Comparative Study of Two Different Tooth Restorative and Finishing/Polishing Techniques, and the Post-Restorative Impact
Brooke Wilder-Corrigan1, Jacob Tuft1, Roberto Lara1, Pam Van Ry2, Ashley Chang2, Josue D Gonzalez Murcia3, Claudia M Tellez Freitas1, Katherine Velasco1 and David S Howard1
1College of Dental Medicine, Roseman University of Health Sciences, Jordan, Utah
2Department of Chemistry & Biochemistry, Brigham Young University ,Utah
3Department of Microbiology and Molecular Biology, Brigham Young University, Utah
Submission: May 11, 2022; Published: May 30, 2022
*Corresponding author: David S Howard, College of Dental Medicine, Roseman University of Health Sciences, Jordan, Utah
How to cite this article: Brooke W-C, Jacob T, Roberto L, Pam Van R, Ashley C, et al. Comparative Study of Two Different Tooth Restorative and Finishing/Polishing Techniques, and the Post-Restorative Impact. Adv Dent & Oral Health. 2022; 15(3): 555914. DOI: 10.19080/ADOH.2022.15.555914
Abstract
This study aimed to improve patient oral health by identifying and illustrating the impact that rotary instruments have on composite restorations during the preparation and finishing/polishing procedures involved in traditional and modern restorative techniques. Marginal defects or deficiencies are a common cause of recurrent caries and restoration failure. Microfractures are a suspected beginning of eventual restoration failures. Therefore, demonstration of iatrogenic damage caused by instrumentation and preparation configuration was assessed with the goal of improving composite resin failure rates and increasing the longevity of dental restorations. Results obtained in this study illustrated that traditionally prepared teeth exhibited more total fractures (p < 0.05) than modern restorative preparations. Traditionally prepared teeth undergoing either finishing/polishing technique did not yield significant differences, while Modern prepared teeth illustrated a statistically significant difference of fractures inflicted from the control group to the final polish for carbide + Jiffy polish (p=0.0034) and diamond + Rockstar polish (p=0.0003). Additional study will be required to determine if a specific location is prone to rotary-insult in Modern finishing and polishing (i.e., infinity margins), or if the results were due to some other cause such as over instrumenting or overheating the teeth. Future research will compare the post-restorative biofilm growth and infiltration of the fractured or marginal deficient areas, and the subsequent impact of rotary instruments on Traditional and Modern restorative techniques and seek to improve the longevity of dental restorations.
Keywords: Restoration, Modern technique, Traditional technique, Finishing, Polishing, Carbide bur, Diamond bur, Microfracture, Jiffy polish, Rockstar polish, Resin failure
Abbreviations: TRI: Tooth restoration interface; TCJP: Traditional Carbide + Jiffy Polish; TDRP: Traditional Diamond + Rockstar Polish; MCRT: Modern Composite Restorative Technique
Introduction
Dental caries is a common multifactorial disease around the world and is regarded as the leading cause of oral pain and tooth loss [1]. Treatment of the disease includes restorative intervention using methods such as amalgam restorations, resin restorations, porcelain restorations, gold restorations, endodontic therapy, and extraction. The use of composite resin has grown in popularity due to esthetic properties. However, the longevity of composite resin restorations is determined to be only 2-6 years [2]. Factors influencing this longevity have long since been proven to correlate with the amount of tooth structure removed, faulty cavity preparations, improper manipulation of restorative materials and geometric form of the cavity preparation [3-5]. However, other factors may also include iatrogenic damage introduced by use of unfavorable restorative and finishing/polishing techniques by the dental provider. Studies analyzing the impact of preparation design and finishing/polishing techniques on resin failure rate and post-restorative biofilm colonization are minimal. Both factors may significantly influence the longevity and success of direct composite resin restorations. Analyzing the post- restorative impact of traditional and modern restorative techniques may be imperative for developing more favorable and long-lasting resins.
