Neonatal Lupus with Severe Multisystem Organ Involvement: An Exceptional Presentation of an Uncommon Disease
Marie-Amelyne Le Rouzic1*, Lénaïg Abily-Donval1, Stéphane Marret1, Xavier Balguerie2 and Caroline Lardennois1
1 Department of Neonatology and Neonatal Intensive Care Unit, Rouen University Hospital, France
2Department of pediatric dermatology, Rouen University Hospital, France
Submission: March 01, 2017;; Published: April 03, 2017
*Corresponding author: Marie-Amelyne Le Rouzic, Department of Neonatology and Neonatal Intensive Care Unit, Rouen University Hospital, 1 rue de Germont, Rouen, France.
How to cite this article: Marie-Amelyne L R, Lénaïg A-D, Stéphane M , Caroline L. Neonatal Lupus with Severe Multisystem Organ Involvement: An Exceptional Presentation of an Uncommon Disease. Acad J Ped Neonatol. 2017; 4(2): 555688. DOI: 10.19080/AJPN.2017.04.555688
Abstract
Neonatal lupus is a rare autoimmune disease associated with autoantibodies transmitted from the mother by passive transplacental passage and which can affect the fetus. We report the case of a newborn infant with neonatal lupus who displayed a severe multisystem organ involvement, the effects of which began in utero. His levels of autoantibodies were high at birth and exchange transfusion was performed in an attempt to lower them: this therapy enabled to improve his skin lesions and his respiratory and hematological condition in a few days’ time with a proven decrease with the levels of autoantibodies afterwards. He was discharged at age 27 days with subnormal biological parameters and only residual atrophic skin lesions. Although exchange transfusion quickly improved this child’s condition, convincing evidence for efficacy of exchange transfusion requires further corroboration and supplementary studies are needed to conclude with certainty on the effects of treatments aiming at decreasing the levels of autoantibodies.
Keywords: Neonatal lupus; Multisystem organ involvement; Maternal follow-up; Exchange transfusion
Abbrevations: NL: Neonatal Lupus; HFNC: High-Flow Nasal Canula; SLE: Systemic Lupus Erythematosus
Introduction
Neonatal lupus (NL) is a rare autoimmune disease, caused by passive transplacental passage of maternal IgG autoantibodies to the infant. NL is a multisystem disease and severe complications may occur. Cardiac involvement is the most frequent complication, as half of the affected neonates have congenital heart block [1]. Skin involvement is present in 15-25% of children with NL [2]. Hepatitis, hematologic abnormalities, pulmonary and neurological involvement may also less frequently occur.
We report here on a patient with NL who displayed a severe multisystem organ involvement, including cutaneous, hematological, pulmonary, splenic and hepatic manifestations, the effects of which began in utero. The antenatal and simultaneous occurrence of all these complications is very rare and may be considered as an exceptional and unusual presentation.
Case Presentation
A 25-year-old primigravida woman was referred to our hospital after sonographic assessment of suspected fetal anemia at 37 weeks of amenorrhea. She was affected by Sjögren’s syndrome with positive anti-SSA and anti-SSB antibodies and treated with hydroxychloroquine and prednisone during her pregnancy. Ultrasound showed estimated weight at the 8th percentile with normal umbilical Doppler flow velocities, accelerated middle cerebral artery flow velocity, splenomegaly and cardiomegaly with pericardial effusion. Previous antenatal ultrasounds were normal, including repeated echocardiographic examinations with no congenital heart block.
