Ogilvie’s Syndrome Complicating a Hemorrhagic Stroke of Brainstem
Hassan Baallal*, Cherkaoui Mandour, Brahim Eljebbouri, Abad cherif El asri, Naima Oukacha, Ali akhaddar and Miloud Gazzaz Brahim El mostarchid
Department of Neurosurgery, University of King Mohammed V Souissi, Morocco
Submission: May 11, 2016; Published: May 24, 2016
*Corresponding author: Hassan Baallal, Department of Neurosurgery, Mohammed V Military Teaching Hospital, University of King Mohammed V Souissi, Rabat, Morocco, Tel: 212661295918; Email :baallalnch@gmail.com
How to cite this article: Hassan B, Cherkaoui M, Brahim E, Abad cherif E, Naima O, et al. Ogilvie’s Syndrome Complicating a Hemorrhagic Stroke of Brainstem. Adv Res Gastroentero Hepatol. 2016; 1(5): 555572. DOI: 10.19080/ARGH.2016.01.555572
Abstract
Ogilvie first described Ogilvie’s syndrome in 1948. This entity is also known as paralytic ileus of the colon, adynamic ileus of the colon, neurological disease causing damage to the central nervous system was identified as an important independent risk factor we reported a 52-year-old Moroccan man from, without history, one after his admission for hemorrhagic stroke of brain stem. He developed abdominal discomfort. Plain abdominal radiography showed diffuse bowel loop dilation and computed tomography showed marked bowel loop dilation and colonic gas. We diagnosed acute pseudo-obstruction of the colon (Ogilvie syndrome) and we decided to use colonoscopic decompression followed by Intravenous neostigmine was given under cardiac monitorization, with good Results.
Keywords: Ogilvie’s syndrome; Brainstem: Hemorrhagic stroke
Introduction
Acute colonic pseudo-obstruction (ACPO) was first described by Sir Heneage Ogilvie [1] who described two patients with colonic pseudo-obstruction resulting from malignant infiltration of the celiac plexus and attributed the syndrome to sympathetic deprivation. It is characterized by a disorder in gastrointestinal motility by marked dilatation of the colon in the absence of mechanical obstruction [2] neurological disease causing damage to the central nervous system was identified as an important independent risk factor [3] there is only a few cases of Ogilvie’s syndrome caused by hemorrhagic stroke of brain stem, we reported a new observation.
Case Report
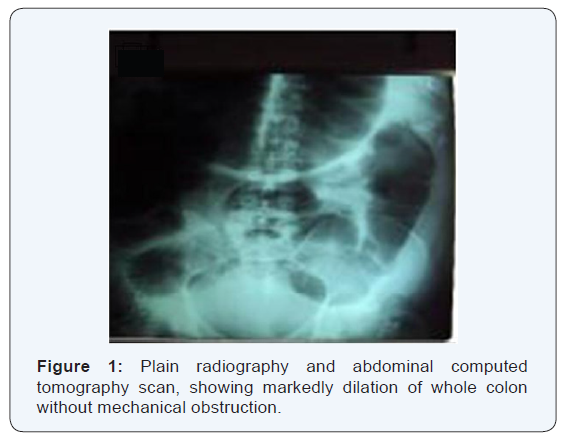
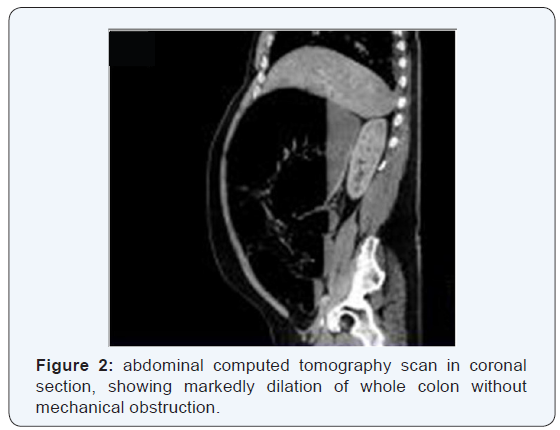
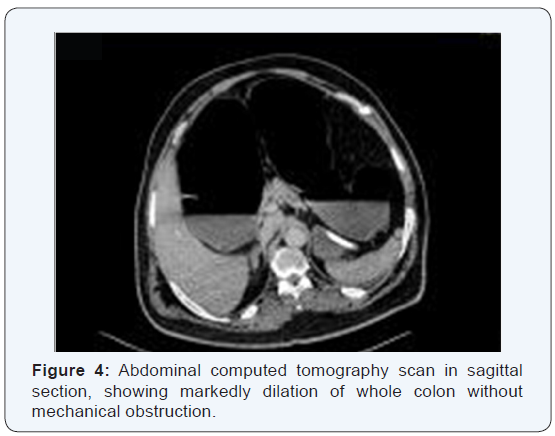
A 52-year-old Moroccan man from, without history admitted to our service for intracranial hypertension syndrome. The clinical examination revealed a cerebellar syndrome. CT scan and MRI angiography showed a hemorrhagic stroke of brain stem without vascular anomaly. One day later He developed abdominal discomfort. On examination, he had a distended abdomen, diffuse tenderness without rebound pain and reduced bowel sounds, but no abdominal mass or peritoneal signs. The patient had no history of metabolic, cardiovascular or pulmonary disease, abdominal or pelvic operations, abdominal cancer, intra-abdominal inflammation or abdominal trauma.He did not