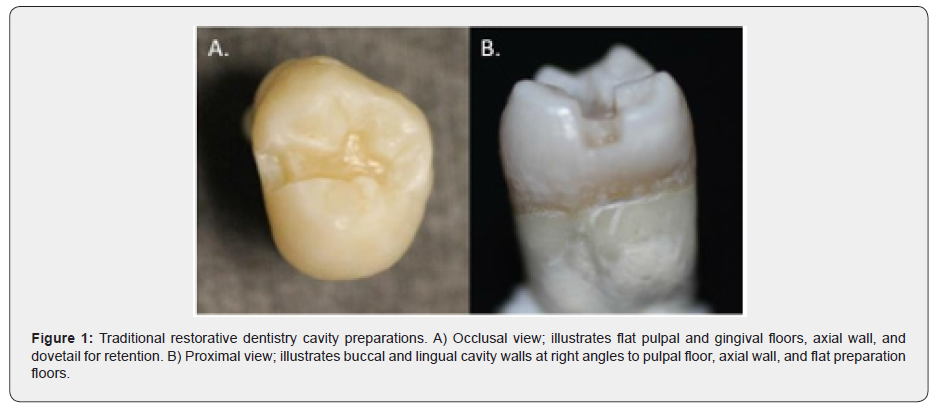
Phase 1 of this study was conducted to directly analyze traditional and modern restorative dentistry and the impact that the finishing/polishing process has on both techniques. The G.V. Black cavity preparation used in traditional restorative dentistry was designed and works very well for amalgam [6]. However, the traditional G.V. Black preparation based on its design criteria creates high C-factor and areas of stress focalization, both of which are unfavorable for success when using composite resins to restore teeth. The design of the Traditional cavity preparation requires resistance and retention to be obtained through removal of healthy tooth structure [7]. Buccal and lingual cavity walls must be created at right angles to the pulpal floor to provide retention and must be parallel to the long axis of the tooth. Additional retentive features, like dovetails or retention grooves, may also be necessary to preserve the longevity of the restoration (Figure 1). Inappropriate stress concentration at the axio-pulpal line angle or along an unbeveled cavo-surface margin, high C-factor, and high tensile strengths all contribute to fracture and failure of the restoration [5]. When these characteristics were observed in composite resin restorations shortly after their initial employment an incremental filling technique was developed in an attempt to mitigate the concerns. Incremental filling techniques utilized in traditional restorative dentistry possess the potential for spaces or voids to be introduced between layered resin. The voids between polymerized layers may serve as reservoirs for colonization by anaerobic bacteria (Figure 2).

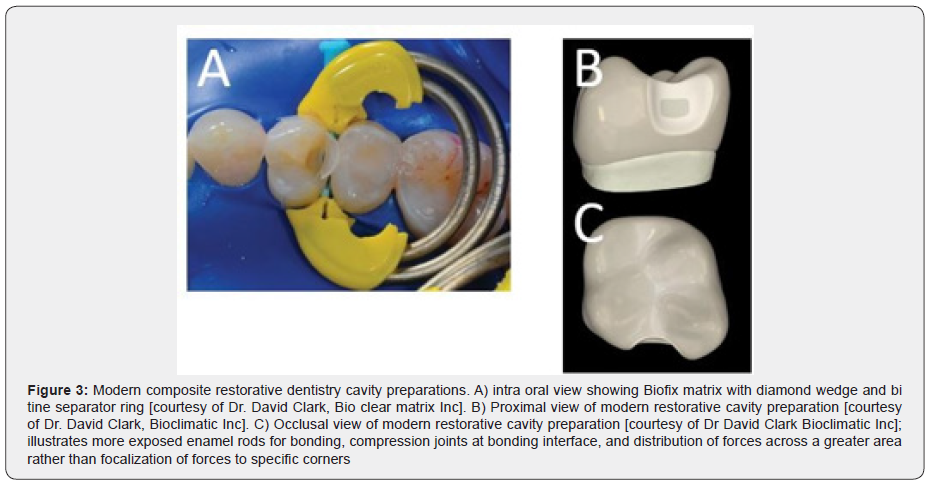
Improper finishing and polishing techniques may exacerbate this colonization process by the introduction of voids or defects in the tooth restoration interface (TRI) of composite resins via microfractures. Modern composite restorative techniques utilize a more conservative and minimally invasive approach. Cavity preparation is created in a “saucer” shape rather than a box shape (see Appendix, Figure 3). Use of a saucer-shaped preparation minimizes C-factor and decreases the negative impact of C-factor on the micro-tensile bond strength of resin to dentin [8,7]. Furthermore, a beveled calla lily or saucer-shaped configuration allows for the creation of compression joints at the TRI vs tensile joints at the margins of perpendicular walls, and distribution of stress across a greater area instead of focalizing stress to corners. Cavo-surface margins are beveled to create an infinity edge margin, which allows composite resins to bond more intimately with exposed enamel rods for retention purposes and allows for finishing the restoration to an undetectable TRI (hence the name “infinity edge”).
