Randomized Controlled Trial on the ASSYST Treatment Intervention with Female Children Polytraumatized by Adverse Childhood Experiences, Neglect, and Maltreatment
Carretero KP1*, Delgadillo A1, Villarreal AM1, Roque JP1, Poiré A1, Mainthow N2, Givaudan M2 and Jarero I2
1Conexiones para aprender A.C, Mérida, Yucatán, México
2Department of Research, EMDR Mexico, Mexico City, Mexico
Submission: June 15, 2023; Published: July 31, 2023
*Corresponding author: Carretero; Kirsha Patricia; Conexiones para aprender A.C. Mérida; Yucatán and México, Email: byda.carretero@gmail.com
How to cite this article:Carretero KP, Delgadillo A, Villarreal AM, Roque JP, Poiré A. Randomized Controlled Trial on the ASSYST Treatment Intervention with Female Children Polytraumatized by Adverse Childhood Experiences, Neglect, and Maltreatment. Acad Acad J Ped Neonatol 2023; 12(5): 555901. 10.19080/AJPN.2023.12.555901
Abstract
The aim of this randomized controlled trial with an intention-to-treat analysis was to evaluate the effectiveness, efficacy, and safety of the Acute Stress Syndrome Stabilization Individual (ASSYST-I) treatment intervention in reducing posttraumatic stress disorder (PTSD) symptoms in female children polytraumatized by adverse childhood experiences, neglect, and maltreatment. A total of 40 female children met the inclusion criteria and participated in the study. Participants’ ages ranged from 8 to 17 years old (M =14.67 years). A two-arm randomized controlled trial (RCT) design was applied. PTSD symptoms were measured in three-time points for all participants in the study. Results showed that the intervention had a significant effect for time on PTSD symptoms (F (2,76) = 36.92 p <.000, η² = .493). A significant effect for group was also found (F (1, 38 = 32.7, p<.005, η² = .896) with a large effect, and a significant interaction between time and group, (F (2, 76) = 56.00, p <.000, η² = .600). Means comparison using t test between groups showed significant differences between the Treatment Group (TG) and the Control Group (CG) in the three-time points comparisons showing a large effect on Time 2 (Post-treatment assessment) which was maintained on Time 3 (Follow-up assessment). Results on the Reliable Change Index (RCI) and the Clinically Significant Change (CSC) Margin showed that the ASSYST-I treatment intervention exhibited reliable change on PTSD symptom reduction and clinically significant change, indicating that the treatment group participants are more likely to belong to the non-PTSD population after the intervention. Conversely, the control group participants are more likely to belong to the PTSD population. No adverse effects or events were reported by the participants during the treatment procedure administration or at follow-up. None of the participants showed clinically significant worsening/exacerbation of symptoms after treatment. Participants in the control group received the intervention treatment after the follow-up assessment, fulfilling our ethical criteria.
Keywords: Acute Stress Syndrome Stabilization; ASSYST; Posttraumatic stress disorder (PTSD), Female Children; Adverse Childhood Experiences; Neglect and Maltreatment
Introduction
Childhood abuse, neglect, and maltreatment, and especially polytraumatization, are known contributing factors to long-term insidious detrimental health defects. While definitions of abuse, neglect, and maltreatment vary and have evolved, the consensus in the scientific literature is that child maltreatment refers to acts of both commission (abuse) and omission or deprivation (neglect) that result in harm, potential harm, or threat of harm to a child and encompasses a variety of lived experiences [1]. These health defects in adults, such as diabetes, heart attack, obesity, cardiovascular and respiratory diseases, cancer, higher mortality rate, drug abuse, depression, anxiety, have been correlated with those who have lived adverse childhood experiences or ACEs, which include child abuse, neglect, and maltreatment, and are partially due to homeostatic changes to physiology and epigenetic processes during critical developmental periods [2-9].
Specifically, ages 3–5 have been associated with hippocampus development and exposure to abuse, neglect, and maltreatment may result in heightened vulnerability to later dissociation and posttraumatic stress disorder (PTSD), with ages 11–13 a key period affecting hippocampal development if exposed to abuse and neglect, age 10-11 affecting amygdala development, and ages 14-16 affecting prefrontal cortex development [10]. The neural processes affected in those who have experienced child abuse, neglect, and maltreatment are mainly in fronto-limbic networks including the medial prefrontal cortex, orbitofrontal cortex, anterior cingulate cortex, hippocampus, and amygdala, with neglect related to developmental changes in insula activation during risk processing and abuse related to developmental changes in fronto-parietal activation during cognitive control [11]. Studies also show that a smaller volume and altered activity patterns in the ventromedial region of the prefrontal cortex (vmPFC) have been observed in children with PTSD, suggesting the implication of frontal lobe circuitry in altered fear extinction features, affecting fear conditioning and learning, having important treatment implications [12].
