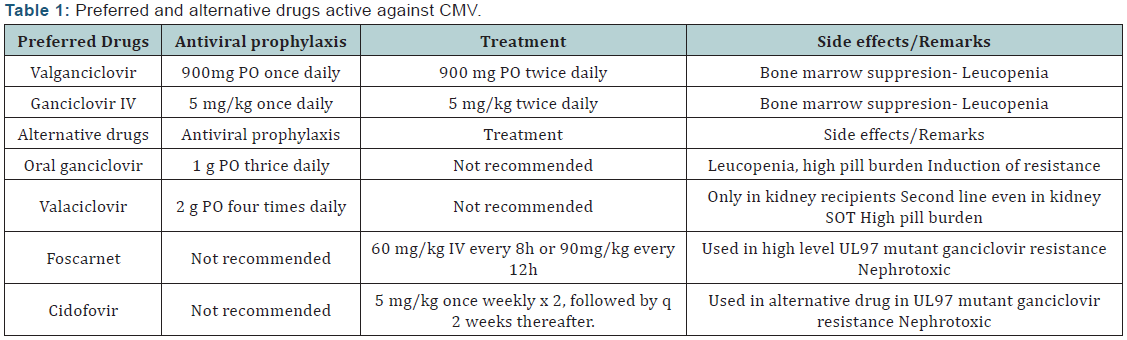
Treatment of CMV in solid organ transplant [7] recipients reduces the risk of allograft injury and death [. The two main drugs used for treating CMV disease are intravenous (IV) ganciclovir (5-mg/kg every 12 hours) and oral valganciclovir (900-mg twice daily). Oral valganciclovir achieves comparable blood levels to IV ganciclovir and is recommended for the treatment of mild to moderate CMV disease in solid organ transplant recipients.
In a study of 321 adult solid organ transplant recipients with CMV disease, the clinical and virologic outcomes were not significantly different between those patients who received oral valganciclovir or IV ganciclovir. The rate of viremia eradication for valganciclovir group and IV ganciclovir group were comparable - 45.1% versus 48.4% at day 21, and 67.1% versus 70.1% at day 49, respectively. The median time of viremia eradication (21 versus 19 days), side effect profiles, and treatment outcomes were also comparable between the two groups .
IV ganciclovir is preferred drug for treatment of severe or life-threatening CMV disease or in those with questionable gastrointestinal absorption. IV ganciclovir is also recommended for those with very high viral load. Oral ganciclovir should never be used in the treatment of CMV disease because of poor oralbioavailability leading to sub-therapeutic blood levels.
In addition to the antiviral therapy, it is strongly emphasized that a cautious reduction in immunosuppression will help in the clearance of infection. CMV occurs as a result of an over-immunocompromised state, hence, the reduction in immunosuppression will allow for the recovery or the generation of CMV-specific immunity that will allow longer-lasting control of the virus infection.
The duration of antiviral therapy should be individualized and be guided by resolution of clinical symptoms and viral load monitoring. Viral load kinetics that have shown to help predict clinical response to antiviral therapy include a lower pretreatment viral load, a faster rate of viral load decline in response to therapy, and viral suppression at the end of treatment. In a recent study which used the WHO international standard for reporting, patients with a pretreatment CMV DNA < 18,200 IU/ mL were more likely to have CMV disease resolution. Moreover CMV suppression < 137 IU/mL was predictive of clinical response to therapy (Table 1).
Prevention
Careful hygiene is the best prevention against CMV. Health care workers have the greatest chances of exposure, but because of precautions used in the health care setting, their risk of acquiring the disease is low.
CMV in solid organ transplantation (SOT)
While most infections in immunocompetent individuals are benign and self-limited, CMV is an important cause of morbidity and mortality in individuals with underdeveloped or compromised immune function, including transplant recipients. Despite significant advances in its diagnosis and therapy, CMV continues to have a major impact on patient and allograft survival among solid organ transplant (SOT) recipients through a variety of direct and indirect effects.
Advances in the field of CMV and solid organ transplantation will be facilitated by the development of [8] optimized threshold for viral diagnosis, [9] effective vaccines for prevention, [10] diagnostic assays to stratify risk of late onset CMV disease by immunological monitoring, and newer antiviral agents with unique mechanisms of action and ideally with much less toxicity.
Conclusion
Gastrointestinal CMV disease is an increasingly recognized clinical problem in immunocompromised patients [11]. Its presentation can be very mild diARGHhea, nausea and vomiting which is common, to very severe colitis which is rare. Our patient developed hemorrhagic shock due to severe colitis and ultimately required hemicolectomy [11a-d]. If kidney transplant recipient presents with a gastrointestinal bleed, CMV disease should be considered immediately. Timely diagnosis and treatment is extremely important as it can have fatal consequences.
References
- Christian Nordqvist (2016) What is Cytomegalovirus? Reviewed by University of Illinois-Chicago, School of Medicine.
- Cytomegalovirus (CMV) and congenital CMV infection: Transmission (2013) Centers for Disease Control and Prevention.
- Sheffield JS (2013) Cytomegalovirus infection in pregnancy.
- Demmler HARGHison GJ (2013) Cytomegalovirus infection and disease in newborns, infants, children and adolescents.
- Griffiths P, Baraniak I, Reeves M (2015) The pathogenesis of human cytomegalovirus. J Pathol 235(2): 288-297.
- Poornima Ramanan, Raymund R Razonable (2013) Cytomegalovirus Infections in Solid Organ Transplantation: A Review. Infect Chemother 45(3): 260-271.
- Friel TJ (2013) Epidemiology, clinical manifestations and treatment of cytomegalovirus infection in immunocompetent hosts.
- Cytomegalovirus (CMV) and congenital CMV infection: Overview (2013) Centers for Disease Control and Prevention.
- Caliendo AM (2013) Approach to the diagnosis of cytomegalovirus infection. Centers for Disease Control and Prevention.
- Cytomegalovirus (CMV) and congenital CMV infection: Prevention (2013) Centers for Disease Control and Prevention.
- Neurological consequences of cytomegalovirus infection information page (2013) National Institute of Neurological Disorders and Stroke.
- CDC (2016) Cytomegalovirus (CMV) and congenital CMV infection.
- CDC (2016) Helping children with congenital CMV.
- Mayo Clinic Staff (2014) Cytomegalovirus (CMV) infection: Symptoms.
- National CMV Foundation. (N.D) Congenital CMV outcomes.






