The monolithic injection molding technique used in modern dentistry provides a solid bulk of material for strength and has little to no potential to introduce voids or spaces between resin layers. Lack of a potential reservoir space in bulk-fill techniques may suggest bacterial colonies cannot penetrate into the defects of composite resin restorations and migrate deeper into the tooth. Use of improper finishing and polishing techniques in modern dentistry is still of concern however, due to the potential for iatrogenic damage to be introduced on the surface of composite resin restorations.
Phase 2 of this study will directly analyze the post-restorative migratory capacity of Pseudomonas bacterial strains on the surface of restorations completed by traditional and modern restorative standards. In this phase, the teeth will be incubated with a Pseudomonas biofilm exposed to the surface of traditional and modern post-restorative teeth to evaluate bacterial adherence and/or penetration into defect areas, which would be indicative of a damaged area allowing biofilm adhesion. Pseudomonas exposure will simulate biofilm present within human subjects under normal oral conditions.
The unfavorable use of rotary instruments (i.e., Carbide vs. diamond burs) may introduce microfractures in composite resin restorations or teeth that can serve as reservoirs for colonization of aerobic bacteria, such as Pseudomonas or streptococcus. The brittle nature of polymerized composite resins may succumb to iatrogenic damage if the operator uses instruments that are not conducive to finishing and polishing brittle materials. Increased colonization due to insufficient techniques may lead to restoration failure over time. We theorize that traditional restorative dentistry using the G.V. Black preparation and incremental-fill technique leads to easily compromised tensile joints and voids or defects between layers that can be fractured during finishing and polishing. These compromised areas then serve as access points and reservoirs for the colonization of bacteria after use of carbide rotary instruments during finishing and polishing. It has been observed by some that all composite restorations leak at the preparation margins [9-11]. Modern composite restorative dentistry on the other hand, uses preheated monolithic injection molding techniques that result in compression joints and few, if any, voids or defects between polymerized layers. Additionally, researchers have observed that preheating composite results in significantly decreased microleakage [12]. If proven true, this means that bacteria have no migratory capacity to deeper surfaces. Failure to penetrate resins to a deeper level may result in decreased recurrent caries, bacterial infections into the dentinal tubules, and pulpal irritation. We aim to discover if microfractures caused by unfavorable materials and techniques can be a beginning platform for biofilm colonization. This study aims to improve patient oral health by illustrating the impact that rotary instruments have on composite during the preparation and finishing/polishing procedures involved in traditional and modern restorative techniques. Demonstration of unfavorable instrumentation may improve composite resin failure rates and increase the longevity of dental restorations.
Objectives
The main objectives of this comparative study include:
i. Improve patient oral health by illustrating the impact of improper use of instrumentation, and or unfavorable materials and methods used during preparation and finishing/polishing procedures in traditional and modern restorative techniques.
ii. Improve direct composite resin failure rates by demonstrating the influence of improper instrumentation on post-restorative biofilm colonization in traditional and modern restorative techniques.
iii. Discover if a particular restorative technique is more beneficial to prevent recurrent colonization and promotes restoration longevity and success.
