Vitamin K Deficiency Bleeding: A Case Revealed by Intracranial Haemorrhage
D D Ndour1* and M Mbaye2
1 Service de Pédiatrie- Néonatologie Centre Hospitalier National Dalal Jamm, Senegal
2 Service de Neurochirurgie, Chnu Fann, Senegal
Submission: November 30, 2017; Published: December 21, 2017
*Corresponding author: D D Ndour, Service de Pédiatrie- Néonatologie Centre Hospitalier National Dalal Jamm, Dakar, Senegal.
How to cite this article:D D Ndour, M Mbaye . Vitamin K Deficiency Bleeding: A Case Revealed by Intracranial Haemorrhage. Acad J Ped Neonatol. 2017; 6(2): 555737. DOI: 10.19080/AJPN.2017.06.555737
Abstract
We report a case of late haemorrhagic disease due to vitamin K deficiency, revealed by intracranial haemorrhage. Thelate form of haemorrhagic disease due to vitamin K deficiency is rare but potentially serious because it is life-threatening.From this case we propose a literature review to take stock of the haemorrhagic disease due to vitamin K deficiency, its diagnosis, its aetiologies and the various prophylaxis proposed.
Keywords: Haemorrhagic disease; Vitamin K; Subdural haematoma
Introduction
Intracranial haemorrhage in early childhood is associated with a wide variety of causes such as trauma, vascular malformations (aneurysm and arteriovenous malformation), haemorrhagic infarction, brain tumours or blood coagulation disorders (congenital or acquired from coagulation factors). Vitamin K deficiency causes blood coagulation disturbances that can lead to intracranial haemorrhage [1]. The classic role of vitamin K is its anti-haemorrhagic function which is necessary for the synthesis in the liver of the functional forms of prothrombin (factor II) and factors VII, IX and X. After secretion in the blood, these four Vitamin K – dependent factors participate in coagulation. A series of complex events leads to the conversion of fibrinogen to fibrin and the formation of a haemo static plug. Biochemically, the roles of vitamin K are multiple. It allows the carboxylation of glutamate residues into gamma-carboxyglutamate necessary for hepatic synthesis of vitamin K-dependent coagulation factors, and also for the synthesis of osteocalcin and other proteins involved in the vascular structure. The consequences of vitamin K deficiency for haemostasis are an inability to synthesize functional molecules of factors II, VII, IX and X resulting in a hypocoagulable state [2]. In the event of vitamin K deficiency, the liver synthesizes non-functional coagulation factors called PIVKA (Protein Induced by Vitamin K Absence or Antagonists). These proteins cannot fix calcium and act by inhibiting coagulation, which leads to a haemorrhagic syndrome. Haemorrhagic disease of the newborns was first described by Townsend in 1894. This terminology, however, is not concise because infants can also be affected and moreover it is not informative on the cause of the haemorrhagic disease. This is why the term haemorrhagic disease due to vitamin K deficiency seems more appropriate. It is a disease that has become rare in the industrialized countries thanks to the prophylaxis systematically proposed at birth and continued if necessary during the whole period of exclusive breastfeeding. The placental passage of vitamin K is weak and newborns have little hepatic reserve. All newborns are therefore deficient at birth. In addition,vitamin Kis low in breast milk. Breastfed newborns are therefore at risk of vitamin K deficiency and haemorrhagic disease. We report the case of an infant with late haemorrhagic disease due to vitamin K deficiency revealed by intracranial haemorrhage.
Case
This is a new-born male aged 1 month 1 day, hospitalized for generalized convulsions without fever.
Pregnancy and delivery occurred under normal conditions (no maternal medication taken during pregnancy apart from iron and vitamin supplementation, no risk of infection, delivery without obstetrical trauma and with a birth weight of 3010 g and a good adaptation to extra uterine life). The child was under exclusive breastfeeding. He had received 2 doses of oral vitamin K (1mg) at birth and on day 1 (first day of life). The mother reported diarrhoea a week earlier leading to a prescription for antibiotics. There was no history of convulsions in the family, nor a history of bleeding. On admission, a sleepy infant was noted at the clinical examination; slightly hypotonic. The rest of the neurological examination was normal. He had neither hepatomegaly nor splenomegaly. The growth in height and weight was considered satisfactory: the weight was 4020 g (+1 SD), the height of 55 cm (+2 SD) and the head circumference of 37.5 cm (+ 2 SD). The infectious balance (C-Reactive Protein, Procalcitonin, and Haemoculture) returned normal. The biological test showed a normal blood count and picture, a prothrombin time (PT) of 42% and an activated partial thromboplastin time (APTT) of 85 seconds for a control at 33 seconds with lowered vitamin K-dependent factors (factor II=0.04 IU / ml, factor VII=0.06 IU / ml, factor IX=0.04 IU / ml, factor X=0.05 IU / ml). The level of fibrinogen was normal as well as the liver function test (ASAT, ALAT, PAL and CGT) and the blood ionogram. The cerebral CT showed temporal and occipital sub dural haematoma and intraventricular haemorrhage (HIV) grade II of the Papile classification, which was seen already on cranial ultra sonography. Intravenous vitamin K treatment normalized the coagulation profile. There was no surgical indication for subdural haematoma and monitoring was recommended.
