Less Than Half of Pediatricians Educate Parents of Newborns on Risks and Benefits of Swaddling
Joshua Yang , Erica Ragen and Rachel Y Goldstein*
Children’s Hospital Los Angeles, USA
Submission: March 21, 2018; Published: June 21, 2018
*Corresponding author: Rachel Y Goldstein MD, MPH, Children’s Orthopaedic Center , Children’s Hospital Los Angeles, 4650 Sunset Blvd MS #69 Los Angeles CA 90027, USA.
How to cite this article:Joshua Y BA, Erica R P, Rachel Y G. Less Than Half of Pediatricians Educate Parents of Newborns on Risks and Benefits of Swaddling. Acad J Ped Neonatol. 2018; 6(5): 555756. DOI: 10.19080/AJPN.2018.06.555756
Abstract
Objectives: To determine what education parents and what training pediatricians are receiving on swaddling.
Study Design: Parents of newborns were surveyed about their experiences with swaddling. Pediatricians were also surveyed about their training and counseling they administered.
Results: 100 parents completed the survey. Mean age of patients was 5.1 months. 42% of parents currently swaddled their child at time of clinic visit, while 79% (46/58) swaddled their child at one point. 48% of parents received instructions on swaddling from non-medical resources. 66% reported that they had not been counseled about any risks to swaddling. 49 pediatricians were surveyed. 63%were not educated about safe swaddling practices during their training. 55% routinely educated parents about safe swaddling while 45% discussed the risks of swaddling.
Conclusion:With most parents not counseled on the risks to swaddling, there is a need for pediatricians to routinely counsel parents on the risks and benefits to swaddling.
Keywords: Counseling; Infants; Educational Tools; Swaddling Guidelines; Risks
Introduction
Swaddling is a common practice that has gained popularity and interest internationally with various studies examining its favorable outcomes [1]. Reports on the benefits of swaddling include quieter sleep patterns in infants which help reduce the risk of regulatory disorders in the child and stress for the parent [2-5].
However, various reports have cited swaddling as a controversial issue due to an array of risks associated with its practice [1,6-12]. In 2015, the Centers for Disease Control and Prevention (CDC) reported 1,600 deaths from Sudden Infant Death Syndrome (SIDS) which was the leading cause of infant death in the United States [13]. With swaddling a known link to SIDS, previous studies have presented safe swaddling practices to minimize the risk of SIDS or other complications such as overheating and hip dysplasia [14]. In 2016, the American Academy of Pediatrics (AAP) updated their guidelines and policy on swaddling and determined that with their recommendations, decisions should be made on an individual basis depending on the physiological need of the infant [15].
There is a variety of educational tools available through various online search engines and pediatric societies; however, it remains unclear what information parents are being educated on safe swaddling practices. In addition, there have been no studies surveying what types of education and counsel pediatricians are administering to parents of newborns. The purpose of this study was to explore the educational practices that pediatricians were offering and the knowledge of parents on safe swaddling practices.
Methods
After IRB exemption was granted at our institution, parents of patients aged 0-12 months who presented to clinic for any evaluation without a diagnosis of hip dysplasia were enrolled into this prospective study. Parents were administered an anonymous one-time survey in regards to their swaddling practices and knowledge.
Additionally, pediatricians and pediatric residents in a major metropolitan area were also administered an anonymous one-time survey to assess their training and counseling practices regarding safe swaddling techniques. All surveys were distributed through RedCap© and results were reported using mean values.
Results
100 parents of patients were enrolled at their child’s routine clinic visit, and patients had a mean age of 5.1 months (range: 0-12 months). 43% (43/100) of parents swaddled their child at time of the survey. Of the parents that did not swaddle their child at time of the survey, 81% (46/57) had swaddled their child prior to clinic visit and discontinued at a mean age of 2.8 months (range: 0-9 months). 11% (11/100) of parents have never swaddled their child.
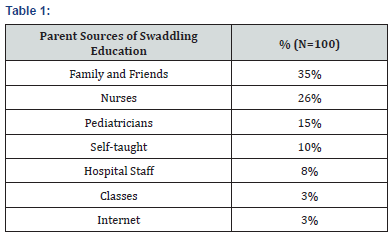
Parents discontinued swaddling for the following reasons: 59% (27/46) Child disliked swaddling, 35% (16/46) child outgrew swaddling, 4% (2/46) child started to roll over, 2% (1/46) pediatrician recommended stopping, 2% (1/46) child became too hot, 2% (1/46) discontinued on their own. Interestingly, 48% (48/100) of parents received instructions on swaddling from non-medical resources (Table 1). Only 34% (34/100) of parents were counseled on the risks to swaddling with only 24% (8/34) counseled about hip dysplasia (Table 2).