Materials and Methods
Materials
Materials used for this study were as follows:
a) Traditional preparations: Tofflemire matrix, Ultra etch, Scotchbond universal single dose, shade A2 Filtek supreme.
b) Modern preparations: Bioclear matrix, Ultra etch, Scotchbond universal single dose, shade A2 Filtek bulk fill flowable, shade A2 Filtek 1 bulk fill.
Tooth Selection and Preparation

Extracted virgin human 3rd molars were obtained from a tooth bank supplied by Roseman College of Dental Medicine. The sample teeth were initially evaluated for any visible fractures and microfractures with 2.5x magnification Orascoptic Loupes using Bioclear Disclosing Solution and LED light. Samples with visibly detectable fracture lines were not included in this study (Figure 4). Eighty (80) teeth in total were selected based on these criteria, with twenty in each study group. All samples were mounted in a PVS base to ensure repeatable orientation of samples. All samples were then evaluated prior to preparation by Micro-CT to account for and map any pre- existing internal micro fractures.
Study Design
The four groups created for this study were as follows: 1) Traditional GV Black preparation with incremental fill technique followed by carbide finishing burs and Jiffy polishing system; 2) Traditional GV Black preparation with incremental fill technique followed by diamond finishing burs, brownie bur, and Rockstar polisher; 3) Modern calla lily or saucer-shaped preparation with heated bulk fill injection molding technique followed by carbide finishing burs and Jiffy polishing system; 4) Modern calla lily or saucer-shaped preparation with heated bulk fill injection molding technique followed by diamond finishing burs, brownie bur, and Rockstar polisher. Burs were traded out to a new bur after every three tooth preparations completed [13]. Burs used during Modern preparations included 330, #4 round latch, and beveling burs. Burs used during Traditional preparations included 330 and #4 round latch burs. All samples were evaluated post- preparation by Micro-CT to account for fractures inflicted during the preparatory phase.
Restoration and Finishing Techniques
Teeth were restored using materials designated for each preparation design. All materials were used according to manufacturer guidelines. The curing technique used for traditional preparations was from an occlusal direction only with a 30-second cure. The curing technique used for modern preparations was a 5-second tac cure from buccal, lingual and occlusal, followed by a full 30-second cure from all three of the previously mentioned directions.
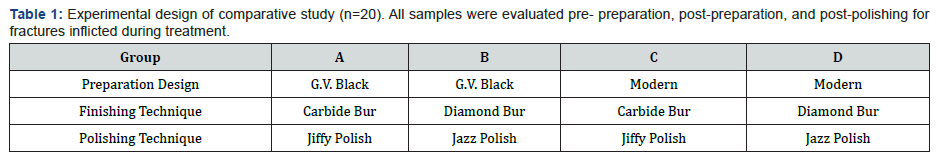
Micro-CT Scan
Teeth were mounted on a repeatable oriented base using PVS and analyzed by X-Ray Microtomography scanning (Micro-CT) to record baseline fracture levels. Teeth were then randomly grouped (n=20) and prepared based on experimental design (Table 1). All samples were evaluated post-preparation by Micro-CT for additional fractures inflicted during the preparatory phase. Teeth were then restored, polished, and evaluated a third time for additional fractures inflicted. All data was compared to control values and statistically analyzed for significant fracture differences.
Statistical Analysis
GraphPad Prism program was used for statistical analysis. Statistical significance was assessed using impaired T-Test and One way-ANOVA test to compare among different group treatments.