The prevalence of child abuse, neglect, and maltreatment is alarming. On April 6, 2022, the United States Center for Disease Control and Prevention (CDC) reported that 1,750 children died of abuse and neglect in the year 2020 and that of the 74.2 million children in the US 10.6 million, or 1 out of 7, has experienced maltreatment in the previous year, which is likely underestimated due to lack of reporting [13]. Therefore, the need for prevention of child abuse, neglect, and maltreatment is crucial. In instances where prevention is not occurring, effective, efficient, and safe evidence-based PTSD treatment interventions for polytraumatized children is essential for the health, growth, and functioning of individuals, families, and communities.
AIP Theoretical Model
According to the Adaptive Information Processing (AIP) theoretical model memory networks of stored experiences are the basis of both human mental health and human pathology across the clinical spectrum. AIP disruptions due to high arousal states from adverse life experiences result in pathogenic memories that are inadequately processed and dysfunctionally stored in the brain. The information stored in these neurophysiological memory networks generates the present suffering, difficulties, and symptoms across the clinical spectrum [14,15].
PTSD and Intrusion Symptoms
According to the Diagnostic and Statistical Manual of Mental Disorders (5th Edition; DSM-5) posttraumatic stress disorder (PTSD) is a trauma- and stressor-related disorder occurring after exposure to one or more traumatic events (Criterion A). These Criterion A events include, but are not limited to, threatened or actual physical assault (e.g., childhood physical abuse, physical attack), threatened or actual sexual violence (e.g., forced sexual penetration, alcohol/drug-facilitated sexual penetration, abusive sexual contact, noncontact sexual abuse, sexual trafficking) (p. 274) [16].
PTSD Intrusion Symptoms associated with the traumatic event(s), beginning after the traumatic event occurred, are 1. Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s). 2. Recurrent distressing dreams in which the content and/or affect of the dream are related to the traumatic event(s). 3. Dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event(s) were recurring. 4. Intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event(s). 5. Marked physiological reactions to internal or external clues that symbolize or resemble an aspect of the traumatic event(s). “These intrusive memories often include sensory (e.g., sensing the intense heat that was perceived in a house fire), emotional (e.g., experiencing the fear of believing that one was about to be stabbed), or physiological (e.g., experiencing the shortness of breath that one suffered during a near-drowning) components.Some individuals with the disorder do not have intrusive memories of the event itself, but instead experience intense psychological distress or physiological reactivity when they are exposed to triggering events that resemble or symbolize an aspect of the traumatic event” (p. 271, 282-283) [16].
Acute Stress Syndrome Stabilization Individual Treatment Intervention
The Acute Stress Syndrome Stabilization (ASSYST) Individual treatment intervention was born during humanitarian fieldwork and is an AIP-informed, evidence-based, carefully field-tested, and user-friendly psychophysiological algorithmic approach, whose reference is the EMDR Protocol for Recent Critical Incidents and Ongoing Traumatic Stress (EMDR-PRECI) [17-25]. This treatment intervention is specifically designed to provide in-person or online support to clients who present Acute Stress Disorder (ASD) or Posttraumatic Stress Disorder (PTSD) intense psychological distress and/or physiological reactivity caused by the disorders’ intrusion symptoms associated with the memories of the adverse experience(s).
The objective of this treatment intervention is focused on the patient’s Autonomic Nervous System sympathetic branch hyperactivation regulation through the reduction or removal of the activation produced by the sensory, emotional, or physiological components of the pathogenic memories of the adverse experience(s) to achieve optimal levels of Autonomic Nervous System activation, stop the three major stress hormones [adrenaline (epinephrine), noradrenaline (norepinephrine), and cortisol] secretion, and reestablish the Prefrontal Cortex functions (e.g., processing of information); thus, facilitating the AIP-system and the subsequent adaptive processing of information [26].
Previous ASSYST Treatment Intervention Studies:
Seven previous studies on the ASSYST treatment interventions have proven their efficacy and safety with different populations: (I) General population in lockdown and with ongoing traumatic stress during the COVID-19 Pandemic. (II) TeleMental Health counseling to the general population after adverse experiences. (III) Mental Health Professionals working during the COVID-19 Pandemic with patients suffering from trauma-related disorders and stressors. (IV) General population with non-recent pathogenic memories. (V) Adult Syrian refugees living in Lebanon. (VI) Adult Females with Adverse Childhood Experiences. (VII) Public sector workers during the COVID-19 pandemic [27-33].
Reliable Change Index and Clinically Significant Change Margin
To know whether PTSD symptoms change does indeed indicate reliable and clinical significant change in this study, we used the Reliable Change Index (RCI) and the Clinically Significant Change (CSC) Margin. The RCI is used to determine if the magnitude of observed change over time on a given measure is beyond what should be attributed to measurement error. The CSC is used to determine if an observed end score on a measure of symptomatology indicates that respondent is more likely to belong to the non-disordered population than the disordered population. For the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL- 5), the more conservative value of the RCI is 18-points and ≤ 28 end score for the CSC margin [34].