Discussion
Haemorrhagic disease due to vitamin K deficiency exists in 3 forms (Table I): early, classic and late forms.
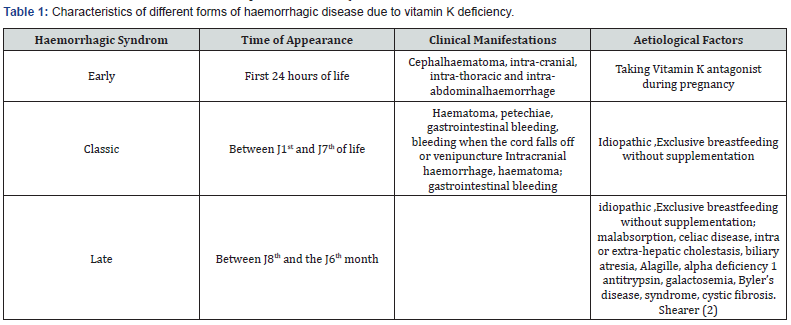
Early form
The early form is defined as bleeding attributable to a vitamin K deficiency in the first 24 hours of life. It is rare and is usually seen in infants whose mothers have received drugs that interfere with the Vitamin K metabolism, through known mechanisms (oral anticoagulants) or uncertain (anticonvulsants, such as phenytoin), anti tuberculous drugs (rifampicin, isoniazid) [2].
Classic form
It occurs typically between the 2nd and 7th day of life. Falsely thought to be idiopathic, it is most often secondary to inadequate nutrition. Taking medication during pregnancy is also incriminated. Several authors find a significant decrease in the activity of prothrombin between the 2nd and 3rd day of life.
Late form
It occurs between the 8th day of life and the 6th month with maximum incidence between the 3rd and 8th week of life. The late form is characterized by a high prevalence of intracranial haemorrhages, which are most often the circumstance of discovery [2]. It is almost always seen in infants exclusively breastfed. Hepatobiliary insufficiency is a contributing factor as well as malabsorption.
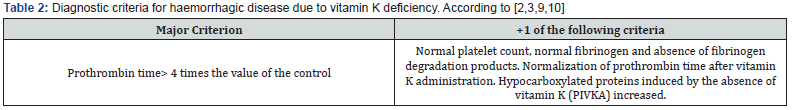
Our observation illustrates a late form which was revealed by the most serious and frequent clinical presentation, i. e. Intra cranial haemorrhage. Indeed the late form is considered to be serious with a risk of 50 to 70% of intracranial haemorrhage, 20% of mortality and 40% of severe neurological sequelae[3]. It can also be revealed by haematomas, gastrointestinal bleeding and mucosal bleeding. In one Ethiopian study, among 127 cases of haemorrhagic disease due to vitamin K deficiency, the most common bleeds were gastrointestinal (53%) and umbilical (23%) [4]. Only one child had intracranial bleeding. In this series, the mortality rate was 26% related to delayed diagnosis and management. Mortality is probably under estimated because in low-income countries many children die before arriving at the hospital [2,4] In Thailand, out of 691 cases of late form, the prevalence of intracranial haemorrhage was 82%, the mortality rate was 24% and about 50% of the survivors had permanent neurological deficits [5]. Chaou et al. [6] described the occurrence of cerebral haemorrhages with predominance in boys. They were revealed by a pallor, jaundice, fever, cyanosis and anisocoria between 10 and 40 days of life. The brain lesions found were subarachnoid haemorrhages in 91% of cases, alone or associated with subdural haematomas in 38% of cases, intra-parenchymal haemorrhage in 31% of cases, intra-ventricular haemorrhage in 13% of cases and haemorrhage from the posterior fossa in 9% of cases. In our observation, the infant had received incomplete prophylaxis. Prevention therefore has limits, particularly related to the observance of treatment. An intramuscular injection (IM) of 1 mg vitamin K at birth provides complete protection against both early and classic forms (with comparable efficacy of the IM and oral route) but also against the late form (with a higher efficiency of the IM route compared to the oral route) [2]. The French Society of Neonatology recommends for all full-term infants the systematic oral administration of three doses of vitamin K1 at 2 mg per dose: one at birth (or shortly thereafter), one between 72 and 96 hours of life and one at 1 month of life [7]. Biologically, a low prothrombin time (PT) with fibrinogen and a normal number of platelets