take other concomitant medication. He was afebrile, and results of blood tests were unremarkable. Plain abdominal radiography showed diffuse bowel loop dilation (Figure 1), and computed tomography showed marked bowel loop dilation and colonic gas, without obstructive masses or ischemic bowel lesions (Figures 2-4). We diagnosed acute pseudo-obstruction of the colon (Ogilvie syndrome). Nasogastric decompression and discontinuation of oral intake did not relieve our patient’s abdominal pain.

He developed dyspnea because of persistent abdominal distention, and we decided to use colonoscopic decompression followed by. Intravenous neostigmine was given under cardiac monitorization. Two hours later, he had profuse rectal gas and feces excretion. Her complaints improved abruptly. He was symptom-free for 9 days and was discharged on the 15th day.
Discussion
Ogilvie first described Ogilvie’s syndrome in 1948. This entity is also known as paralytic ileus of the colon, adynamic ileus of the colon, or false colonic obstruction. Dudley et al. used the term pseudo-obstruction to describe the clinical appearance of a mechanical obstruction with no evidence of organic disease during laparotomy. Cerebral palsy has been shown to be associated with a high rate of colonic dysmotility [4]. In a study by Johanson et al. [3], neurological disease causing damage to the central nervous system was identified as an important independent risk factor. These factors could predispose these patients to development of ACPO. Colonic it may occur in any patient population, but has a higher predilection for males in the sixth decade [5,6].
The pathogenesis is not fully understood, although it is thought to be an imbalance between inhibitory sympathetic and stimulatory parasympathetic innervations [5,7] On the basis of their experience, some authors affirmed that this syndrome is caused by the inhibition of gastrointestinal hormones that, under the control of neurohypophysis, contribute to colon motility. This supposition is backed up by the fact that medical treatment with somatostatin or octreotide leads to resolution of the disorder, it is known that the autonomic nervous system is the control center for bowel function. The parasympathetic system innervates the smooth muscle to induce peristalsis, thereby inducing normal defecation. Disruption of the parasympathetic system or innervations of the sympathetic system will disrupt normal bowel function. There are many conditions and interventions that have been shown to be associated with bowel dysmotility resulting in ACPO. The differential diagnoses for this condition should also include mechanical bowel obstruction, toxic megacolon, and severe constipation with fecal impaction. In the case described above, the patient’s only significant risk factors for developing ACPO were his hemorrhagic stroke of brain stem. Ogilvie’s syndrome has been reported as a complication Parkinson’s disease, multiple sclerosis, stroke, meningitis, meningioma, and Guillain–BARGHe´ syndrome have been associated with this syndrome [8].
