Comparison of Radiographic Alveolar Bone Level using Crown and Sleeve-Coping Telescopic Denture Design on the Abutments of Non-molars for Periodontal and Prosthetic Treatments - A long-term study
Guey-Lin Hou1,2*
1Former Professor, Department of Periodontics, and Graduate Institute of Dental Science, Department of Periodontal Prosthesis, Kaohsiung Medical University, Kaohsiung City, Taiwan
2Former Professor, Department of Periodontal & Prosthetic Therapeutic Center, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Taiwan
Submission: January 10, 2022; Published: February 01, 2022
*Corresponding author: Guey-Lin Hou, Former Professor, Graduate Institute of Dental Science, Department of Periodontics, Kaohsiung Medical University, Taiwan Adv
How to cite this article: Guey-Lin Hou. Comparison of Radiographic Alveolar Bone Level using Crown and Sleeve-Coping Telescopic Denture Design on the Abutments of Non-molars for Periodontal and Prosthetic Treatments - A long-term study. Adv Dent & Oral Health. 2022; 15(2): 555907. DOI: 10.19080/ADOH.2022.15.555907
Abstract
The aim of the present study was to evaluate the long-term effectiveness of clinical combination of non-surgical periodontal therapy (NSPT) with CSC telescopic denture for treatment of non-molars affected severe advanced periodontitis (SAP) with secondary occlusal traumatism (SOT). A total 26 individuals ranging in age from 38 to 78 years with moderate to severe advanced periodontitis were collected as the study samples. Baseline data were assessed included gingival index (GI), plaque index (GI), probing pocket depths, clinical attachment levels, digital radiographic alveolar bone levels (DRABLs), before and after periodontal prosthetic therapies, respectively. The results revealed a strong significant gain (p<0.0001; 1.26±2.19 mm) of RABLs on the maxillary anterior teeth, and a significant gain (p<0.05; 0.69±1.77 mm) of RABLs on the maxillary premolars, respectively. The mean (SD) of RABL on the mandibular premolars (0.98±1.33 mm)was greater than those of mandibular anterior teeth(0.90±1.31mm). Both of mandibular anterior teeth and premolars existed a remarkable significance (p<0.001) of statistical analysis before and after periodontal and prosthetic therapies. We can conclude that the combined use of periodontal and prosthetic therapies of CSCTD seem to be a valuable option in the treatment of SAP with SOT.
Keywords:DRABL; CSCTD; NSPT; SAP with SOT; Abutments
Abbreviations:NSPT: Non-surgical periodontal therapy; SAP: Severe advanced periodontitis; SOT: Secondary occlusal traumatism; GI: Gingival index; PALs: Periodontal attachment levels; DSRIA: Digital scanning radiographic image analysis; IRABL: Initial radiographic alveolar bone level; ABH: Alveolar bone height; IR: intentional replantation
Introduction
The former literatures documented that non-surgical periodontal therapy may not only effectively improves clinical parameters, but also resolves and arrests periodontal tissues inflammation [1-3]. In addition, there still exist some problematic areas, such as, root trunk morphology, furcal root concavity, periodontal osseous defects, usually correlated with deep pockets that may adversely respond to non-surgical periodontal therapy because of these sites limited access to debride bacterial soft and hard deposits. The finding of minimal bone fills after scaling and root planning was in contrast to the findings of bone fills, which reported by Rosling et al. [4] and Polson & Heijl [5] that abundant bone repair, post-surgically. Some clinical studies [6-8] indicated that deep pockets within the non-molar and molar areas have prone to higher mortality rate when observed over many years. There still exists conflicting data regarding the bone fills of angular defects following surgical and non-surgical periodontal therapy (NSPT). Renvert et al. [9] indicated that limited repair in treating intraosseous defects using flap operation and there was virtually no bone fill after root planning.