Objective
The objective of this randomized controlled trial with intention-to-treat analysis was to evaluate the effectiveness, efficacy, and safety of the Acute Stress Syndrome Stabilization Individual (ASSYST-I) treatment intervention in reducing posttraumatic stress disorder (PTSD) symptoms in female children polytraumatized by adverse childhood experiences, neglect, and maltreatment.
Method
Study design
To measure the effectiveness of the ASSYST-I on the dependent variable PTSD symptoms, this study with an intention-to-treat analysis used a two-arm randomized controlled trial (RCT) with a waitlist no-treatment control group design. PTSD symptoms were measured at three time points for all participants in the study: Time 1. Pre-treatment assessment; Time 2. Post-treatment assessment; and Time 3. Follow-up assessment. For ethical reasons, all participants in the control group received the intervention treatment after the follow-up assessment was competed.
Ethics and research quality
The research protocol was reviewed and approved by the EMDR Mexico International Research Ethics Review Board (also known in the United States of America as an Institutional Review Board) in compliance with the International Committee of Medical Journal Editors recommendations, the Guidelines for Good Clinical Practice of the European Medicines Agency (version 1 December 2016), and the Helsinki Declaration as revised in 2013. The research quality of this study was based on the Consolidated Standards of Reporting Trials (CONSORT) 2010 Statement and the Standard Protocol Items Recommendation for Interventional Trials (SPIRIT) 2013 checklist [35,36].
Participants
This study was conducted in Toluca City, Mexico, from May to July 2023, with the Mexican (Latina) female child population with pathogenic memories from adverse childhood experiences (ACEs), neglect, and maltreatment living in a center under the Mexican Government’s protection. Forty-seven potential participants were recruited. Inclusion criteria was: (a) being a female child, (b) having pathogenic memories from ACEs, neglect, and maltreatment causing current distress, (c) voluntarily participating in the study, (d) not receiving specialized trauma therapy, (e) not receiving drug therapy for PTSD symptoms, (f) having a PCL-5 total score of 33 points or more. Exclusion criteria was: (a) ongoing self-harm/suicidal or homicidal ideation, (b) diagnosis of schizophrenia, psychotic, or bipolar disorder, (c) diagnosis of a dissociative disorder, (d) organic mental disorder, (e) a current, active chemical dependency problem, (f) significant cognitive impairment (e.g., severe intellectual disability, dementia), (g) presence of uncontrolled symptoms due to a medical illness. Seven of the 47 potential participants were excluded due to having PCL-5 scores under 33 points (subclinical symptoms). These seven participants have been living in the center since they were very young and were not exposed to prolonged adverse experiences like the other participants. A total of 40 females children met the inclusion criteria and participated in the study. Participants’ ages ranged from 8 to 17 years old (M =14.67 years). Participation was voluntary with the participants’ and their legal guardians signed informed consent in accordance with the Mental Capacity Act 2005.
Instruments for Psychometric Evaluation
a) We used the Trauma Screen Checklist from the Child PTSD Symptom Scale for DSM-5 for trauma-exposed children and adolescents for the study participants to choose the traumatic events they have lived prior to being rescued by the Mexican Government. This list contains 15 frightening or stressful events that can happen to children and all of them fulfill DSM-5 PTSD Criterion A. Participants chose the event that bothered them the most to answer the PCL-5 during the three assessment times [37,38].
b) To measure PTSD symptom severity and treatment response, we used the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) provided by the National Center for PTSD (NCPTSD) with the time interval for symptoms to be the past week. The instrument was translated and back-translated to Spanish. It contains 20 items, including three new PTSD symptoms (compared with the PTSD Checklist for DSM-IV) [39,40]: blame, negative emotions, and reckless or self-destructive behavior. Respondents indicated how much they have been bothered by each PTSD symptom over the past week (rather than the past month), using a 5-point Likert scale ranging from 0=not at all, 1=a little bit, 2=moderately, 3=quite a bit, and 4=extremely. A total symptom score of zero to 80 can be obtained by summing the items. The sum of the scores yields a continuous measure of PTSD symptom severity for symptom clusters and the whole disorder. Psychometrics for the PCL-5, validated against the Clinician- Administered PTSD Scale-5 (CAPS-5) diagnosis, suggest that a score of 31-33 is optimal to determine probable PTSD diagnosis, and a score of 33 is recommended for use at present [38-40].
