Periodontal and Restorative Treatment Approach to Gingival Recession Associated with Non-Carious Cervical Lesion: Report of Three Cases
Rania Gargouri1, Héla Jegham2*, Rym masmoudi2 and Mohamed Bassem khattech2
1Department of Periodontology, Faculty of Dental Medicine, University of Monastir, Monastir, Tunisia
2Military Hospital of Instruction of Tunis, Department of Medicine and Dental Surgery Mont Fleury- 1008 Tunisia
Submission: March 27, 2023; Published: April 10, 2023
*Corresponding author: Héla Jegham, Military Hospital of Instruction of Tunis, Department of Medicine and Dental Surgery Mont Fleury- 1008 Tunisia
How to cite this article: Rania Gargouri, Héla Jegham*, Rym masmoudi and Mohamed Bassem khattech. Periodontal and Restorative Treatment Approach to Gingival Recession Associated with Non-Carious Cervical Lesion: Report of Three Cases. Adv Dent & Oral Health. 2023; 16(1): 555931. DOI: 10.19080/ADOH.2023.16.555931
Abstract
Gingival recession (GR) is a common problem in the world population that can induce aesthetic complaints and dentin hypersensitivity. It is often complicated by dental substance wear at the gingival third of the tooth due to reasons other than dental caries. This condition is described as a non-carious cervical lesion (NCCL). If a NCCL is present in a site with gingival recession, the muco-gingival condition is defined as a combined defect (CD). Thus, a multidisciplinary approach should be considered for the treatment of this condition which includes muco-gingival surgery and the reconstruction of the cemento-enamel junction. Zucchelli et al. proposed a treatment strategy based on the position of the Maximum root coverage (MRC) and the NCCL location and extent. The aim of this article is to review the treatment protocols regarding a CD and present the different steps of the management of three clinical cases.
Keywords: Case report; Gingival recession; Cemento enamel junction; Tooth abrasion; Surgery
Abbreviations: GR: Gingival recession; NCCL: Non-carious cervical lesion; CD: Combined defect; MRC: Maximum root coverage; CEJ: Cemento-enamel junction
Introduction
According to the Glossary of Periodontal Terms [1], gingival recession [GR] is defined as the location of the gingival margin apical to the cemento-enamel junction (CEJ). It is associated with attachment loss due to the migration of the whole periodontal attachment apparatus [gingiva, periodontal ligament, and alveolar bone]. These defects are greatly prevalent worldwide, affecting from 40% to 100% individuals [2,3]. This common problem leads to root exposure, therefore favoring root caries, non-carious cervical lesions, dentin hypersensitivity, poor plaque control and compromising aesthetics. Moreover, if left untreated, GR has a high risk of progression over time. Due to these issues, many patients seek gingival recession treatment [2]. GR defects have multifactorial causes; Trauma from improper toothbrushing and low plaque control have been proposed as the main triggers of this disease in the presence of various predisposing factors including a thin periodontal biotype, the absence of attached gingiva, tooth malposition and iatrogenic factors such as uncontrolled orthodontic movement and defective restorations [4]. After examining 1010 GR defects, Pini-Prato reported that only 46% of the considered root surfaces were intact, with an identifiable CEJ and absence of cervical wear. Consequently, it has been reported that cervical abrasion was observed in about 50% of the examined teeth with gingival recessions [5].
Based on this finding, the new classification of the muco-gingival conditions of the 2017 World Workshop proposed a treatment-oriented classification including gingival recession severity, gingival phenotype and the presence of associated cervical lesion. In a first step, the interdental clinical attachment level is determined with reference to a new classification system (Cairo 2011) [6], then, the gingival phenotype which includes gingival thickness and keratinized tissue width is examined. Following this, the condition of the tooth surface in the area of the gingival recession is evaluated. Since NCCLs are common findings in patients with gingival recession defects, a classification of these defects has been introduced [5]. A tooth with an identifiable CEJ belongs to class A, while one with no identifiable CEJ belongs to class B. Each class is subdivided depending on the presence (+) or absence (-) of a cervical step over 0.5 mm, yielding four classes (A+, A-, B+, B-).
Tooth position, aberrant frenum, and the number of the adjacent recessions are also features contributing to the description of the site. It is assumed that GR and NCCL may share the same etiologic factors. Although an abrasion, due to mechanical forces, plays an important role in the development of NCCLs, it is not the unique cause, other factors such as corrosion, and possibly abfraction may be involved. Frequently, as a misdiagnosis, restorative procedures are adopted as the only treatment of these cervical lesions leading to marginal bleeding, attachment loss and the increase of the gingival recession. A decision-making process to facilitate the treatment of GR associated with NCCLs was proposed based on the topography of the NCCL and its relationship with the maximum root Coverage [MRC] achievable by mucogingival procedures. The aim of this report is to discuss, through three clinical cases, the different steps of restorative and/or surgical phases for treating GR associated with NCCL based on Zucchelli’s decision making process for treating NCCLs associated with gingival recessions.
First Case
A 56-year-old female patient, in good general medical condition, nonsmoker, complained of root exposure on her frontal maxillary teeth and a cervical abrasion of the upper canines, causing plaque retention and increased sensitivity (Figure 1). The patient expressed her desire to regain the previous position of her gingiva. At clinical examination, multiple adjacent buccal recessions were found on the four maxillary incisors and canines. The profile visual inspection of the left and right canine confirmed the presence of a NCCL concomitant to the GR (Figure 2). The patient was asked about her tooth-brushing and dietary habits. She revealed that she brushes her teeth horizontally with excessive force. After the exclusion of a traumatic occlusion and data analysis, the main contributing factors were thin gingival biotype and improper tooth-brushing. Full mouth radiographs, periodontal charting and photographic documentation were carried out.