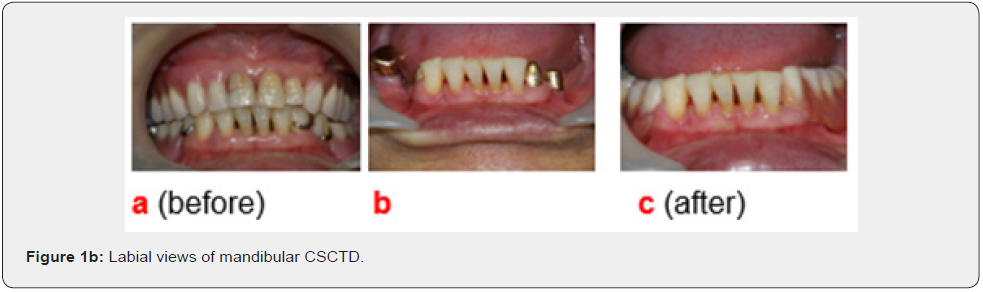
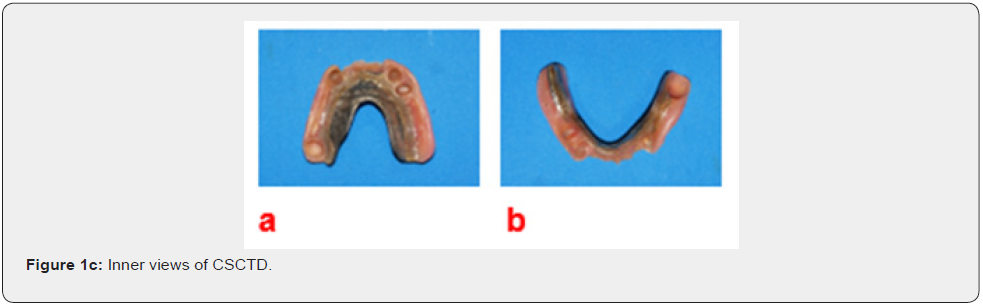
Baderstein et al. [10] found periodontal flap operation resulted in 0.5 mm bone fill in angular defects and no changes following root planning. Lindhe et al. [11] and Isidor & Karring [12] indicated that long-term effective of non-surgical and surgical periodontal treatment showed a tendency toward more gain of mean periodontal attachment levels (PALs). Most of former reports did not present the quantity and volume of alveolar bone levels before and after non-surgical and surgical periodontal therapies via assessment of radiographic alveolar bone levels (RABLs). Little or limited reports [13] related to the RABL differences of periodontal treatment before and after assessments with combination of periodontal and prosthetic designs using digital scanning method. The purpose of present study was retrospectively to investigate one of our long-term follow-up case series. The subject is focus on the differences of RABLs before and after periodontal and prosthetic treatment using NSPT and CSC telescopic denture (CSCTD) design on the abutments of non-molars for the long-term study of abutments with severely advanced periodontitis (SAP). In addition, evidenced-based clinical trials options as TPP, NSPT, and CSCTD were also prescribed here (Figure 1a,b,c).

Materials and Methods
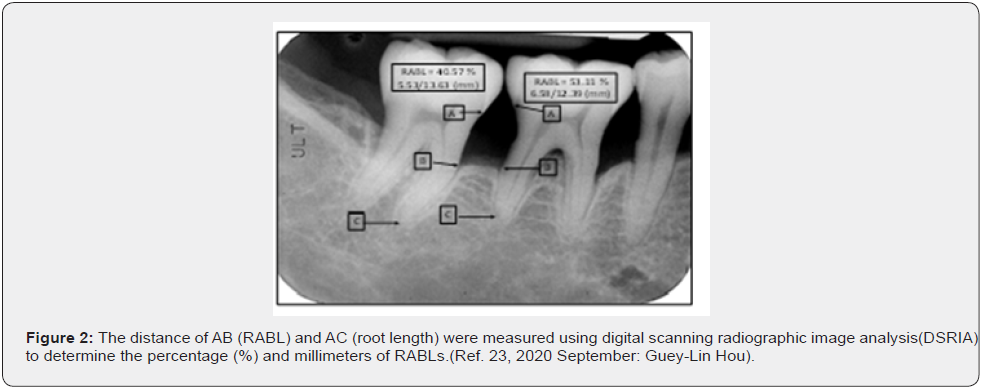
The present samples are extension of our cases series study on the outcome of a periodontal Clinics for the treatment of individuals affected SAP with SOT. The present samples were based on a retrospective analysis of 26 individuals. Proper informed consent was obtained from these 26 individuals, aged 38 to 78 years old (average 54.77 ± 10.19 years old) who reported or referred to the Periodonal Department of Kaohsiung Medical University for seeking for Sandwich’s therapy [14]. Individuals had standard parallel method of full-mouth X-ray photography using the magnified images by 3.5 times, which initially destroyed angular bone. The distance of AB (RABL) and AC (root length) were measured using digital scanning radiographic image analysis(DSRIA) to determine the percentage (%) and millimeters of RABLs. Duplicate measurements were obtained from each tooth (Figure 2). All the measurements were numerically coded, and the results were processed and analyzed by the computer system equipped with the MIS [15,16]. Inferential statistics of Pearson product difference correlation, regression analysis and paired t-test according to the study assumptions and variation characteristics. P=0.05 is the significant standard value.