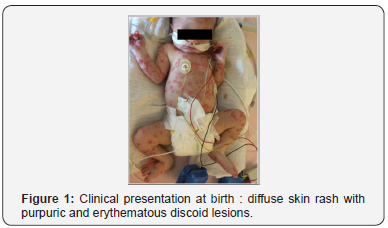
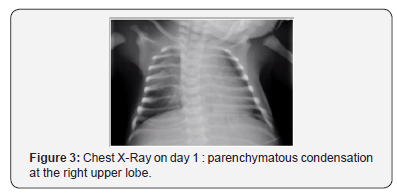
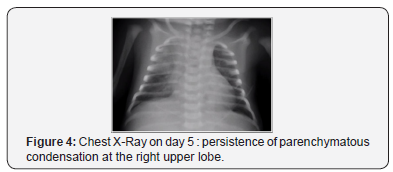
A full-term male infant weighing 2450g (<3rd percentile), with 1- and 5- minutes Apgar scores of 9 and 10 respectively, was born via planned caesarian section at 38 weeks. Physical examination in the delivery room showed diffuse skin rash with purpuric and erythematous discoid lesions with no mucosal involvement (see Figure 1 & 2). Some lesions were desquamative. He was also found with an enlarged spleen, measuring 7 cm below the left costal margin, and a mild hepatomegaly. A few minutes after birth, the patient developed respiratory distress syndrome and high-flow nasal cannula (HFNC) oxygen therapy was introduced. Chest x-ray showed parenchymatous condensation at the right upper lobe (see Figure 3 & 4). His electrocardiogram did not reveal heart block and his echocardiography showed pericardial effusion and no cardiomegaly. Concerning his biological parameters, hemoglobin concentrations were 12.7 and 12.8g/dL in the cord and peripheral blood, respectively. His complete blood count revealed a thrombocytopenia at 23G/L without hemorrhagic symptoms and a platelet transfusion of 10ml was performed. The rest of his laboratory evaluation showed hepatic cytolysis, cholestasis and stigmata of hemolysis with increased reticulocyte count (160G/L), elevated lactate dehydrogenase (1916UI/L) and collapsed haptoglobin (<0.10g/L). Our patient was screened for viral infections, including Cytomegalovirus, Epstein-Barr Virus, Herpes Simplex Virus, Varicella Zoster Virus, Parvovirus B19, Coxsackie Virus, rubella and toxoplasma. All serologic tests proved negative. Anti-SSA/Ro antibodies and anti-SSB/La antibodies were detected in our patient (115.5CU and >1550CU respectively). A fluorescent test for antinuclear antibody was also positive at titer >1200CU (speckled-nucleolar pattern). Nuclear RNP, Sm, Slc-70 and Jo-1 antibodies were absent. These high levels of anti-SSA and anti-SSB antibodies leaded to the diagnosis of neonatal lupus with a highly probable mother-to-child transmission of these autoantibodies.

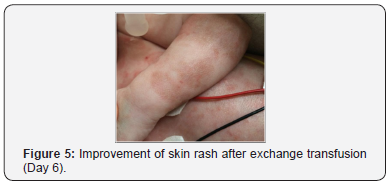
When he was three days-old, our patient was treated with exchange transfusion in an attempt to lower autoantibodies levels. He received another platelet transfusion at the end of the exchange. A significant decrease in anti-SSA antibodies was observed (25.3 CU) but the concentration of anti-SSB antibodies still exceeded the established upper limit of linearity for the assay (>1550CU). Due to persistent thrombocytopenia, he was treated with intravenous gammaglobulin (1 g/kg/day) for two days.

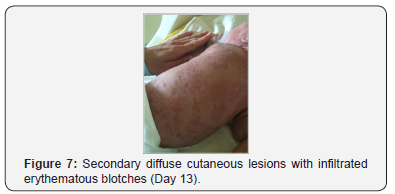
When the patient was thirteen days-old, he presented secondary diffuse cutaneous lesions with infiltrated erythematous blotches (see Figure 7), different in aspect from the skin lesions present at birth, associated with an increase of his splenomegaly (5cm below the left costal margin). Laboratory parameters showed a slight decrease in platelet count (from 115G/L to 94G/L) and an elevated C-reactive protein (up to 71mg/L). Skin lesions improved within a few days but splenomegaly remained stable. Topic therapy with hydrocortisone was started and performed for four days just before he was discharged from hospital at age 27 days. The electrocardiogram remained normal and a control of the echocardiography showed a normal heart with disappearance of the pericardial effusion. Laboratory parameters before discharge revealed the following data: hemoglobin 12g/dL, hematocrit 0.36, white blood cell count 15.2G/L, platelet count 74G/L, ASAT 45UI/L, ALAT 37UI/L, GGT 945UI/L, ALP 276UI/L, bilirubin 10μmol/L.