With the use of a periodontal probe, a thorough clinical examination of the hard tissues showed:
A deep crown radicular defect on the right canine and a less deep crown radicular defect on the left canine: Class B+ defects; A complete disappearance of the CEJ was observed on both teeth with the presence of a step >0,5mm. A mild rotation was observed on both lateral incisors.
Regarding the soft tissues: GR RT2 on the incisors and the upper canines and a sufficient band of keratinized tissue was present apically to the gingival margins.
Afterwards, the patient was informed about the treatment plan which was the following:
i. Initial therapy includes first etiologic factors management: the modified bass brushing technique was demonstrated to the patient, a soft toothbrush and a nonabrasive tooth-paste were prescribed.
Second; a session of scaling and professional tooth cleaning was performed with the use of a polishing paste.
ii. A reevaluation session was then scheduled to assess the supragingival plaque control and the tooth brushing technique.
The patient was compliant with the instructions and well prepared for the treatment of the cervical and recession defect. The restorative and surgical procedures were performed during the same session by two clinicians of the Departments of Conservative Dentistry and Periodontology. The key step in the combined approach is the determination of the MRC line. It is the line that represents the limit for apical preparation of the conservative restoration [7]. In fact, the MRC is considered to be the clinical CEJ both in the upper canines where the anatomical CEJ disappeared and also in the incisors where the conditions for a complete root coverage are not present: malposition of the lateral incisors, interdental attachment loss. Therefore, prior to the restoration, this curved line was calculated for each affected tooth and marked by means of a dental pen. On the left and right canine, the MRC was located in the deepest portion of the NCCL (Zucchelli’s Type 3 defect) separating the defect into a coronal area treated by a resin restoration and an apical area treated by coronally advanced flap for multiple gingival recession and a CTG placed on the right and left maxillary canines to avoid the collapse of the flap on the cervical lesion (Figure 3).

Restorative Procedures

Following local anesthesia, a gingival cord was inserted to isolate the restoration field on the canines. The area located coronally to the MRC was prepared with diamond burs removing the superficial dentin. Mild enameloplasty was also done to reduce the depth of the defect (Figure 4). The aims of this crown odontoplasty were to obtain an emergence profile compatible with periodontal health, preventing plaque accumulation and pseudo pocketing and to increase the retention of the resin by creating a beveled surface. After Adhesive procedures, the conservative therapy is then performed by applying fluid resin to the level of the MRC and a thorough finishing and polishing made sure of a smooth surface condition (Figure 5).

Surgical Procedures
As illustrated above, the NCCL defects on the canines are combined with multiple adjacent recessions. The surgical technique was the coronally advanced envelope flap (Zucchelli) underneath which a CTG was applied specifically on both canines. Under local anesthesia, the incision design consisted in paramarginal incisions to create surgical papillae followed by intrasulcular incisions, a distal and mesial vertical releasing incisions. The flap was raised with the split-full-split technique and a deep and superficial incisions were performed in order to release the muscle insertions and to coronally advance the flap (Figure 6). A deepithelization of the anatomical papillae was made by using surgical scissors and a CTG was harvested from the palate and applied on the canine’s defects, the flap was advanced and sutured 1mm coronal to the MRC with sling sutures (Figure 7 & Figure 8).



Results
The GM was coronally advanced to the level of the MRC on the incisors, as for the canines, the advanced tissues and the CTG were filling the NCCL defect and merged with the cervical restoration. Follow up results are illustrated in the figures (Figure 9 & Figure 10).