Results
MCRT Vs. Traditional Treatments
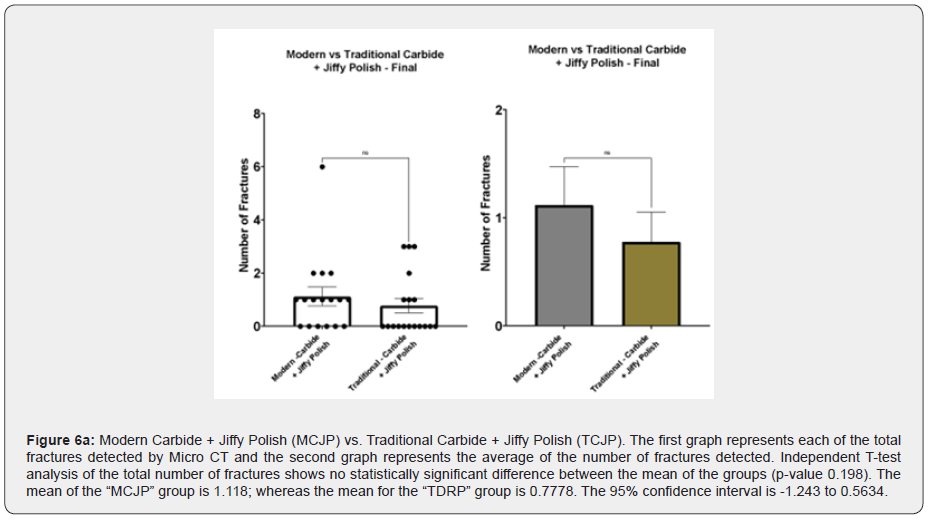
A significant difference was found between traditional preparations and MCRT preparations; traditionally prepared teeth exhibited more total fractures (p < 0.05) than Modern saucer-shaped preparations (Figure 5). Comparison of polishing between MCRT and Traditional techniques, however, did not yield significant differences in number of provider-induced microfractures (Figure 6a & 6b).

Traditional Treatments
Traditionally prepared teeth undergoing either experimental finishing/polishing technique did not yield significant differences between polishing techniques (Figure 7). In other words, finishing and polishing restorations on traditional GV Black prepared teeth did not introduce new microfractures.
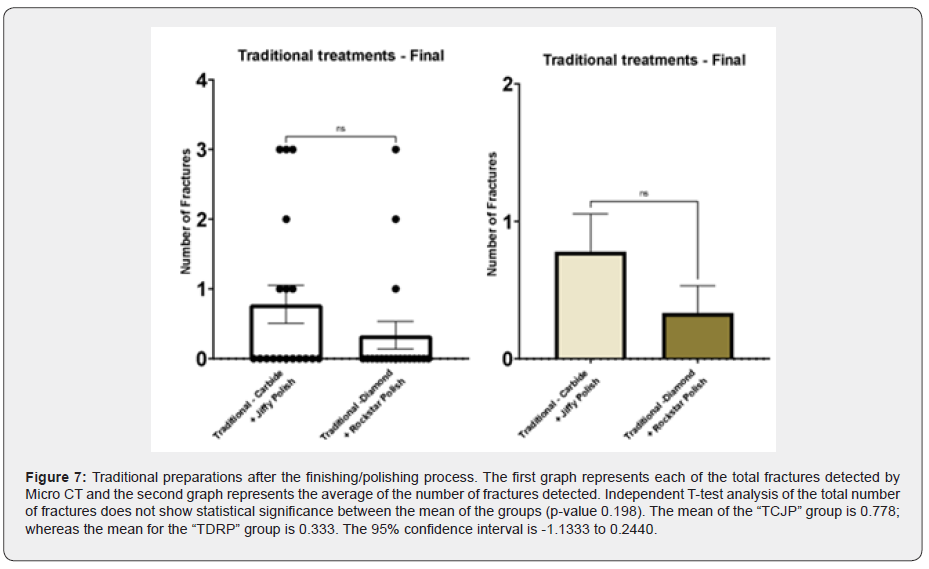
Traditional Treatments
Traditionally prepared teeth undergoing either experimental finishing/polishing technique did not yield significant differences between polishing techniques (Figure 7). In other words, finishing and polishing restorations on traditional GV Black prepared teeth did not introduce new microfractures.
