Evaluation of Frequency, Degree of Lower Wisdom Tooth Occlusion and Complications after Surgery in 90 Patients
Hamed Nabahat1*, Nadasadat Hashemi1, Alireza Rajabi2, Naval Zaeri2, Melika Tahan1, Mahmoud Malek Mohammadi2, Sogol Poursamad2, Amirhosein Babalou1 and Sahar Haghighat2
1A.I. Yevdokimov Moscow State University of Medicine and Dentistry, Moscow, Russia
2I.M. Sechenov First Moscow State Medical University (MSMU), Moscow, Russia
Submission: November 14, 2022; Published: November 28, 2022
*Corresponding author: NedaSadat Hashemi, A.I. Yevdokimov Moscow State University of Medicine and Dentistry, Moscow, Russia
How to cite this article: Hamed Nabahat*, Nadasadat Hashemi, Alireza Rajabi, Naval Zaeri, Melika Tahan, Mahmoud Malek Mohammadi, Sogol Poursamad, Amirhosein Babalou and Sahar Haghighat. Evaluation of Frequency, Degree of Lower Wisdom Tooth Occlusion and Complications after Surgery in 90 Patients. Adv Dent & Oral Health. 2022; 15(5): 555922. DOI: 10.19080/ADOH.2022.15.555922
Abstract
The presence of opioid receptors around peripheral nerves allows for postoperative analgesia, thus encouraging the study of the effect of opioids in combination with local anesthesia (LA). Studies have also reported the effectiveness of topical opioids in achieving adequate analgesia in inflamed areas. Using the concept of peripheral opioid receptors, our study aimed to evaluate the effectiveness of opioid analgesia in postoperative pain management. Also, the presence of impacted teeth is a common phenomenon and in different societies, its prevalence and distribution vary significantly. The possibility of problems occurring in case of failure to diagnose and treat the impacted lower wisdom teeth on time indicates the importance of this issue. According to the results of this research, the prevalence of impacted teeth with medium hardness and difficulty in patients referring to the Faculty of Dentistry of Mod Amulet Clinic in Russia is relatively high. Buprenorphine added to lidocaine 2% showed a minimal decrease in the pain score and duration of postoperative analgesia with no difference in the frequency of rescue analgesics consumed between the test and control.
Keywords: Impacted teeth; Lower wisdom teeth; Impact teeth; Prevalence lesions
Abbreviations: LA: Local anesthesia; NSAIDs: Nonsteroidal anti-inflammatory medicines; TMJ: Temporomandibular joint
Introduction
The patient is more likely to have pain and discomfort because of the surgically removed impacted mandibular third molars in the oral cavity. Even though the lower jaw’s third molars are frequently extracted surgically, patients’ greatest concern is pain control [1]. The main issue arises postoperatively when the anesthetic’s effects wear off, even when intraoperative pain is effectively managed with local anesthesia (LA). The management of pain is a crucial component since postoperative pain and discomfort can make the patient’s overall treatment experience unpleasant. Most of the time, local anesthetics such as lidocaine 2% with epinephrine 1:2,000 are used during tooth extraction [2,3]. The local agent’s effects last for roughly 40 to 60 minutes, which is how long the surgery takes. The patient experiences discomfort as soon as the local anesthetic agent’s effects wear off [4]. The patient takes analgesics after surgery to get over this. Nonsteroidal anti-inflammatory medicines (NSAIDs) including ibuprofen, aspirin, and diclofenac, as well as opioids with central action like morphine, are the most often prescribed analgesics. These medications efficiently control postoperative pain, but they each have different side effects [5]. Systemic side effects of NSAIDs include peptic ulcers, platelet dysfunction, and renal, and hepatic dysfunction. Opioids that are -agonists, however, provide an efficient substitute for opioids without causing immediate organ damage. Opioids, however, can also have central side effects such as nausea, vomiting, dizziness, exhaustion, respiratory depression, and hypotension.