Second Case
A 40-year-old patient in good general medical condition, nonsmoker, consulted after complaining from hypersensitivity related to defective resin restorations on the left maxillary premolars. After clinical examination, old cervical resin restorations were partially covering a NCCL located on the 24 and 25, RT1 GR was also concomitant to the defects. A wide band of keratinized tissue was present apically to the recessions (Figure 11). After one session of initial therapy, a combined approach was decided since the cervical abrasions involved the root and crown area resulting in the disappearance of the CEJ (B+ defects). In fact, restorative therapy alone will result in a long crown and an apical position of the GM which is esthetically unfavorable. The MRC was calculated (type 3 defect) and the restoration of the coronal part of the defect was performed by means of fluid resin (Figure 12) After the finishing and polishing of the restoration, the root coverage procedure was achieved. The surgical technique consisted of a coronally advanced flap after marginal incision and deepithelization of the anatomical papillae (Figure 13).



Results
There was a decrease in hypersensitivity with acceptable esthetic results. The GM was coronally advanced demonstrating the complete coverage and the successful restoration of the defects (Figure 14 & Figure 15).


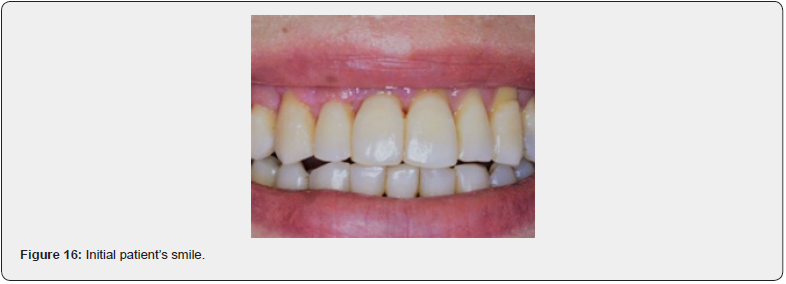
Third case
A female patient, nonsmoker and in a good general condition complained from poor smile aesthetics related to root exposures on her frontal maxillary teeth accentuated on her left and right canines (Figure 16). The clinical examination revealed RT2 recessions and non-carious cervical lesion on the left canine confined to the root of the tooth (Figure 17). The treatment approach was periodontal only, as the lesion was exclusively radicular. Zucchelli’s envelope flap was performed, and a connective tissue graft was placed at the level of 21, 22 and 23 (Figure 18-20).