Procedure
Randomization, Allocation Concealment Mechanism, and Blinding Procedure
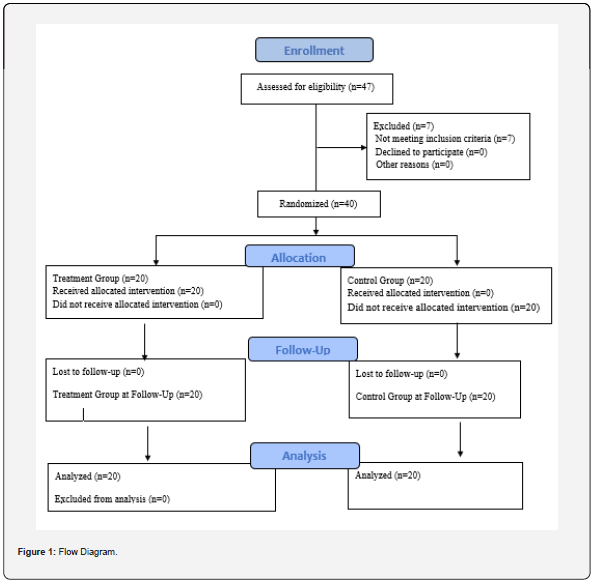
A computer-generated simple randomization with a 1:1 allocation ratio was used. Two independent assessors blind to treatment conditions conducted the randomization process to avoid allocation influence. The treatment random allocation sequence was concealed using sequentially numbered, opaque, sealed, and stapled envelopes who were open only after they were irreversibly assigned to the participants. The safekeeping of the envelopes and the assignment of participants to each arm of the trial (implementation of the random allocation sequence) was overseen by a person not involved in the research study and independent of the enrollment personnel. The treatment allocation of the participants was blinded for the research assistants who conducted the intake interview, initial assessment, and enrollment, and also for the independent assessors who conducted the followup assessments. Participants were instructed to not reveal their treatment allocation to the persons conducting the assessments. Twenty participants were allocated in the treatment group (TG) and twenty participants in the control group (CG). See Figure 1. Flow Diagram.
Enrollment, Assessments Times, Blind Data Collection, and Confidentiality of Data
Treatment group (TG) and control group (CG) participants completed the instruments in person and on an individual basis during distinct assessment moments. During Time 1, research assistants formally trained in all of the instruments’ administration, who were not blind to the study, but blind to the participant’s treatment allocation, conducted the intake interview, collected demographic data (e.g., name, age, gender, and contact information), assessed potential participants for eligibility based on the inclusion/exclusion criteria, obtained signed informed consent from the participants and their legal guardians, conducted the pre-treatment application of instruments, enrolled participants in the study, and randomly assigned each treatment group participant to one of the four clinicians formally trained in the ASSYST-I that participated in this study.
The research assistants also assisted the participants in identifying the pathogenic memory of their worst adverse experience from the Trauma Screen Checklist to be treated with the ASSYST-I. Each identified memory was written down by the research assistants on the Memory Record Sheets that were utilized by the clinicians during the ASSYST-I treatment intervention and utilized by participants during the three assessments times to ensure participants were focusing on the same memory when they received the treatment intervention, as well as the specific assessment time when they completed the assessment tools.
To obtain maximally interpretable PCL-5 scores, research assistants and independent assessors a) discussed with each participant the purpose of the instrument in detail, b) encouraged attentive and specific responding, c) invited participants to read each question carefully before responding and to select the correct answer, d) clarified their questions about some the symptoms, such as differentiating between intrusive memories and flashbacks, e) reworded conceptually complex symptoms (i.e., symptoms in the reexperiencing cluster) when necessary, f) reminded participants of the last-week symptom’s time frame, as well as, g) to only report symptoms related to the pathogenic memory of their worst adverse experience and not based on their everyday general distress.
During Time 2 (post-treatment assessment 7 days after treatment), and Time 3 (follow-up assessment 30 days after treatment), assessments were conducted for all participants by blind to treatment allocation independent assessors with formal training in administration of the instruments. The data safe keeper independent assessor received the participant’s assessment instruments that were answered during Times 1, 2, and 3. All data was collected, stored, and handled in full compliance with the EMDR Mexico International Research Ethics Review Board requirements to ensure confidentiality. Each study participant and their legal guardians gave their consent for access to their data, which was strictly required for study quality control. All procedures for handling, storing, destroying, and processing data were in compliance with the Data Protection Act 2018. All persons involved in this research project were subject to a signed professional confidentiality agreement.
Withdrawal from the Study and Missing Data
All research participants had the right to withdraw from the study without justification at any time and with assurances of no prejudicial result. If participants decided to withdraw from the study, they were no longer followed up in the research protocol. There were no withdrawals or missing data during this study.
Treatment
Clinicians and Treatment Fidelity
The ASSYST-I was provided in-person to individual participants by four licensed clinicians formally trained in this treatment intervention. Clinicians received on-going supervision and clinical feedback from the research project Clinical Director through daily group supervision and completing detailed session summary forms for each session with each participant that they were assigned that were designed specifically for the ASSYST-I treatment intervention to guide, elicit, monitor, and facilitate clinicians’ treatment adherence.