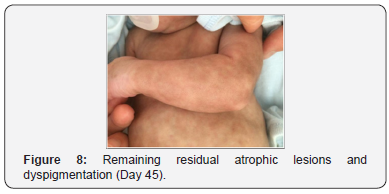
By the time the infant reached 3 months of life, the test for anti-SSA/Ro antibodies was completely negative, the test for anti- SSB/La antibodies was still positive at titer 847.1CU and liver function tests had returned to normal. However, he still presented dyspigmentation and some residual atrophic lesions (see Figure 8).
Discussion
Neonatal lupus (NL) is a rare autoimmune condition and only 1.5% to 2% of neonates develop the disease if the mother has autoantibodies [3]. The first case of neonatal lupus with cutaneous involvement was described by McCuistion and Schoch in 1954 [4]. Skin lesions are the dominant features in the majority of NL cases [5] and usually present at up to 6 weeks of life or later [6] but some lesions may be congenital, as in our case. Cutaneous lesions are transient and usually resolve within four to six months when maternal autoantibodies disappear [7]. However, a few cases of persistent telangiectasia, atrophy or pigmentation have been reported [8]. No skin biopsy was necessary in our patient (as the diagnosis was confirmed with high serum antibody levels based on maternal history) but differential diagnoses including congenital infections were discussed while waiting for the immunological results. Neonatal skin rashes due to bacterial or viral infections are common as the barrier between the mother and the fetus is not completely impermeable [9]. Our patient was systematically screened for TORCH infections (Toxoplasmosis, Other infections, Rubella, Cytomegalovirus, Herpes simplex virus), especially as his mother had a CMV serology with a dubious pattern (IgM-detection of borderline significance). All tests finally proved negative but this illustrates the absolute need to search for infections when confronted to a neonatal skin rash.
The most dangerous complication of NL is congenital heart block, especially irreversible third-degree heart block which must require pacing. It can present in utero or after birth. Monitoring with serial fetal echocardiography is recommended to start at 16 weeks of gestation [10] in order to implement a treatment in utero if necessary. Our patient was regularly monitored and no congenital heart block was found. As described above, his mother was treated with hydroxychloroquine. A study by Izmirly et al concluded that exposure to prenatal hydroxychloroquine in mothers with systemic lupus erythematosus (SLE) may decrease the risk of cardiac manifestations of NL [11]. In any case, a regular antenatal monitoring of the fetal heart rate along with echocardiography is recommended to screen for congenital heart block in pregnant women with known SLE or Sjögren’s syndrome [12].
Jaeggi et al. [13] showed a correlation between the level of autoantibodies and the development of cardiac NL anomalies and this was our rationale for performing an exchange transfusion. To our knowledge, this is the first case described in literature treated with exchange transfusion with a proven decrease in the levels of autoantibodies associated with a rapid decrease in cutaneous manifestations whereas skin lesions are usually described as dissipating within four to six months after birth. However, there are not enough evidence to conclude with certainty on the role of the exchange transfusion in the reduction of symptoms presented by our patient.
Hematologic manifestations (hemolytic anemia, thrombocytopenia or neutropenia) are rare and usually infraclinic. Hepatic and splenic manifestations may also occur. Like cutaneous manifestations, they are usually transient (as in our case) and should need no further treatment [14].
Pulmonary manifestations are extremely rare and have been occasionally reported in this pathology [15]. In these few cases, pneumonitis was transient. As for our patient, he presented oxygendependent respiratory distress syndrome along with radiological manifestations that resolved in 10 days’ time. Neonatal lupus was suspected to be responsible for the lung involvement because the symptoms began right at birth and because there was no other proven etiology to explain the clinical picture.
