Elective Gastrostomy Feeding in Children Using a Button
M Fall*, S Camara, IB Welle and G Ngom
Department of Pediatric Surgery of Albert Royer Children’s Hospital in Dakar, University Cheikh Anta Diop Senegal
Submission: February 19, 2017; Published: June 08, 2017
*Corresponding author: M Fall, Department of Pediatric Surgery of Albert Royer Children’s Hospital in Dakar, University Cheikh Anta Diop, BP 5005, Dakar Fann, Senegal.
How to cite this article: M Fall, S Camara, I Welle, G Ngom. Elective Gastrostomy Feeding in Children Using a Button. Acad J Ped Neonatol. 2017; 5(1): 555709. DOI: 10.19080/AJPN.2017.05.555709
Abstract
Aim: The goal of our study is to evaluate a new method of gastrostomy practiced for a few months in our service using a button installed by elective track under the left costal.
Patients and methods: This is a retrospective study of 02 years (January 2013- December 2014) collecting all records of patients who underwent a first gastrostomy feeding using a button that is posed on the left costal. The records of patients with gastrostomy tube or placed using a laparotomy and patients with a gesture associated with gastrostomy or laparotomy history were excluded.
Results: The series included 12 patients including 7 boys with an age averaged of 4.5 years (3 months and 8 years). The indication for surgery was dominated by caustic stenosis of the esophagus (91%). We noted two early leaks, one late leak (35 days postoperatively), one button drop and one erosion of the balloon. The average hospital stay was 05 days (04 and 08 days). The 02 deaths reported in the series are independent of the gastrostomy. Parents were satisfied due to the discretion of the device that offers the child a freedom of activity and a greater level of comfort.
Conclusion: The first elective gastrostomy feeding with the laparoscopy are the two less invasive techniques most relevant to our context since our main indication was a caustic stenosis of the esophagus.
Keywords: Gastrostomy; Children; Button; Dakar
Introduction
Gastrostomy is an alternative method of oral feeding that provides the body with the necessary nutrients through a tube inserted into the stomach through the intermediary of a stoma. Its realization is different depending on the team. Some choose the installation of a gastrostomy tubing (Foley, Malecot, and Pezzer) through an umbilical median first others choose the minimally invasive endoscopic or laparoscopic methods using a less bulky device (button) [1]. The gastrostomy feeding is a common indication in our practice conditions because of the high number of esophagus caustic burns sequelae. Previous work shows that a gastrostomy is performed in 18.3% (20/109) after caustic burns of the esophagus which represent 72% (56/77) indications [2,3]. The goal of our study is to evaluate a new method of gastrostomy practiced for a few months in our service using a button installed by elective track under the left costal.
Materials and Methods
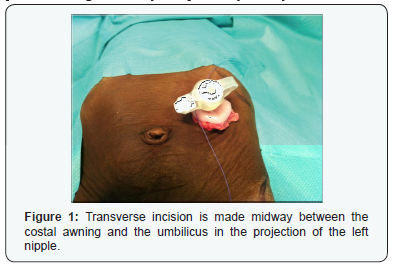
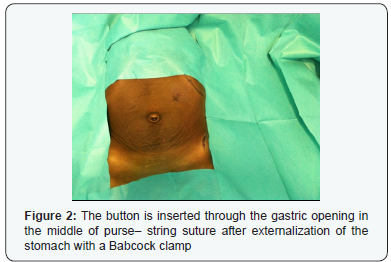
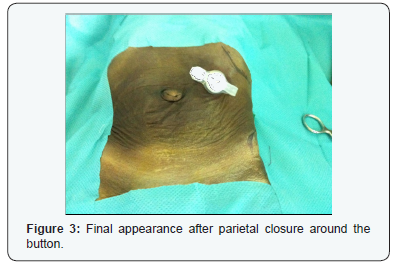
This is a retrospective study of 02 years (January 2013- December 2014) collecting all records of patients who underwent a first gastrostomy feeding using a button that is posed on the left costal at the Children Hospital Albert Royer of Dakar. The surgery is performed under general anesthesia in a patient in decubitus with a block under left costal. A transverse incision of 1.5 cm is made midway between the costal awning and the umbilicus in the projection of the left nipple (Figure 1). The opening of the fascial muscular planes and peritoneum is made gradually. The stomach can be exposed using 2 Farabeuf retractors, then seized by a Babcock clamp and exteriorized through the parietal opening. Sometimes we can use a malleable valve to rule out the left lobe of the liver. The stomach thus well spread with the anterior face exposed, we realized two concentrated purse – string sutures of absorbable threads 3/O. The heads of two purse – string sutures must be opposed. The opening of the stomach in the middle of purse – string suture is started with an electrical bistoury then completed and extended by the tip of a Kelly clip. The button is inserted through the gastric opening and the first purse – string sutures clamped above the balloon marker (Figure 2). The stomach is reinstated in the abdomen and then the balloon is inflated with 5 cc of sterile water and 2nd knot is tight at the top of the balloon. The two opposing heads knots are attached to the deep fascia which straightens the stomach and the abdominal wall. The parietal opening is closed around the button (Figure 3). We analyzed the age, the gender, the surgery indication, the postoperative complications and parental satisfaction. The records of patients with gastrostomy tubing placed using a laparotomy and patients with gastrostomy or laparotomy history were excluded.