Treatment Description and Treatment Safety
An AIP & Symptom trajectory-based stepped care approach to adverse experiences was used during this study. This means a stepped progression of mental health care provided in an increasingly intensified manner based on the ongoing monitoring of the PTSD symptom trajectory during the study. The main objectives of this approach are a) to strategize treatment, b) to provide the treatment interventions according to the progression of the pathophysiology, and c) to improve symptom relief and clinical outcomes. After an adverse experience, the steps we follow are based on current evidence-based interventions. Step 1. Watchful waiting (monitoring of symptoms over time). Step 2. Psychoeducation, and support from families and close friends. Step 3. ASSYST for Individuals or Groups. Step 4. EMDR Integrative Group Treatment Protocol. Step 4. EMDR Protocol for Recent Critical Incidents and Ongoing Traumatic Stress. Step 5. Pharmacotherapy.
Participants’ treated memories were an average of 4.56 years old and received six in-person sessions, with an average length of 35-40 minutes per session. The ASSYST-I treatment intervention focused on the pathogenic memory produced by the worst adverse experience selected during T1. Pre-treatment assessment. To ensure the continuity and congruency of the intervention and measurement of its efficiency and efficacy, as mentioned above, during the intake interview after the memory was selected, the research assistants conducting the intake interview wrote down the specific memory on a Memory Record Sheet, which was used during each session of the ASSYST-I treatment procedure and was referenced to answer T1, T2, and T3 assessments.
At the beginning of the first treatment session, the participants were asked to run a mental movie of the specific previously selected memory, and then to choose the worst part. The treatment intervention was considered complete when the participant’s subjective levels of disturbance associated with the pathogenic memory decreased to zero or one (ecological/realistic). The ASSYST treatment intervention was provided to all the treatment group participants in an intensive treatment modality with two 60 minutes (max) sessions provided per day over three consecutive days.
Treatment safety was defined as the absence of adverse effects, events, or symptoms worsening. Therefore, participants were instructed by their clinicians to immediately report any adverse effects (e.g., dissociative symptoms [derealization/ depersonalization], fear, panic, freeze, shut down, collapse, fainting); events (e.g., suicidal ideation, suicide attempts, selfharm, homicidal ideation); or symptoms worsening during the entire study timeframe. A clinician working at the center on a regular basis was in charge of reporting to the research project Clinical Director any adverse effects, events, or worsening of symptoms during the study. No adverse effects or events were reported by the TG participants during the treatment procedure administration or at thirty-day follow-up. None of the participants in the TG showed clinically significant worsening/exacerbation of symptoms on the PCL-5 after treatment.
Examples of the Pathogenic Memories Treated with the ASSYST-I
Participants chose an average of five out of the fifteen traumatic events from the Trauma Screen Checklist. Examples of pathogenic memories treated during the ASSYST-I sessions were: a) Having been expelled from her house at age 8, being homeless, suffering continuous sexual rape including 10 men at the same time, and severe physical violence for years; b) having been burned on the genitals and legs with a lighter and on the back with a frying pan, and stabbed in the hand with a knife by the stepmother; c) attempted drowning in a water tank, hit with an electric cable, and burned by the stepmother; d) having been kidnapped, and for a whole year sexually abused, beaten, and her body used to test injected drugs; e) having been exploited by a sect; f) being tied to a chair and beaten by both parents.
Statistical Analysis
To analyze the effect of the ASSYST-I treatment on PTSD symptoms, analyses of variance (ANOVA) for three times repeated measurements (Time 1. Pre-treatment assessment; Time 2. Post-treatment assessment; and Time 3. Follow-up assessment), comparing Treatment group (TG) vs Control group (CG) was carried out. Eta squared (η²) is reported to show the effect sizes. Mean comparisons between and within groups using t test were conducted; Cohen´s d, is included to report the effect size.
Results
Effects on PTSD symptoms
Results showed that the intervention had a significant effect for time on PTSD symptoms (F (2,76) = 36.92 p <.000, η² = .493). A significant effect for group was also found (F (1, 38 = 32.7, p<.005, η² = .896) with a large effect, and a significant interaction between time and group, (F (2, 76) = 56.00, p <.000, η² = .600).
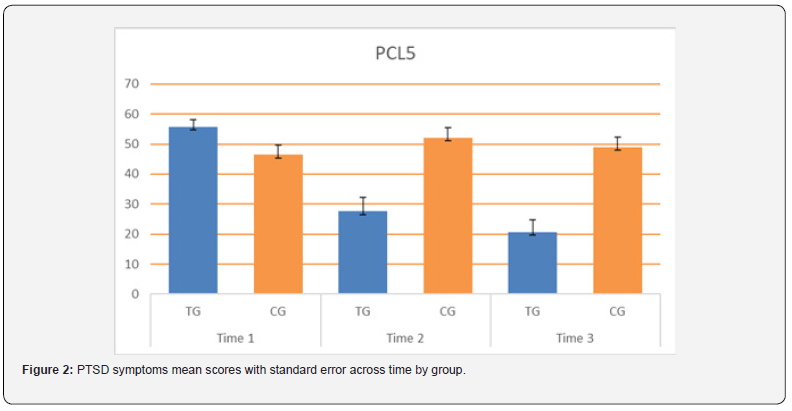
Mean comparisons between groups
Means comparison using t test between groups showed significant differences between the Treatment Group (TG) and the Control Group (CG) in the three time-point comparisons. For Time 1. Pre-treatment assessment (M = 55.70, SD = 10.50 vs M = 46.40, SD = 14.50), t (38) = 2.32, p<.05, d = .73, with a medium effect size. For Time 2. Post-treatment assessment. (M = 27.55, SD = 20.71 vs M = 52.00, SD = 15.74), t (38) = -4.20, p = .000, d = -1.72, with a large effect size and for Time 3. Follow-up assessment (M = 20.65, SD = 18.62 vs M = 48.95, SD = 15.46), t (38) = - 5. 22, p = .000, d = -1.65, also with a large effect size.