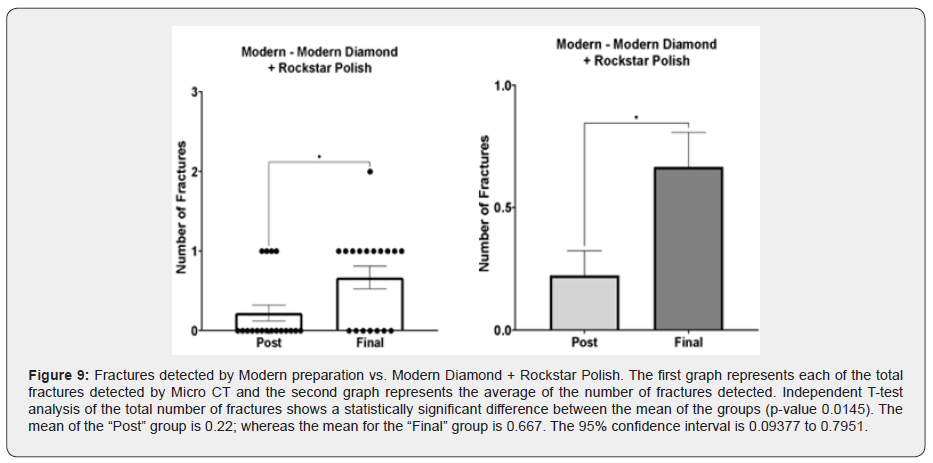
Additional study and further investigation are necessary to determine the reasoning for this observed effect of finishing and polishing Modern preparations. One way-ANOVA comparison between Control, post-preparation and final finishing and polishing for Modern prepped teeth and Carbide + Jiffy Polish revealed that there were not significant differences in the number of cracks inflicted between the control (“Initial”) and post-preparation (“Post”) MicroCT scans, but there were significant differences from the control to post-finishing and polishing (“Final”) (Table 2). One way-ANOVA comparison between Control, post-preparation and final finishing and polishing for Modern prepped teeth and Diamond + Rockstar Polish also revealed that there were not significant differences in the number of fractures inflicted between the control (“Initial”) to post-preparation (“Post”), but that there were significant differences from the control to the final polish (“Final”) (Table 3). Additional investigation is planned to determine the reasoning for these observed effects.
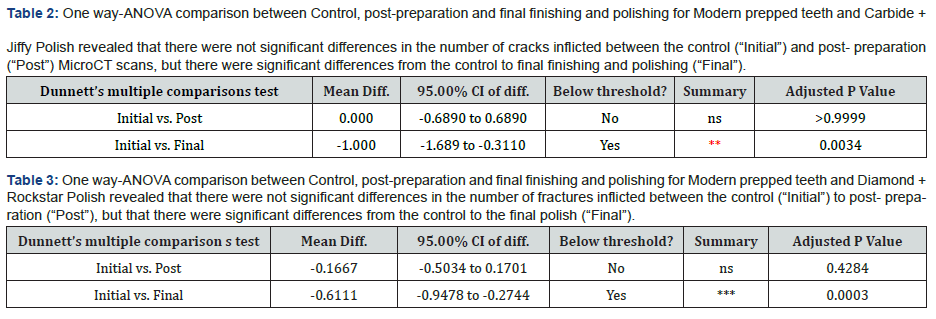
Table 2 One way-ANOVA comparison between Control, post-preparation and final finishing and polishing for Modern prepped teeth and Carbide + Jiffy Polish revealed that there were not significant differences in the number of cracks inflicted between the control (“Initial”) and post- preparation (“Post”) MicroCT scans, but there were significant differences from the control to final finishing and polishing (“Final”).

