Gross Hematuria Post-Pieloplasty as Single Manifestation of Primary Renal CandidiasisM
Pacheco-Mendoza Byron A1*, David Mejía-Camacho2 and Realpe1
1Deparment of Pediatric Surgeon and Pediatric Urology, Centro Médico Nacional “20 de Noviembre” ISSSTE, Mexico
2 Deparment of Pediatrics, Hospital General de Cabo San Lucas, Mexico
Submission: February 05, 2016; Published: March 28, 2017
*Corresponding author: Byron Alexis Pacheco-Mendoza, Monrovia 302-206, Portales Norte, Benito Juárez, 06720, Mexico City, Mexico.
How to cite this article: Pacheco-Mendoza B A, David M, Realpe. Gross Hematuria Post-Pieloplasty as Single Manifestation of Primary Renal Candidiasis. Acad J Ped Neonatol. 2017; 4(4): 555685. DOI: 10.19080/AJPN.2017.04.555685
Abstract
Primary Renal Candidiasis (PRC) has been described in pre-term and term newborn hospitalized in neonatal intensive care units (NICU). A risk factor for PRCis hydronephrosis. The aim of this paper is to present the case of a toddler suffering from PRC without hospitalization in intesive care units, and with gross hematuria pospieloplasty
A 3 year-old male was admitted in the hospital with fever and gastroalimentary vomiting. The diagnosis of hydronefrosis by ureteropelvic junction obstruction was established. Treatment with ceftriaxone and nephrostomy guided by ultrasonography (US) was applied. Three months later, pyeloplasty and pigtail placement were carried out. Two weeks after postpyeloplasty, the patient presented gross hematuria, with secondary anemia (Hb 6.5g/dl). Urine cultures positive for Candida albicans. US renal report fungoma of 7x5mm in left kidney. Management was done with fluconazole at 6 mg/kg/day by 6 weeks. Currently asymptomatic.
Keywords: Gross hematuria; Renal candidiasis; Pyeloplasty
Abbrevations: PRC: Primary Renal Candidiasis; US: Ultrasonography; KBUS: Kidney-Bladder-Ultrasonography; APD: Anterior-Posterior Diameter; NORA: Normalised Residual Activity; DRF: Differential Renal Function
Introduction
Primary renal candidiasis (PRC) has been described previously [1]. Preterm newborn have risk factors for developing systemic or non-systemic candidiasis, because they are subject to intravenous broad spectrum antibiotics, parenteral nutrition, central venous catheters; among other factors. An important history in these patients is the presence of hydronephrosis [2].
The main clinical manifestation reported in the PRC has been anuria or oliguria secondary to mycetomas, fungomas obstructing the ureteropelvic junction, especially in pre-term patients [3,4].
The aim of this paper is to present the case of a toddler with PRC manifested by gross hematuria pospyeloplasty and being an outpatient.
Case Report
A 3 year-old male patient, no report of prenatal hydronephrosis, with no relevant prenatal and perinatal history. Fever of 39 °C, 48 hours of evolution and gastroalimentary vomiting.
Physical examination
Palpable mass on the left flank, painful, mobile, non-stony.
Laboratories
Hematic biometry: Leukocytes 16,340/ul, neutrophils 88%. Blood chemistry: Serum creatinine 0.26 mg / dl. Uroanalysis: Leukocyte sterease (+), countless leukocytes.
Work-up
Kidney-Bladder-Ultrasonography (KBUS): Left kidney with severe hydronephrosis with pelvis of 350 ml, anterior-posterior diameter (APD) pelvic of 75mm, renal parenchyma thinned (4mm).
Diuretic renography with 99mTcMAG-3: Normalised residual activity (NORA) at 60 minutes>1 in the left kidney with 39% of differential renal function (DRF).
Based on these results, we decided to perform nephrostomy and intravenous (IV) treatment with ceftriaxone for 14 days, thus resolving the infectious condition.
Three months later, Anderson Hynes pyeloplasty and pigtail catheter placement were performed. After 24 hours postsurgery, yhere were no complications, no incidents or accidents.
Evolution
After two weeks post-pyeloplasty, he presents gross hematuria with clots, without abdominal pain. During physical examination with heart rate (HR) of 125bpm, abdomen without bleeding in surgical wound, no hematomas, no palpable mass.
Laboratories
Hb: 6.5g/dl, hematocrit 19%, leukocytes 4300/ul, platelets 188,000/ul TP: 14.2, TTPa: 38.5, Urine culture: 48-hour without bacterial growth.
Work-up
KBUS with APDpelvic of 48 mm, no evidence of renal pelvic clots, no retroperitoneal extra-renal collections.
We decided to hospitalize with absolute rest, red blood cells were transfused; he was discharged from hospital at 48 hours without hematuria.
After 8 weeks post-pyeloplasty, a pigtail catheter was removed by cystoscopy.