Neonatal lupus is a multidisciplinary challenge, especially when children present multisystem organ involvement. Outcomes can vary among patients [5] and the prognosis depends upon the cardiac involvement. Long-term follow-up is compulsory as these patients are at risk of developing an autoimmune disease in their lifetime [10]. Further studies are needed to evaluate the effects of treatments which would decrease the levels of autoantibodies. This uncommon presentation enables to underline the need for mothers to be followed-up closely during their pregnancy to detect and prevent the possible fetal and neonatal complications.
Consent
Informed parental consent was obtained for publication of data.
References
- Kuy RK, Tae YY (2009) A case of Neonatal Lupus Erythematosus Showing Transient Anemia and Hepatitis. Ann Dermatol 21(3): 315- 318.
- Silverman E, Jaeggi E (2010) Non-Cardiac Manifestations of Neonatal Lupus Erythematosus. Scand J Immunol 72(3): 223-225.
- Smyth A, Garovic V (2009) Systemic lupus erythematosus and pregnancy. Minerva Urol Nefrol 61(4): 457-474.
- Mc Cuistion CH & Schoch EP (1983) Possible discoid lupus erythematosus in a new born infant. Report of a case with subsequent development of acute systemic lupus erythematosus in mother. Arch Dermatol 119(7): 615-618.
- Johnson B (2014) Overview of Neonatal Lupus. J Pediatr Health Care 28(4): 331-341.
- Inzinger M, Salmhofer W, Binder B (2012) Neonatal lupus erythematosus and its clinical variability. J Dtsch Dermatol Ges.. 19(6): 407-410.
- Tincani A, Nuzzo M, Motta M, Zatti S, Lojacono A, et al. (2006) Autoimmunity and pregnancy: autoantibodies and pregnancy in rheumatic diseases. Ann N Y Acad Sci 1069: 346-352.
- Shahian M, Khosravi A, Anbardar MH (2011) Early cholestasis in neonatal lupus erythematosus. Ann Saudi Med 31(1): 80-82.
- Jones L & Wilson D (2011) Hematological problems in the fetus and neonate. In: Martin R, Fanaroff A, Walsh M (Eds.), Fanaroff & Martin’s neonatal-perinatal medicine: Diseases of the fetus and infant. Mosby, St. Louis, MO, USA, pp. 1303-1360.
- Lee LA (2009) The clinical spectrum of neonatal lupus. Arch Dermatol Res 301(1): 107-110.
- Izmirly PM, Kim MY, Llanos C, Le PU, Guerra MM, et al (2010) Evaluation of the risk of anti-SSA/Ro-SSB/La antibody-associated cardiac manifestations of neonatal lupus in fetuses of mothers with systemic lupus erythematosus exposed to hydroxychloroquine. Ann Rheum Dis 69(10):1827-1830.
- Tincani A, Rebaioli CB, Taglietti M, Shoenfeld Y (2006) Heart involvement in systemic lupus erythematosus, anti-phospholipid syndrome and neonatal lupus. Rheumatology. 45(4): 8-13.
- Jaeggi E, Laskin C, Hamilton R, Kingdom J, Silverman E (2010) The importance of the level of maternal anti-Ro/SSA antibodies as a prognostic marker of the development of cardiac neonatal lupus erythematosus a prospective study of 186 antibody-exposed fetuses and infants. J Am Coll Cardiol 55(24): 2778-2784.
- Feki S, Turki A, Frikha F, Hachicha H, Walha L, et al. (2015) Neonatal lupus and maternofetal transmission of anti-SSA/Ro and anti-SSB/la antibodies. Arch Pédiatr 22(2): 154-159
- Fonseca E, Contreras F, Garcia-Frias E, Carrascosa MC (1991) Neonatal lupus erythematosus with multisystem organ involvement preceding cutaneous lesions. Lupus. 1(1): 49-50.






