Mean comparisons within groups:
Intragroup means comparisons using t test for Treatment group (TG) showed significant differences between Time 1 Pretreatment assessment and Time 2. Post-treatment assessment, t (19) = 7.40, p=.000, d = .73, with a medium effect size. Comparisons between Time 2. Post-treatment assessment and Time 3 Follow-up assessment, t (19) = 2.17, p < .05, d =. 24 also showed significant differences, with a small effect size.
Intragroup means comparisons using t test for Control group (CG) showed significant differences both with a small effect size. between Time 1. Pre-treatment assessment and Time 2. Posttreatment assessment, t (19) = -2.56, p =.01, d = -.25 and between Time 2. Post-treatment assessment and Time 3. Follow-up assessment, t (19) = 3.70, p=.001, d = .13. See Table 1 and Figure 2.
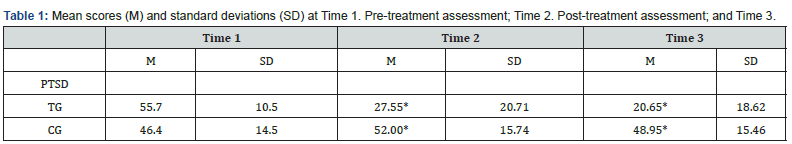
*Statistically significant differences between groups with a large effect size.
Discussion
The aim of this randomized controlled trial with an intentionto- treat was to evaluate the effectiveness, efficacy, and safety of the Acute Stress Syndrome Stabilization Individual (ASSYST-I) treatment intervention in reducing posttraumatic stress disorder (PTSD) symptoms in female children polytraumatized by adverse childhood experiences, neglect, and maltreatment. A total of 40 females children met the inclusion criteria and participated in the study. Participants’ ages ranged from 8 to 17 years old (M =14.67 years). A two-arm randomized controlled trial (RCT) design was applied.
Result showed statistically significant differences between groups from the pre-treatment assessment with a lower score for PTSD symptoms for the Control group, the effect size of these differences by Time 1 was considered small according to Cohen´s calculator. However, significant differences with a large effect size were found for the Post-treatment and Follow-up assessment comparing the two groups. For the Post-treatment assessment scores had increased for the Control Group in contrast with the Treatment group, this statistically significant difference was confirmed with the large effect size obtained. These differences between groups were maintained by the follow up assessment and can be attributed to the treatment.
Regarding the Reliable Change Index (RCI), 18 out of 20 TG participants (90%) exhibited reliable change on symptom reduction with an average of 37.61 points of PTSD symptom reduction, 18-points being the more conservative value. This is indicative that the ASSYST-I treatment intervention reduced PTSD symptom severity beyond what is attributable to measurement error.
In reference to the Clinically Significant Change (CSC) margin, 14 out of 20 TG participants (70%) exhibit clinically significant change, indicating that these participants are more likely to belong to the non-PTSD population. Following our AIP & Symptom trajectory-based stepped care approach to adverse experiences, EMDR therapy was provided to the six participants that did not reach a CSC margin after the Time 3 Follow-up assessment.
Conclusion
The evidence of the detrimental mental and physical effects of ACEs, particularly child abuse, neglect, and maltreatment, has been well documented and researched, and the individual and societal negative outcomes are widely known. Prevention is the most effective and ideal approach to combating PTSD and PTSD symptoms in children and adolescents. For those who have experienced ACEs or various types of child maltreatment, vital to the health of children, and long-term health outcomes of adults is an effective and efficient (time and cost) PTSD treatment intervention that can be used with children to prevent undesirable long-term health outcomes. With the abundance of studies demonstrating the negative effects of ACEs and childhood maltreatment, there is a lack of studies with evidence for effective PTSD treatment in polytraumatized children, which is a devastating problem that does not know regional confinement, causing mental and physical health problems, at a neural and structural level, that requires high quality, evidence-based PTSD treatment interventions. This paper is intended to fill some of the gap in the lack of research and evidence for PTSD treatment interventions for polytraumatized children.
Limitations, and Future Directions
The small sample size and the follow-up assessment at 30 days due to ethical reasons (providing treatment to the CG participants as soon as possible) are limitations of this study. We recommend future multicenter randomized controlled trials with an intentionto- treat analysis, a larger sample, follow-up assessment at six months, and following the Consolidated Standards of Reporting Trials (CONSORT) 2010 Statement and the Standard Protocol Items Recommendation for Interventional Trials (SPIRIT) 2013 checklist.