is very supportive of diagnosis; a normal PT excludes the diagnosis; a rapid correction or a decrease in bleeding after vitamin K administration confirms the diagnosis [8]. For our child, paraclinical data favoured vitamin K deficiency, and intravenous vitamin K treatment normalized coagulation status rather quickly. The diagnosis of haemorrhagic disease due to vitamin K deficiency is biological and quite easy (Table 2). The hypocarboxylated proteins induced by the absence of vitamin K (PIVKA) remain detectable even after the administration of vitamin K, which makes it an excellent blood marker of the vitamin K deficit [2], apart from the situation of intoxication in vitamin K deficiency. In the face of haemorrhagic disease due to vitamin K deficit,it is important to look for a secondary cause. The causes of late form of haemorrhagic disease are numerous (Table I) [3]. Regarding the subdural haematoma, the treatment consists of an evacuation by transfontanellar puncture or a bit hole as soon as it causes complications, in particular compression of the brain structures. For our patient there was no surgical indication and clinical and CT surveillance was instituted.
Conclusion
Haemorrhagic disease due to vitamin K deficiency has become rare because of the systematic prevention but its incidence is difficult to determine. The late-onset of haemorrhagic disease due to vitamin K deficiency is a reality; it is severe and has a variable incidence depending on the type of prophylaxis. At the international level, it is recommended to give 1 single dose of 1 mg intra muscularly in all neonates at birth. However, many countries prefer the oral route. Our clinical case illustrates the importance of adequate prophylaxis in neonates under exclusive breastfeeding. It seems important, especially in low-income countries, that studies be conducted to evaluate the conditions of vitamin K use in hospitals and the incidence of haemorrhagic disease due to vitamin K deficiency.
Authors’ Statement
The authors declare that they have no conflicts of interest in relation to this article.
References
- Joseph JV (2014) Intracranial Hemorrhage in Early Infancy-Renewed Importance of Vitamin K Deficiency. Pediatr Neurol 50(6): 545-546.
- Shearer M (2009) Vitamin K deficiency bleeding in early infancy Blood Rev 23(2): 49-59.
- AB de C, Oudyia V, Bressona, Bosdurea E, B. Roquelaurec et al (2013) Maladie hémorragique par déficit en vitamine K : a` propos d’un cas secondaire à une cholestase néonatale transitoire. Archives de pédiatrie 503-506
- Lulseged S (1993) Haemorrhagic disease of the newborn: a review of 127 cases. Ann Trop Paediatr 13(4):331-6.
- Chuansumrit A, Isarangkura P, Hathirat P, Vitamin K Study Group(1998) Vitamin K deficiency bleeding in Thailand: a 32-year history. Southeast Asian J Trop Med Public Health 29(3):649-54.
- Chaou WT, Chou ML (1984) Eitzman DV: Intracranial hemorrhage and vitamin K deficiency in early infancy. J Pediatr 105(6): 880-884.
- Hascoet JM, Picaud JC,Lapillonne A, Boithias C, Bolot P (2015) VITAMINE K - Mise à jour des recommandations.SFN . Bulletin n° 06.
- Sutor AH, Kries VR, Cornelissen EA, McNinch AW, AndrewM (1999) Vitamin K deficiency bleeding (VKDB) in infancy. Thromb Haemost 81(3):456-61.
- Van WM, De BR, Van DVS, Van BS, et al (2009) Vitamin K, an update for the paediatrician. Eur J Pediatr 168(2):127-34.
- Cornelissen M, Von KR, Loughnan P, et al (1997) Prevention of vitamin K deficiency bleeding: efficacy of different multiple oral dose schedules of vitamin K. Eur J Pediatr 156(2):126-31.






