This helped researchers understand buprenorphine hydrochloride, a medication with powerful analgesic efficacy and almost no negative systemic side effects. A synthetic opioid with agonistic, antagonistic, and antihyperalgesic properties is buprenorphine hydrochloride. Buprenorphine’s pharmacological effects are reportedly 20–25 times stronger than those of morphine (a -opioid receptor agonist), with a quicker onset and longer duration of action (buprenorphine 0.3 mg is as potent as morphine 10 mg) [6,7]. Various factors such as the growth stage of the tooth and the radiographic pattern of the development and growth of the teeth affect this frequency. Embedded teeth can cause caries, pulp, and periodontal diseases, root resorption of adjacent teeth, and even tumors of the mouth, jaw, and face, which are very difficult to diagnose and treat for dentists, and how to treat in terms of function and beauty is also difficult for patients with It is important [5]. The reasons for prescribing wisdom tooth extraction are pain caused by caries, temporomandibular joint (TMJ) pain, orthodontics and crowding, pericoronitis, and prosthetic preparations. And its distribution has considerable diversity.
Materials and Methods
A number of 90 patients (out of 850 patients) who were referred to the oral and maxillofacial surgery department of the Moscow Clinic in 2021-2022 for the surgery of mandible wisdom teeth were included in the plan [8]. Before surgery, the degree of hardness of the impacted tooth was evaluated and determined according to the combination of Winter, Schiller, and Pell & Gregory classifications based on the OPG radiographic view and recorded in the checklist [9,10]. Then wisdom tooth surgery was performed. The Pell & Gregory criterion is expressed as follows:
a) Pell & Gregory’s vertical classification is described in three classes A, B, and C in terms of depth of wisdom tooth (M3) embedment compared to the dentofacial plan of the second molar tooth (M2). In class A, the depth of M3 embedment is at the level of the dentofacial plan of the M2 tooth, class B, the depth of M3 embedment is between the dentofacial surface and the CEJ of the M2 tooth, and in class C, the depth of the M3 embedment is below the CEJ of the M2 tooth.
b) Horizontal Pell & Gregory classification, in terms of the space between the mandible ramus and M3, is divided into three classes 1, 2, and 3.
i. Class 1: There is enough space for M3 growth,
ii. Class 2: There is not enough space for M3 growth (M3 tooth is partially inside the ramus), and
iii. Class 3: M3 tooth is completely inside the ramus.
Schiller’s classification (which is a supplement to Winter’s classification) determines the mesial-distal relationship and the occlusion angle. In this classification, the hardness is grouped as singular, horizontal, vertical, and distangular from one to four, so that in the mesioangular type (hardness 1) the longitudinal axis of the M3 tooth crown with the occlusal surface. The M2 tooth has an angle between 10 and 70 degrees towards the mesial side if it has the same angle towards the distal side [11]. Distangular (difficulty 4) is classified. The angle is less than ten degrees mesial or distal as vertical (difficulty 2), and an angle greater than 70 degrees mesial or distal is considered horizontal depression (severity 3). Finally, by using the above three classifications, technical and technical issues and problems of surgery were predicted and investigated. According to the degree of difficulty obtained from the vertical Pell & Gregory classification from 1 to 3, as well as the horizontal Pell & Gregory from 1 to 3, as well as the Schiller classification from 1 to 4, in total, the total degree of difficulty based on the Pederson classification scale, Defined from 3 to 10.
In general, the degree of hardness of wisdom teeth is classified as follows:
Easy 3-4, medium: 5-7, and hard 8-10. Finally, the information obtained from 90 patients (out of 850 patients) was summarized and compared based on the gender and severity of the obstruction, and the prevalence percentage of different obstructions was obtained.
The relationship between the variables was checked by SPSS software with version 22 [12]. It should be noted that chi-square tests and one-factor analysis of variance were used in the data analysis.
Technique for Making the Solution
A modified solution of lidocaine 2% with epinephrine 1:20,000 mixed with buprenorphine and solution B containing lidocaine 2% with epinephrine 1:2,000 were created as two solutions for a double-blinded trial. Buprenorphine was added to lidocaine 2% at a dosage of 1 ml of 0.3 mg in a 30 ml vial (0.01 mg/ml) [13]. After receiving the coin from the appropriate patient, the dental nurse started working on the solution. The most LA that may be given was 3 ml. In 3 ml of LA given, there was 0.03 mg of buprenorphine (0.01 mg/ml x 3 ml).