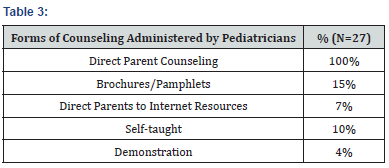
49 pediatricians/trainees were administered the survey with a mean practice of 12.1 years (range: 0-47 years). 55% (27/49) practiced in an outpatient primary care facility, 16% (8/49) were inpatient hospitalist, 14% (7/49) were pediatric residents, 10% (5/49) were outpatient subspecialist, and 4% practiced in multiple hospitals/practices. 20% (10/49) completed a fellowship prior to this survey. During their training, 37% (18/49) were educated about safe swaddling practices and 55% (27/49) of pediatricians counseled parents of newborns about safe swaddling (See Table 3 for types of counseling administered). There were no significant differences shown between pediatricians who were trained and not trained on swaddling and if they routinely counseled parents on safe swaddling (p=0.178). Of the 18 pediatricians/trainees who were educated on safe swaddling practices, 67% (12/18) routinely counseled on safe swaddling.
Of the 55% of physicians surveyed who counseled parents on safe swaddling practices, 81% (22/27) discussed the risks and benefits of safe swaddling practices to parents. Pediatricians/ trainees routinely discussed the following risks to parents: 63% (17/27) sudden infant death syndrome (SIDS), 44% (12/27) overheating, and 44% (12/27) hip dysplasia. In addition, they recommended discontinuing swaddling at a mean age of 3.9 months (range: 1-9 months). Of all the 49 surveyed, only 37% (18/49) were aware of the International Hip Dysplasia Institutes (IHDI) recommendations for healthy hip swaddling.
Discussion
Swaddling has shown to be a beneficial tool in promoting infant sleep [3]. Although the risks of swaddling have been well documented, there are no studies investigating what types of information parents are receiving and what types of counseling pediatricians are administering [1,3,6-11,14,16-18]. In our study, we found that more than half of parents utilize non-medical resources as the primary educational tool on swaddling while only a third of parents were counseled on the risks of swaddling. In addition, 37% of pediatricians were formally educated on swaddling, while 55% of pediatricians routinely counseled on the risks and benefits of swaddling.
Although there has been a movement toward safe swaddling from pediatric societies such as the AAP, there is a lack of educational presence from pediatricians and allied health professionals in their practice. Recent studies have provided the risks involved with improper swaddling techniques. Mcdonnell et. al reported similar conclusions from the 2011 AAP policy statement that swaddled infants should be placed supine to reduce the risk of infants rolling over to the prone position which significantly increases risks [9]. An integrative review of the risks and benefits of swaddling also promoted evidence based swaddling recommendations and informed decision-making among infant caregivers [11]. Although the importance of swaddling education and recommendations are present in the literature, parents of infants have been utilizing non-medical resources, notably family/ friends, as their primary source of education. Concurrently, pediatricians in this study have reported that not only 37% have been formally educated on safe swaddling practices, but also 55% only routinely counsel on the risks to swaddling. With the ample amount of resources and publications for pediatricians on the risks and recommendations on swaddling, these results raise concerns of the quality of education parents are receiving, and the rate at which pediatricians are formally educated and counsel parents about swaddling. By incorporating formal training that include risk and benefit counseling on swaddling, parents can be adequately educated on the importance of safe swaddling.
Hip dysplasia interestingly was the least counseled risk discussed with parents by pediatricians. Of the 100 parents in this study, 24% were counseled on hip dysplasia as a risk factor while 24% of the 49 pediatricians routinely counseled parents on hip dysplasia as a risk. With previous reports reporting that keeping hips extended and adducted promote dysplasia, swaddling has been recognized as a risk factor for developmental dysplasia of the hip (DDH) [12,16,19]. Recommended that monitoring is needed to lessen the risk of DDH to ensure that hips are allowed to flex and abduct in a safe position for hip development [19]. The IHDI’s stance on swaddling also calls for hips to be in slight flexion and abduction to allow free movement [20]. Because the incidence of instability of the hip in newborns can be upwards of 1 in 100, improper swaddling technique can increase the risk of hip dysplasia [21,22]. With only 37% of the 49 pediatricians aware of the IHDI’s recommendations on healthy hip swaddling, there is great concern for the education that parents and pediatricians are receiving on proper techniques in swaddling and the risk for hip dysplasia.
The usefulness of an educational intervention seems warranted to incorporate safe swaddling practices. However, reported a series of 40 mothers of infants who underwent a swaddling educational intervention which included supine positioning of the infant and discouragement of bed sharing [23]. This intervention increased the use of swaddling, but had a limited impact on the given safe sleeping practices [23]. Although the study properly taught how to swaddle infants in the intervention group, the intervention did not include counsel on the risks of improper swaddling techniques which could have encouraged the use of safe swaddling. Further study into swaddling counseling should be investigated to encourage the importance of safe swaddling practices and education.