Results
The series includes 12 patients with 7 boys with an average age of 4.5 years (3 months to 8 years). The surgical indication is dominated by caustic stenosis of the esophagus (1 case of bilateral lip and palate cleft problem). These patients were tardily admitted with an aspect aphasia and severe malnutrition after ingestion of caustic soda. The patients had no history of abdominal surgery. Gastrostomy was associated with a mini tunneling in 5 patients. All patients were fed on the second day postoperative. We noticed two early leaks, one late leak (35 days postoperative), 1 button drop and an erosion of the balloon. The average hospital stay was 05 days (04 and 08 days). Three patients had a button change after an average time of 7 months (4 months and 8 months). Causes of change were an erosion of the balloon in 2 patients and a button fall in the last patient. Eight patients had spontaneous gastrostomy closure including the 7 caustic stenosis cases and lip and palate cleft after an average time of 05 months (04 months and 09 months). The closure was made spontaneously after the balloon deflation, the removing the button and the dressing. The average follow-up time was 13 months (6 months and 18 months). The 02 deaths reported in the series are independent of the gastrostomy. One patient died of an esophageal fistula from a blind dilation made with Savary dilators and the other died as a result of an esophageal replacement. We noted two patients who never stayed in touch. In the overall, parents were satisfied due to the discretion of the device which offers the child freedom to do activities and a greater level of comfort.
Discussion
Esophagus caustic burn is still common in our regions and affects children aged from 2 to 4 years with a slight male predominance. A previous study showed that a gastrostomy was performed in 18.3% after esophagus caustic burns. Because of the delays of medical visits, the children are received in the hospital at a sequelae phase of advanced esophagus stenosis including a severe malnutrition and dehydration [3]. The gastrostomy is then the emergency treatment done for these children to improve their general condition. In Western pediatric population, the most common indication is nutritional support for patients with chronic neurological problems [4,5]. Previously in our hospital the gastrostomy was performed using a Foley urinary catheter (Ch 18 or Ch 20) put in place by a laparotomy above the midline pathway of the umbilicus. Complications were mainly due to falls, internal migration, leakage, and wound complications such as suppuration or desertion [2,3]. Many teams adopted a less invasive approach to the realization of the gastrostomy feeding is now done using an endoscopic method, a radiological method or laparoscopic method causing fewer parietal trauma [6]. The endoscopy has the largest number of major complications, followed by laparoscopic technique. The open gastrostomy seems to be the safest [7]. Our surgical procedure looks like to the laparoscopic method concerning the size of the parietal opening while giving us a good accessibility to the stomach. The first elective less invasive method is interesting in our context because the main indication for gastrostomy in children is esophagus caustic stenosis, making it impossible to achieve endoscopic gastrostomy. The device used has also undergone a major step forward with the upgrade of the gastrostomy button [8]. These devices are easy to use and offer the child a freedom of movement and a comfortable life compared to the traditional catheters (Foley, Malecot, Pezzer) [6]. Many health centers continue to use Foley catheters in our country. This shouldn’t be the case today because of the risks of patients’ life incurring in chronic allergic sensitivity. The gastrostomy device is made with silicone to avoid this sensitivity. Complications found in the reports are dominated by peristomal leakage, balloon ruptures, infection and the appearance of granulation tissue around the gastrostomy port [9-12]. Antibiotic prophylaxis reduces the risk of infection and the application of silver nitrate used to solve the problem of wound healing [6,13]. The deterioration of the balloon is often the result of an inadequate quantity and quality of the liquid injected to fill it. The balloon must be filled with sterile water and not by the saline averaged 5cc [6]. The gastrostomy buttons help fight against the psychological problems related to altered body image especially in older children. The absence of a long catheter hanging out of the abdomen is a clear advantage. The button can improve the parents and children acceptance of the device.