Database Analysis
SPSS version 20 (IBM Corp., 2011) was used for the analysis. Armonk, New York: IBM Corp., IBM SPSS Statistics for Windows, Version 20.0. Statistical significance was defined as a p-value of 0.05. The Wilcoxon signed-rank test was used to compare the pain scores and the number of rescue analgesics between the test and control groups [14,15].
Result and Discussion
The surgical method is invasive since it entails making a mucosal incision to raise a mucoperiosteal flap that exposes the impacted tooth underneath. Bradykinin and histamine are two inflammatory mediators that are released in response to tissue injury. The nociceptors are affected by these inflammatory mediators [14,16]. Soreness, swelling in the submandibular region, and trismus in the submasseteric region are probably the results. Analgesics and anti-inflammatory medications, the most popular of which are NSAIDs, are prescribed postoperatively (nonsteroidal anti-inflammatory drugs) [17]. Despite having an analgesic effect, they have the potential to have negative side effects, including renal damage and GI problems. Opioid analgesics, on the other hand, are a mainstay of management for crippling disorders. In low doses, they are not known to directly affect organs [18]. On the other hand, they are known to have central effects such as nausea, vomiting, increased biliary tract pressure, dizziness, exhaustion, respiratory depression, and hypotension when taken systemically. Studies on the impact of opioids when combined with LA were encouraged by the discovery of opioid receptors on peripheral nerves, which revealed the potential for obtaining postoperative analgesia. However, studies were done to examine the effectiveness of a stronger opioid that is a partial agonist of the -opioid receptor and antagonist of the -opioid receptor and shows less systemic adverse effects due to the varied central effects associated with the usage of morphine. When compared to morphine, buprenorphine, a mild-receptor agonist and antagonist, induced analgesia that lasted longer while having fewer side effects (Table1).
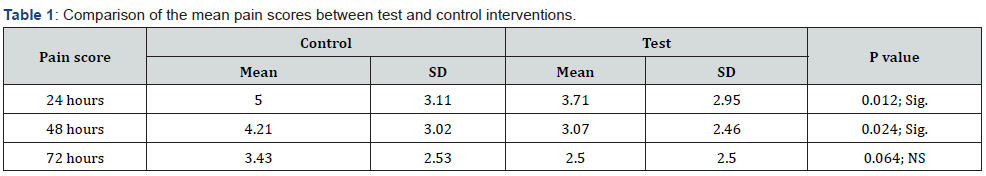
Sig: Significant; NS: Nonsignificant.
Conclusion
Women were more likely than men to have impacted wisdom teeth among the patients who visited the Mod Amulet dental clinic in Moscow. Mesioangular angles of incidence were most frequently seen. Medium hardness degree was associated with the highest likelihood of wisdom teeth impaction. According to the classifications by Winter & Schiller and Pell & Gregory, there is a considerable correlation between gender and the angle at which wisdom teeth are impacted as well as their depth and connection to the ramus. When used for intraoral block procedures, a local anesthetic solution combined with buprenorphine efficiently lowers postoperative pain with few adverse effects. In the first 48 hours after receiving lidocaine and buprenorphine, participants in the current study had significantly lower mean pain scores. However, there was no discernible distinction between the test and control interventions in terms of how many rescue analgesics were used.
Acknowledgment
This study was conducted as a case study in Russia (2021- 2022) and was presented at the International Conference on Dentistry and Oral Health May 05-06, 2022 in Rome, Italy.
References
- Akomolafe AG, Fatusi OA, Ukpong MO, Mosaku KS, Adejobi AF, et al. (2022) Relationship Between Types of Information, Dental Anxiety and Post-Operative Pain Following Third Molar Surgery, A Randomised Study. Journal of Oral and Maxillofacial Surgery.
- Eshghpour M, Nezadi A, Moradi A, Shamsabadi RM, Rezaer N, et al. (2014) Pattern of mandibular third molar impaction: A cross‑sectional study in northeast of Iran. Niger J Clin Pract 17(6): 673-677.