Results


Discussion
Treatment of combined defects are challenging since, in these cases, the surgical root coverage does not achieve complete defect coverage resulting in persistence of dentin hypersensitivity and plaque retention, and the restorative treatment, when performed alone, yields to unesthetic long tooth. The combined restorative and periodontal approach were a subject of numerous studies. In fact, Santamaria et al proved in their two Randomized clinical trials, that reconstructing the whole damaged cervical area with a filling material such as modified glass ionomer and performing a CAF or CAF + CTG is a feasible and efficacious approach since the restorative material did not interfere with the root coverage outcome, and the coronal part of the defect that could not be managed with a CAF alone, is then restored. This induced the complete resolution of hypersensitivity [8-10]. These findings were confirmed in a recently published systematic review and meta-analysis by Gennai et al. [11]; indeed, the restoration of NCCL provides better outcomes for the reduction of Dentin hypersensitivity, which can be explained by obturation of the dentinal tubules by the material alone [complete restoration] or by the material and the root coverage (partial restoration + CTG).
Although histologic studies showed that the soft tissues can adhere to the subgingival resin composite or modified glass ionomer [12], Zucchelli argued that it was not biologically acceptable to restore a part of the root that was once covered with soft tissues [13]. Moreover, alteration of the complete restoration overtime due to discoloration, bacterial infiltration or material wear, complicates the reintervention. Gennai et al. [11] mentioned that the advantage of the partial restoration approach is the decreased risk of restoration detachment and/ or marginal deterioration and the ease of replacing or removing the restoration, as only a minimum portion is covered by the gingival tissue. In consideration of this, the classification of NCCLs, bringing forward an algorithm-based treatment, was proposed by Pini-Prato et al. [5] followed by Zucchelli’s NCCL types exposed in his case series [7].
In this latter, the rationale was that only the part of the CD that will not be covered by the soft tissues will be restored. Therefore, prior to the restoration, it is essential to relocate the lost CEJ or determine the MRC line in order to identify the apical limit of the partial restoration. Although deemed to be subjective and difficult in teeth without intact CEJ [11], The MRC line is an effective method in predicting the final position of the coronally advanced tissues and avoiding mistaking the abrasion line for the CEJ [14]. It is calculated by first measuring the ideal papilla height, from the contact point to the proximal CEJ of the tooth. This coronal reference point is easily detected when the interdental papilla is elevated with the use of a probe. Once this measurement is taken, this distance is reported starting from the actual tip of each papilla. The MRC is then predetermined by connecting with a scalloped line the projection of this distance on the recession margin [12].
Based upon the topographic relationship between the MRC and the NCCL, 5 treatment alternatives to 5 NCCL types were introduced:
If the lesion concerns the root surface only [NCCL types I and II], the adequate treatment is the periodontal surgical approach. Whereas NCCLs occurring coronally to the CEJ [NCCL type V] can only be restored properly with a resin composite filling. Crownradicular NCCLs associated with gingival recession [NCCL types III and IV] are the most complicated and challenging [7]. In fact, in a deep crown radicular NCCL areas, a coronally advanced flap alone could not predict root coverage to the level of the MRC since the presence of the root concavity left after the restoration. These concavities may lead to the flap shrinkage and collapse. Therefore, this type of lesion requires the addition of a CTG underneath the advanced flap. Moreover, one other reason for applying CTG is to augment gingival thickness, therefore ensuring the long-term stability of the coverage procedure [13].
Conclusion
Gingival recessions associated with NCCLs can be successfully treated. Before any restorative/surgical procedure, it is necessary to remove or control all the possible etiological factors associated with GR and NCCLs. The predetermination of the MRC can be used for the selection of the treatment approach of a CD. For the restorative procedure, resin composites may be recommended because of their esthetic properties. In cases where a surgical approach is indicated, CAF and bilaminar procedures combined or not with a CTG are considered the most predictable treatment options for single and multiple recession defects. This report of three cases supports the effectiveness of the combined approach in managing, non-carious cervical lesions associated with gingival recession with regards to tissues biology, surpassing the limitations of each treatment conducted alone and ensuring a long-term stability result.
Conclusion
- The American Academy of Periodontology. Glossary of periodontal terms. 4th edition 2001: 44.
- Susin C, Haas AN, Oppermann RV, Haugejorden O, Albandar JM (2004) Gingival recession: epidemiology and risk indicators in a representative urban Brazilian population. J Periodontol 75(10): 1377-1386.
- Imber J-C, Kasaj A (2021) Treatment of Gingival Recession: When and How? Int Dent J 71(3): 178-187.
- Cortellini P, Bissada NF (2018) Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J Periodontol 89(Suppl1): S204-213.
- Pini-Prato G, Franceschi D, Cairo F, Nieri M, Rotundo R (2010) Classification of dental surface defects in areas of gingival recession. J Periodontol 81(6): 885-890.
- Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U (2011) The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: an explorative and reliability study. J Clin Periodontol 38(7): 661-666.
- Zucchelli G, Gori G, Mele M, Stefanini M, Mazzotti C, et al. (2011) Non-carious cervical lesions associated with gingival recessions: a decision-making process. J Periodontol 82(12): 1713-1724.
- Santamaria MP, Suaid FF, Nociti FH, Casati MZ, Sallum AW, et al. (2007) Periodontal surgery and glass ionomer restoration in the treatment of gingival recession associated with a non-carious cervical lesion: report of three cases. J Periodontol 78(6): 1146-1153.
- Santamaria MP, Suaid FF, Casati MZ, Nociti FH, Sallum AW, et al. (2008) Coronally positioned flap plus resin-modified glass ionomer restoration for the treatment of gingival recession associated with non-carious cervical lesions: a randomized controlled clinical trial. J Periodontol 79(4): 621-628.
- Santamaria MP, da Silva Feitosa D, Nociti FH, Casati MZ, Sallum AW, et al. (2009) Cervical restoration and the amount of soft tissue coverage achieved by coronally advanced flap: a 2-year follow-up randomized-controlled clinical trial. J Clin Periodontol 36(5): 434-441.
- Gennai S, Guiza ZB, Orsolini C, Gosset M (2022) The influence of non-carious lesions in the surgical treatment of gingival recession: A systematic review & meta-analysis. J Dent 117: 103922.
- Santamaria MP, Suaid FF, Carvalho MD, Nociti FH, Casati MZ, et al. (2013) Healing patterns after subgingival placement of a resin-modified glass-ionomer restoration: a histometric study in dogs. Int J Periodontics Restorative Dent 33(5): 679-687.
- Zucchelli G (2013) Mucogingival Esthetic Surgery. 1st é Milan ; Chicago: Quintessenza Edizioni SRL Italy pp. 830.
- Zucchelli G, Mele M, Stefanini M, Mazzotti C, Mounssif I, et al. (2010) Predetermination of root coverage. J Periodontol 81(7): 1019-1026.