Conflict of Interest and Funding:
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We want to express our gratitude to all the clinicians and research assistants that participated in this study, and especially to Verónica Valverde Chávez, Tania Margarita Valdés Estrada, Fundación Gigante, Fundación Familia Bocar, Fundación Dibujando un Mañana and Fundación Compartamos: Conexiones para Aprender, and Save the Children Mexico.
References
- Taina Laajasalo, Laura Elizabeth Cowley, Gabriel Otterman, Diogo Lamela, Leonor Bettencourt Rodrigues, et al. (2023) Current issues and challenges in the definition and operationalization of child maltreatment: a scoping review. Child Abuse & Neglect 140: 106187.
- Monnat M, Chandler RF (2015) Long-Term Physical Health Consequences of Adverse Childhood Experiences. The Sociology Quarterly 56(4): 723-752.
- Ross N, Gilbert R, Torres S, Dugas K, Jefferies P, et al. (2020) Adverse childhood experiences: assessing the impact on physical and psychosocial health in adulthood and the mitigating role of resilience. Child Abuse Neglect 103: 104440.
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, et al. (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine 14(4): 245-258.
- Riedl D, Lampe A, Exenberger S, Nolte T, Trawöger I, et al. (2020) Prevalence of adverse childhood experiences (ACEs) and associated physical and mental health problems amongst hospital patients: results from a cross-sectional study. Gen Hosp Psychiatry 64: 80-86.
- Novais M, Henriques T, Vidal-Alves MJ, Magalhães T (2021) When problems only get bigger: the impact of adverse childhood experience on adult health. Front Psychol 12: 693420.
- Merrick M, Ports KA, Ford DC, Afifi TO, Gershoff E, et al. (2017) Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse Negl 69: 10-19.
- Fujiwara T (2022) Impact of adverse childhood experience on physical and mental health: a life-course epidemiology perspective. Psychiatry Clin Neurosci 76(11): 544-551.
- Layfield SD, Duffy LA, Phillips KA, Lardenoije R, Klengel T, et al. (2021) Multiomic biological approaches to the study of child abuse and neglect. Pharmacology Biochemistry and Behavior 210: 173271..
- Inga Schalinski, Martin H Teicher, Daniel Nischk, Eva Hinderer, Oliver Müller, et al. (2016) Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative, and depressive symptoms in adult patients. BMC Psychiatry 16: 295.
- Jungmeen Kim-Spoon, Toria Herd, Alexis Brieant, Kristin Peviani, Kirby Deater-Deckard, et al. (2021) Maltreatment and brain development: The effects of abuse and neglect on longitudinal trajectories of neural activation during risk processing and cognitive control. Developmental Cognitive Neuroscience 48: 100939.
- Kerbage H, Bazzi O, El Hage W, Corruble E, Purper-Ouakil D, et al. (2022) Early interventions to prevent post-traumatic stress disorder in youth after exposure to a potentially traumatic event: a scoping review. Healthcare 10(5): 818.
- Centers for Disease Control and Prevention (2022) Fast facts: Preventing child abuse & neglect violence prevention injury Center CDC. Centers for Disease Control and Prevention.
- Shapiro F (2018) Eye movements desensitization and reprocessing. Basic principles, protocols, and procedures (Third edition). Guilford Press
- Hase M, Balmaceda UM, Ostacoli L, Liebermann P, Hofmann A, et al. (2017) The AIP Model of EMDR Therapy and Pathogenic Memories. Front. Psychol 8: 1578.
- Vihang N Vahia (2013) American Psychiatric Association, Diagnostic and statistical manual of mental disorders (5th Edtn.) Arlington, VA, United States. Indian J Psychiatry 55(3): 220-223.
- Jarero I, Artigas L, Luber M (2011) The EMDR protocol for recent critical incidents: Application in a disaster mental health continuum of care context. Journal of EMDR Practice and Research, 5(3):82-94.
- Jarero I, Uribe S (2011) The EMDR protocol for recent critical incidents: Brief report of an application in a human massacre situation. Journal of EMDR Practice and Research 5(4): 156-165.
- Jarero I, Uribe S (2012) The EMDR protocol for recent critical incidents: Follow-up Report of an application in a human massacre situation. Journal of EMDR Practice and Research 6(2): 50-61.
- . Jarero I, Amaya C, Givaudan M, Miranda A (2013) EMDR Individual Protocol for Paraprofessionals Use: A Randomized Controlled Trial Whit First Responders. Journal of EMDR Practice and Research 7(2): 55-64.
- Jarero I, Uribe S, Artigas L, Givaudan M (2015) EMDR protocol for recent critical incidents: A randomized controlled trial in a technological disaster context. Journal of EMDR Practice and Research 9(4): 166-173.