After 10 weeks post-pyeloplasty, there was gross hematuria again, without clots, without symptomatic anemia.
Laboratories
Urinalysis: countless haematocytes, no crenocytes, no urine proteins. Urine culture: Report at 48 hours candida albicans.
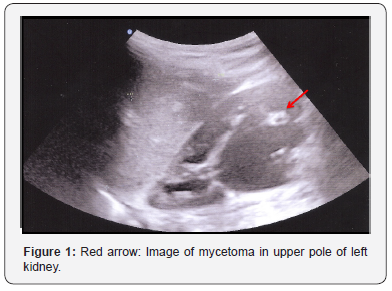
Abdominal US to search fungomas: Two hyperechoic images in left renal parenchyma of 7x5 mm and 3x3 mm, without acoustic shadow suggestive of mycetomas (Figure 1).
\
Doppler echocardiogram: Normal
Management with fluconazole 7 days IV and then 5 weeks oral.
Actually in the last follow-up at 12 months after the antifungal treatment, the patient was asymptomatic with negative urinalysis and urine cultures, KBUS with residual image of 3x4mm in left kidney.
Discussion
PRC has been reported in term infants [5], preterm infants [6] and, infants [7], commonly in intensives care units; but we do not know of reports in a toddler as in the case that we are reporting.
Due to the use in the intensive care rooms, of broad spectrum antibiotics, intravascular devices and parenteral nutrition, among other factors, fungic systemic or localized infections have been increasing [8,9]. But our patient does not belong to this group of inpatients; he is a patient diagnosed from the outpatient clinic. Most of the reported cases of PRC in children have as a common denominator, the presence of ipsilateral hydronephrosis [10], similar to our patient; but also we added a risk factor that was the use of nephrostomy for 3 months, which undoubtedly contributed to the colonization of the kidney by candida.
PRC can manifest as pyelonephritis and/ or mycetomas [11]. In children we do not know of reports of pyelonephritis (PN) as the only manifestation, but we do of PN plus mycetomas [10], or mycetomas at the ureteropelvic junction causing anuria or oliguria [12,13]. The patient in the study, did not have obstruction of the urinary tract, he had gross hematuria with acute anemia. We found reports in adults of macroscopic hematuria in PRC [14], but according to the review in the world literature this is the first case reported with this clinical manifestation in toddler.
The diagnosis of PRC has been established by ultrasonography (US), retrograde pyelography, excretory urography, anterograde pyelography and tomography [15]. The most used method is the US. We established the diagnosis by US, and also followed up with US.
The treatment of primary renal candidiasis is based on antifungal agents, the mostly used are fluconazole, amphotericin and flucytosine [16,17]; we used fluconazole for 6 weeks with complete resolution of symptom and mycetomas.
For the cases of obstructive uropathy secondary to mycetomas, several treatments have been described, such as percutaneous nephrostomy [18], percutaneous extraction of mycetomas with thrombectomy devices [19]; none of these procedures was necessary to use in our patient; gross hematuria finished with oral fluconazole treatment.
Conclusion
This is the first report of a child with primary renal candidiasis, manifested with anemising gross hematuria post-pyeloplasty. We present this manifestation of primary renal candidiasis to be considered in the differential diagnosis of a patient with hematuria and history of pyeloplasty with chronic use of nephrostomy.
References
- Brown GC, Magargal LE, Shields JA, Goldberg RE, Walsh PN (1981) Retinal arterial obstruction in children and youngadults. Ophthalmol 88(1): 18-25.
- Manayath GJ, Shah PK, Narendran V, Morris RJ (2010) Idiopathic pediatric retinal artery occlusion. Indian J Ophthalmol 58(2): 151-152.
- Arevalo D, Melo Granados E, Cortes S, Paez A, Soria C (2016) Hemiretinal Artery Occlusion in an 11-Year-OldChild with Dextrocardia. Case Reports in Ophthalmological Medicine 2016: 1-3.
- Monagle P (2005) Thrombosis in children with BT shunts, Glenns and Fontans. Progress in PediatricCardiology 21(1): 17-21
- Knoop K, Trott A (1994) Ophthalmologic procedures in the emergency department--Part I: Immediate sight-saving procedures. Acad Emerg Med 1(4):408-412
- Hayreh SS, Jonas JB (2000) Optic disk and retinal nerve fiber layer damage after transient central retinal artery occlusion: an experimental study in rhesusmon keys. Am J Ophthalmol 129(6): 786-795.
- Schmidt DP, Schulte-Monting J, Schumacher M (2002) Prognosis of central retinal artery occlusion: local intraarterial fibrinolysis versus conservative treatment. AJNR Am J Neuroradiol 23(8): 1301-1307.






