This study proved to be limited by its sample size and anonymity. Previous health histories and biases on swaddling could have affected parent answers on the questionnaire. In addition, although this study was conducted in a major metropolitan area and diverse community, demographic information was not recorded which could have shown differences in parents with different levels of education or socioeconomic status. Relationships between counsel on swaddling and demographic information should be investigated to see if there are discrepancies in education between socioeconomic statuses of families.
Conclusion
Approximately half of the surveyed parents were taught how to swaddle by clinicians or hospital classes, and most had not been counseled about the risks to swaddling. Concurrently, over half of the surveyed pediatricians were not educated about swaddling practices during their training. With a significant amount of education on safe swaddling practices coming from non-medical resources, there is a need for pediatricians to routinely counsel parents on safe swaddling practices including the risks and benefits to swaddling.
References
- van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TW, et al. (2007) Swaddling: a systematic review. Pediatrics 120(4): e1097-e1106.
- Oden RP, Powell C, Sims A, Weisman J, Joyner BL, et al. (2012) Swaddling: will it get babies onto their backs for sleep? Clin Pediatr (Phila) 51(3): 254-259.
- Gerard CM, Harris KA, Thach BT (2002) Physiologic studies on swaddling: an ancient child care practice, which may promote the supine position for infant sleep. J Pediatr 141(3): 398-403.
- Franco P, Seret N, Van Hees JN, Scaillet S, Groswasser J, et al. (2005) Influence of swaddling on sleep and arousal characteristics of healthy infants. Pediatrics 115(5): 1307-1311.
- Brackbill Y (1971) Cumulative effects of continuous stimulation on arousal level in infants. Child development 42(1): 17-26.
- Thach BT (2009) Does swaddling decrease or increase the risk for sudden infant death syndrome? J Pediatr 155(4): 461-462.
- Ponsonby AL, Dwyer T, Gibbons LE, Cochrane JA, Wang YG (1993) Factors potentiating the risk of sudden infant death syndrome associated with the prone position. N Engl J Med 329(6): 377-382.
- Pease AS, Fleming PJ, Hauck FR, Moon RY, Horne RS et al. (2016) Swaddling and the Risk of Sudden Infant Death Syndrome: A Metaanalysis. Pediatrics 137(6): e20153275.
- McDonnell E, Moon RY (2014) Infant deaths and injuries associated with wearable blankets, swaddle wraps, and swaddling. J Pediatr 164(5): 1152-1156.
- Richardson HL, Walker AM, Horne RS (2009) Minimizing the risks of sudden infant death syndrome: to swaddle or not to swaddle? J Pediatr 155(4): 475-481.
- Nelson AM (2017) Risks and Benefits of Swaddling Healthy Infants: An Integrative Review. MCN Am J Matern Child Nurs 42(4): 216-225.
- Clarke NM (2014) Swaddling and hip dysplasia: an orthopaedic perspective. Archives of disease in childhood 99(1): 5-6.
- https://www.cdc.gov/sids/data.html
- Task Force On Sudden Infant Deaths (2016) SIDS and Other Sleep- Related Infant Deaths: Updated 2016 Recommendations for a Safe Infant Sleeping Environment. Pediatrics 2138(5).
- Moon RY, Task Force On Sudden Infant Death S (2016) SIDS and Other Sleep-Related Infant Deaths: Evidence Base for 2016 Updated Recommendations for a Safe Infant Sleeping Environment. Pediatrics 138(5): e20162940.
- Harcke HT, Karatas AF, Cummings S, Bowen JR (2016) Sonographic Assessment of Hip Swaddling Techniques in Infants With and Without DDH. J Pediatr Orthop 36(3): 232-238
- Tsogt B, Manaseki-Holland S, Pollock J, Blair PS, Fleming P (2016) Thermoregulatory effects of swaddling in Mongolia: a randomised controlled study. Arch Dis Child 101(2): 152-160.
- Wang E, Liu T, Li J, Edmonds EW, Zhao Q et al. (2012) Does swaddling influence developmental dysplasia of the hip?: An experimental study of the traditional straight-leg swaddling model in neonatal rats. J Bone Joint Surg Am 94(12): 1071-1077
- Mahan ST, Kasser JR (2008) Does swaddling influence developmental dysplasia of the hip? Pediatrics 121(1): 177-178.
- Hip-Healthy Swaddling: Are you swaddling your baby properly? International Hip Dysplasia Institute 2018.
- Clinical practice guideline: early detection of developmental dysplasia of the hip. Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip. American Academy of Pediatrics (2000). Pediatrics 105(4 Pt 1): 896-905.
- Kotlarsky P, Haber R, Bialik V, Eidelman M (2015) Developmental dysplasia of the hip: What has changed in the last 20 years? World J Orthop 6(11): 886-901.
- Kelly BA, Irigoyen MM, Pomerantz SC, Mondesir M, Isaza-Brando N (2017) Swaddling and Infant Sleeping Practices. J Community Health 42(1): 10-14.






