Conclusion
The first elective gastrostomy feeding with the laparoscopy are the two less invasive techniques most relevant to our context since our main indication was a caustic stenosis of the esophagus.
References
- Grant JP (1988) Comparison of percutaneous endoscopic gastrostomy with Stamm gastrostomy. Ann Surg 207(5): 598–603.
- Ndour O, Fall FA, Ndoye NA, Sidibe S, Gassama F, et al. (2013) Indications for gastrostomy feeding in children: about 77 cases collected at the Pediatric Surgery center of Aristide Le Dantec Hospital in Dakar, Senegal. J Afr Hépatol Gastroentérol 7(3): 112-116.
- Mboup CA (2004) Evaluation of the management of the caustic stenosis esophagus in children: retrospective study about 49 cases collected at the Pediatric Surgery center of Aristide Le Dantec Hospital. Thesis Med, University of Dakar, Senegal, N°06.
- El-Matary W (2008) Percutaneous endoscopic gastrostomy in children. Can J Gastroenterol 22(12): 993-998.
- Catto-Smith AG, Jimenez S (2006) Morbidity and mortality after percutaneous endoscopic gastrostomy in children with neurological disabilities. J Gastroenterol Hepatol 21(4): 734-738.
- Vasseur Maurer S, Reinberg O (2015) Laparoscopic technique to perform a true Stamm gastrostomy in children. J Pediatr Surg 50(10): 1797-1800.
- Liu R, Jiwane A, Varjavandi A, Kennedy A, Henry G, et al. (2013) Comparison of percutaneous endoscopic, laparoscopic and open gastrostomy insertion in children. Pediatr Surg Int 29(6): 613-621.
- Gauderer MW, Ponsky JL, Izant RJ (1980) Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg 15(6): 872–875.
- Rothenberg SS, Bealer JF, Chang JHT (1999) Primary laparoscopic placement of gastrostomy buttons for feeding tubes. Surg Endosc 13(10): 995-997.
- Ruangtrakool R, Ong TH (2000) Gastrostomy button: clinical appraisal. J Med Assoc Thai 83 (8): 839-849.
- Ségal D, Michaud L, Guimber D, Ganga-Zandzou PS, Turck D, et al. (2001) Late-onset complications of percutaneous endoscopic gastrostomy in children. J Pediatr Gastroenterol Nutr 33(4): 495-500.
- Ackroyd R, Saincher M, Cheng S, El-Matary W (2011) Gastrostomy tube insertion in children: The Edmonton experience. Can J Gastroenterol 25(5): 265-268.
- Launay V, Gottrand F, Turck D, Michaud L, Ategbo S, et al. (1996) Percutaneous Endoscopic Gastrostomy in Children: Influence on Gastroesophageal reflux. Pediatrics 97(5): 726-728.






