- Jarero I, Schnaider S, Givaudan M (2019) EMDR Protocol for Recent Critical Incidents and Ongoing Traumatic Stress with First Responders: A Randomized Controlled Trial. Journal of EMDR Practice and Research 13(2): 100-110.
- Encinas M, Osorio A, Jarero I, Givaudan M (2019) Randomized Controlled Clinical Trial on the Provision of the EMDR-PRECI to Family Caregivers of Patients with Autism Spectrum Disorder. Psychology and Behavioral Science International Journal 11(1): 1-8.
- Estrada BD, Angulo BJ, Navarro ME, Jarero I, Sánchez-Armass O, et al. (2019) PTSD, Immunoglobulins, and Cortisol Changes after the Provision of the EMDR- PRECI to Females Patients with Cancer-Related PTSD Diagnosis. American Journal of Applied Psychology 8(3): 64-71.
- Jiménez G, Becker Y, Varela C, García P, Nuño MA, et al. (2020) Multicenter Randomized Controlled Trial on the Provision of the EMDR-PRECI to Female Minors Victims of Sexual and/or Physical Violence and Related PTSD Diagnosis. American Journal of Applied Psychology 9(2): 42-51.
- Jarero I (2021) ASSYT Treatment Procedures Explanation. Technical Report. Research Gate
- . Becker Y, Estévez ME, Pérez MC, Osorio A, Jarero I, et al. (2021) Longitudinal Multisite Randomized Controlled Trial on the Provision of the Acute Stress Syndrome Stabilization Remote for Groups to General Population in Lockdown During the COVID-19 Pandemic. Psychology and Behavioral Science International Journal 16(2): 1-11.
- Smyth-Dent K, Becker Y, Burns E, & Givaudan M (2021) The Acute Stress Syndrome Stabilization Remote Individual (ASSYST-RI) for TeleMental Health Counseling After Adverse Experiences. Psychology and Behavioral Science International Journal 16(2): 1-7.
- Magalhães SS, Silva CN, Cardoso MG, Jarero I, Pereira Toralles MB, et al. (2022) Acute Stress Syndrome Stabilization Remote for Groups Provided to Mental Health Professionals During the Covid-19 Pandemic. Journal of Medical and Biological Science 21(3): 637-643.
- Mainthow N, Pérez MC, Osorio A, Givaudan M, Jarero I, et al. (2022) Multisite Clinical Trial on the ASSYST Individual Treatment Intervention Provided to General Population with Non-Recent Pathogenic Memories. Psychology and Behavioral Science International Journal 19(5).
- Smith S, Todd M, Givaudan M (2023) Clinical Trial on the ASSYST for Groups Treatment Intervention Provided to Syrian Refugees living in Lebanon. Psychology and Behavioral Science International Journal 20(2): 1-8.
- Mainthow N, Zapien R, Givaudan M, Jarero I (2023) Longitudinal Multicenter Randomized Controlled Trial on the ASSYST Individual Treatment Intervention Provided to Adult Females with Adverse Childhood Experiences. Psychology and Behavioral Science International Journal 20(3): 556040.
- Magalhães SS, Guimarães ACF, Silva CN, Souza JSS, Carasek L, et al. (2023) Randomized Clinical Controlled Trial on the ASSYST Treatment Intervention Provided to Public Sector Workers During the COVID-19 Pandemic. Psychology and Behavioral Science International Journal 20(5): 1-11.
- Marx BP, Lee DJ, Norman SB, Bovin MJ, Sloan DM, (2021) Reliable and Clinically Significant Change in the Clinician-Administered PTSD Scale for DSM-5 and PTSD Checklist for DSM-5 Among Male Veterans. Psychological Assessment. Advance online publication.
- David Moher, Sally Hopewell, Kenneth F Schulz, Victor Montori, Peter C Gøtzsche, et al. (2010)Consolidated Standards of Reporting Trials. (CONSORT) 2010 Statement 340: 869
- An-Wen Chan, Jennifer M Tetzlaff, Douglas G Altman, Andreas Laupacis, Peter C Gøtzsche, et al. (2013) Standard Protocol Items Recommendation for Interventional Trials . (SPIRIT) 2013 Checklist. Retrieved at 158(3): 200-207.
- Edna B Foa, Anu Asnaani, Yinyin Zang, Sandra Capaldi, Rebecca Yeh, et al. (2018) Psychometrics of the Child PTSD Symptom Scale for DSM-5 for Trauma-Exposed Children and Adolescents. Journal of Clinical Child & Adolescent Psychology 47(1): 38-46.
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, et al. (2013) The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov.
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, et al. (2016) Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders- Firth edition (PCL-5) in veterans. Psychol Assess 28(11): 1379-1391.
- Franklin CL, Raines AM, Cucurullo L-A, Chambliss JL, Maieritsch KP, et al. (2018) 27 ways to meet PTSD: Using the PTSD-checklist for DSM-5 to examine PTSD core criteria. Psychiatry Research 261: 504-507.






