Discussion
This study was performed to illustrate the impact that rotary instruments have on teeth and composite restorations during the preparation and finishing/polishing procedures involved in traditional and modern restorative techniques. Our data illustrates that Traditional restorative preparation techniques have a tendency to inflict more fractures on a human tooth than Modern preparation techniques [5,14]. While these data suggest that Modern composite tooth preparations appear to be superior to traditional preparations in terms of reducing iatrogenic damage produced by rotary instruments, the finishing and polishing of Modern composite restorations appears to yield a higher propensity for microfracture (traditionally polished teeth produce <1 fracture per tooth, while modern polished teeth produce >1 fracture per tooth). Based on these findings, a definitive conclusion regarding which preparation technique and finishing/polishing combination yields the most ideal outcomes cannot be made with certainty without further study. Modern preparations, though superior to Traditional, appear to be prone to microfracture under either polishing modality, or thus, may not be considered more “ideal” in terms of microfracture prevention, for promoting longevity of the restoration. Additional analysis will be necessary to determine whether a specific location is prone to rotary-insult in Modern finishing and polishing (such as infinity margins)or whether the effect is from overheating due to insufficient lubrication and cooling in the process, or some other phenomenon. It has been hypothesized that the observed microfractures resulting from finishing and polishing may be related to the use of beveling techniques, which is unique to Modern preparations and not Traditional preparations. Increased beveling and exposure of enamel rods may lead to thinner composite resins along infinity margins and produce an area of the tooth susceptible to rotary-insult and fracture [15]. Understanding the reason for, and location of microfractures, will be necessary for improving composite resin failure rates and increasing the longevity of dental restorations.
Conclusion
Our data illustrates that Traditional restorative preparation techniques tend to inflict more fractures on a human tooth than Modern preparation techniques. Finishing and polishing a tooth that has been prepared using a Modern technique, however, will introduce more fractures than finishing and polishing a traditionally prepared tooth. Additional research is required to determine how the polishing technique uniquely affects Modern composite restorations and the propensity to introduce microfractures. Understanding restorative methods will lead to improved longevity of dental composite resins.
References
- Kidd EA, Giedrys Leeper E, Simons D (2000) Take two dentists: a tale of root caries. Dental update 27(5): 222-30.
- Drummond JL (2008) Degradation, fatigue, and failure of resin dental composite materials. Journal of dental research 87(8): 710-719.
- Reel DC, Mitchell RJ (1989) Fracture resistance of teeth restored with Class II composite restorations. The Journal of prosthetic dentistry 61(2): 177-80.
- Larson TD, Douglas WH, Geistfeld RE (1981) Effect of prepared cavities on the strength of teeth. Operative dentistry 6(1): 2-5.
- el Mowafy OM (1993) Fracture strength and fracture patterns of maxillary premolars with approximal slot cavities. Operative dentistry 8(4): 160-6.
- Smith GE, Gale W, Schmidseder J (1982) [Principles of cavity preparation for silver amalgam restorations]. Zahnarzt 26(10): 515-25.
- Severns JE (2019) Student's Manual of Cavity Preparation. Creative Media Partners, LLCP p. 42.
- Alomari QD, Barrieshi-Nusair K, Ali M (2011) Effect of C-factor and LED Curing Mode on Microleakage of Class V Resin Composite Restorations. Eur J Dent 5(4): 400-408.
- Gordon J Christensen D (2021) Are there proven preventive restorative materials?
- Christensen GJ (2010) Should Resin-Based Composite Dominate Restorative Dentistry Today? The Journal of the American Dental Association 141(12): 1490-1493.
- Antonson SA, Yazici AR, Okte Z, Villalta P, Antonson DE, et al. (2012) Effect of resealing on microleakage of resin composite restorations in relationship to margin design and composite type. Eur J Dent 6(4): 389-395.
- Wagner WC, Aksu MN, Neme AM, Linger JB, Pink FE, et al (2008) Effect of pre-heating resin composite on restoration microleakage. Operative dentistry 33(1): 72-78.
- Emir F, Ayyildiz S, Sahin C (2018) What is the changing frequency of diamond burs? J Adv Prosthodont 10(2): 93-100.
- Ferracane JL (2017) Models of Caries Formation around Dental Composite Restorations. Journal of dental research 96(4): 364-371.
- Poojary PK, Bhandary S, Srinivasan R, Nasreen F, Pramod J, et al. (2013) Influence of restorative technique, Bevelling and aging on composite bonding to sectioned incisal edges: A comparative in vitro study. J Conserv Dent 16(1): 28-31.






