- Ciftci V, Guney A, Deveci C, Sanri I, Salimow F, et al. (2021) Spontaneous space closure following the extraction of the first permanent mandibular molar. Niger J Clin Pract 24(10): 1450-1456.
- Choudhury R, Rastogi S, Rohatgi RG, Abdulrahman BI, Dutta S, et al. (2022) Does pedicle flap design influence the postoperative sequel of lower third molar surgery and quality of life? J Oral Biol Craniofac Res 12(5): 694-701.
- Pérez-González F, Abusamak M, Sáez-Alcaide LM, García-Denche JT, et al. (2022) Effect of time-dependent ibuprofen administration on the post operatory after impacted third molar extraction: a cross-over randomized controlled trial. Oral Maxillofac Surg p: 1-8.
- Amaral JS, Marto CM, Farias J, Pereira DA, Ermida J, et al. (2022) A Pilot Randomized Controlled Clinical Trial Comparing Piezo Versus Conventional Rotary Surgery for Removal of Impacted Mandibular Third Molars. Bioengineering 9(7): 276.
- Hamed N, Melika T, Faezeh A, Leonid SK, Kapralova VV (2021) Regeneration of Permanent Tooth Enamel (Alternative Solution of Nano-hydroxyapatite) after Exposure to Beer (Laboratory Study at the Dental Center, Moscow, Russia). Adv Dent & Oral Health 14(4): 555891.
- Shoshani-Dror D, Shilo D, Ginini JG, Emodi O, Rachmiel A (2018) Controversy regarding the need for prophylactic removal of impacted third molars: An overview. Quintessence International 49(8): 653-662.
- Terlemez A, Tassoker M, Kizilcakaya M, Gulec M (2019) Comparison of cone-beam computed tomography and panoramic radiography in the evaluation of maxillary sinus pathology related to maxillary posterior teeth: Do apical lesions increase the risk of maxillary sinus pathology? Imaging Sci Dent 49(2): 115-122.
- Faridnejad H (2022) Biostat Biom Open Access J Design and Simulation of the Source (Wiggler) and Medical Beamline of Iranian Light Source Facility (ILSF) for Medical Applications. JP Journal of Biostatistics 10(4): 555793.
- Abdilahi AM, Ashar A, Hassan J, Naqash A. Comparative Study of two Flap Designs on Postoperative Sequelae after Removal of Impacted Mandibular Third Molar.
- Farhadi F, Emamverdizadeh P, Hadilou M, Jalali P (2022) Evaluation of Infection and Effective Factors in Impacted Mandibular Third Molar Surgeries: A Cross-Sectional Study. Int J Dent 2022: 8934184.
- Domínguez M, Pina T (2020) Aging Through Cartoons: The Unbearable Lightness. Understanding the Discourse of Aging: A Multifaceted Perspective pp: 307.
- Isah MB, Oche OM, Yunusa EU, Yunusa MA, Oladigbolu RA, et al. Perception, prevalence and correlates of depression among females attending the Gynaecological Clinic of Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria.
- Kang F, Sah M, Fei G (2020) Determining the risk relationship associated with inferior alveolar nerve injury following removal of mandibular third molar teeth: A systematic review. J Stomatol Oral Maxillofac Surg 121(1): 63-69.
- Masinde D, Cheruiyot J. Dental Caries Experience and Associated Risk Factors Among Pre-School Going Children in Bureti Sub-County, Kericho County, Kenya.
- Estrela CR, Bueno MR, Estrela MR, Estrela LR, Guedes OA, et al. (2022) Frequency and risk factors of maxillary sinusitis of endodontic origin evaluated by a dynamic navigation and a new filter of cone-beam computed tomography. J Endod 48(10): 1263-1272.
- Verhulst MJ, Loos BG, Gerdes VE, Teeuw WJ (2019) Evaluating all potential oral complications of diabetes mellitus. Frontiers in endocrinology 10: 56.






