Ischemia or perforation is the feared complication of ACPO; spontaneous perforation has been reported in 3% to 15% of patients with a mortality rate of 50% or higher [9] Depending on the severity of the underlying illness, the overall mortality may be as high as 25% to 31% [10]. Abdominal x-ray plays a crucial role in the diagnosis and management of ACPO. It shows a massively dilated colon with minimal or no distention of the small intestine [5] Although CT with oral and intravenous contrast medium is not essential for the diagnosis, it may be helpful in excluding the presence of frank perforation, obstruction, and toxic megacolon. On CT images, there is normal haustral marking, lack of gas in the distal colonic segments, and marked dilatation of the colon in the absence of any obstructive lesion [10]. Evidence of rapid cecal dilatation or a cecal diameter larger than 11 to 13 cm on abdominal x-ray radiographs has been associated with increased risk of cecal ischemia, necrosis, and perforation [5,7,11]. No consensus exists regarding the minimal cecal diameter required for the diagnosis; the most commonly agreed value is 9 cm, in our case this diameter is 13 cm. The main focus of management of Ogilvie’s syndrome relates to treating the underlying disorder and correcting any biochemical abnormalities. Initial management in acute colonic pseudo- obstruction usually involves confirmation of the syndrome. Subsequently, care can be divided into several phases. These phases include conservative, pharmaceutical, endoscopic and surgical management, all of which involve nursing input and specific nursing interventions most cases of acute colonic pseudo-obstruction respond to conservative management Studies have suggested that intravenous administration of neostigmine, an acetylcholinesterase inhibitor, causes rapid colonic decompression in people with Ogilvie’s syndrome [12]. It is speculated that the rationale of the pharmacological approach is based on the theory that acute colonic pseudo-obstruction results from parasympathetic dysfunction or excessive sympathetic stimulation. Neostigmine 2mg given intravenously over three to five minutes rapidly decompresses the colon in people with acute colonic pseudoobstruction who have failed to respond to conservative treatment [13]. In our case, after intramuscular injection of neostigmine colonoscopic decompression, defecation occurred approximately 2 h later. Recurrence after medical treatment is 20–50% [13] for recurrences; neostigmine may be a useful therapeutic agent, especially for uncomplicated cases.
Conclusion
Ogilvie’s syndrome is still a problem after hemorrhagic stroke of brain stem, this syndrome should be kept in mind, when the clinical picture of this syndrome occurs. Parenteral neostigmine injection might be a useful therapeutic tool, especially in the early phases of this syndrome.
Authors’ contributions
All the authors have contributed to this manuscript in ways that comply to the ICMJE authorship criteria. All the authors have read and approved the final version of the manuscript.
References
- Ogilvie H (1948) Large-intestine colic due to sympathetic deprivation; A new clinical syndrome. Br Med J 2(4579): 671-673.
- Laine L (1999) Management of acute colonic pseudo-obstruction. N Engl J Med 341(3): 192-193.
- Johanson JF, Sonnenberg A, Koch TR, McCarty DJ (1992) Association of constipation with neurologic diseases. Dig Dis Sci 37(2): 179-186.
- Veugelers R, Benninga MA, Calis EA, Willemsen SP, Evenhuis H, et al. (2010) Prevalence and clinical presentation of constipation in children with severe generalized cerebral palsy. Dev Med Child Neurol 52(9): e216-221.
- Rolandelli RH,Zinner MJ, Schwartz SI, Ellis H, et al. (1997) Maingot’s Abdominal Operations. (10th edn.), Stamford: Appleton and Lange pp. 347.
- Delgado-Aros C, Camilleri M (2003) Pseudo-obstruction in the critically ill. Best Prac Res Clin Gastroenterol 17(3): 427-444.
- Rondeau M, Weber JC, Nodot I, Storck D (2001) Acute colonic pseudoobstruction in internal medicine: etiology and prognosis, report of a retrospective study. Rev Med Interne 22(6): 536-541.
- Ponzano C, Nardi S, CARGHieri P (1997) Diagnostic problems, pathogenetic hypothesis and therapeutic proposals in Ogilvie’s syndrome. Review of 470 observations from the literature an presentation of 5 new cases. Minerva Chir 52(11): 1311-1320.
- Rex DK (1997) Colonoscopy and acute colonic pseudo-obstruction. Gastrointest Endosc Clin North Am 7(3): 499-508.
- Sheik RA, Yasmeen S, Pauly MP, Trudeau WL (2001) Pseudomembranous colitis without diARGHhea presenting clinically as acute intestinal pseudo-obstruction. J Gastroenterol 36(9): 629-632.
- Grassi R, Cappabianca S, Porto A, Sacco M, Montemarano E, et al. (2005) Ogilvie’s syndrome (acute colonic pseudo-obstruction): review of the literature and report of 6 additional cases. Radiol Med 109(4): 370-375.
- Turegano-Fuentes, Munoz-Jimenez, Del Valle-Hernandez, Pérez-Díaz D, Calvo-Serrano M, et al. (1997) Early resolution of Ogilvie’s syndrome with intravenous neostigmine: a simple, effective treatment. Diseases of the Colon and Rectum 40(11): 1353-1357.
- Ponec RJ, Saunders MD, Kimmey MB (1999) Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med 341(3): 137-141.






