Results
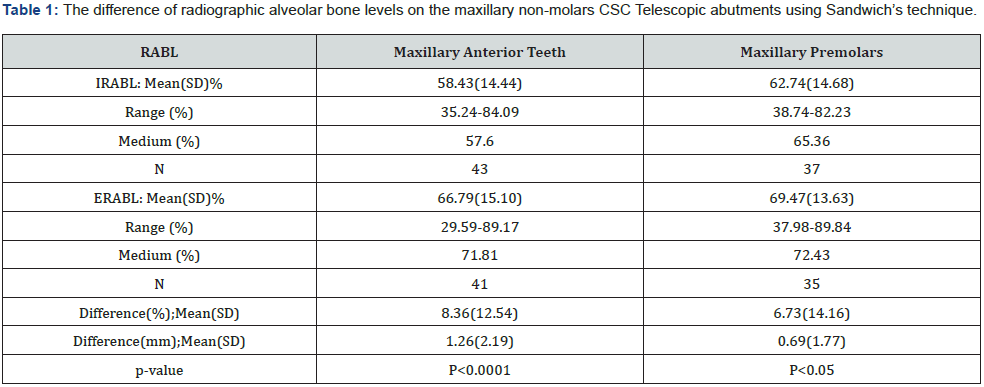
According to the classification of tooth type and position, non-molar teeth are collected as a total 43 upper anterior teeth, including incisors, and canine teeth. The total of 37 premolars are consisted the maxillary first and second premolars. In addition, a total 62 teeth consist of 31 mandibular anterior teeth (including mandibular central incisors, lateral incisors and canine teeth) and 31 premolars (including the first and second premolars), respectively (Table 1). The initial radiographic alveolar bone level (IRABL) of maxillary anterior teeth showed that the mean(SD) was 58.43% (±14.44%) and the end radiographic alveolar bone level (ERABL) was 66.79% (±15.10%). The mean (SD) of IRABL of the maxillary premolars was 62.74% (±14.68%) and ERABLs was 69.47%(±13.63)% (Table 1). The measurement of root length (mm) compared to that of alveolar bone height on the maxillary anterior teeth is obtained the mean (SD) 1.26 (±2.19) mm after treatment. The statistical analysis showed remarkable significance (p<0.0001). The differences of ERABLs and IRABLs of maxillary premolars are 0.69 (± 1.77) mm. The differences of ERABL and IRABL on maxillary premolars got a mean (SD) 0.69(±1.77) mm and revealed a statistically significant (p<0.05), respectively (Table 1).
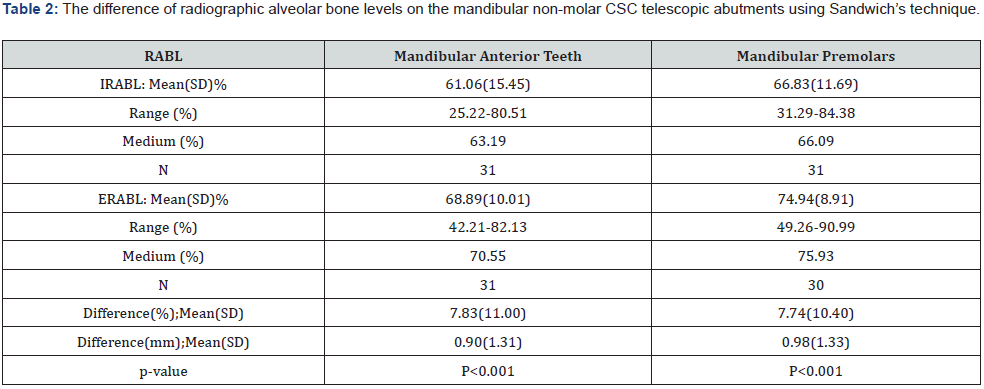
Table 2 The mean (SD) of IRABL of the mandibular anterior teeth was 61.06% (± 15.45%), and the mean(SD) of ERABL was 68.89% (±10.01%); The mean(SD) of IRABL on the mandibular premolars was 66.83% (± 11.69%) and ERABL was 74.94%(± 8.91%), respectively. The differences of ERABL and IRABL are 7.83(±11.0%) on the mandibular anterior teeth, where the differences of ERABL and IRABL are 7.74(10.40%) on the mandibular premolars, respectively. The measurement of root length (mm) compare to that of alveolar bone height (ABH) before and after treatment on the mandibular anterior teeth is obtained the mean (SD) 0.90(±1.31) mm after treatment, where the measurements of root length (mm) as compare to ABH on the lower premolars are 0.98(±1.33) mm. The mean (SD) of RABL on the mandibular premolars was greater than those of mandibular anterior teeth. In addition, Both mandibular anterior teeth and premolars (Table 2).
Discussion
It can be argued that the lose rate of periodontal attachment levels is influenced by some deteriorative factors such as type of plaque infection, host susceptibility, and the local environment of chronically inflamed tissue, pathologically deepened pockets resulted from foods impaction, ill-fitting restorations, crowding of teeth, morphology of alveolar bone, trauma from occlusion etc. Lindhe & Nyman [17] and Rosling et al. [18] reported that an effect of following proper periodontal therapy (teeth which exhibit severely reduced but healthy periodontium still exhibit a permanently increased mobility), does not diminish the increased mobility of the tooth, splinting of the teeth may be considered. This type of treatment is only in cases, however, during the recall phases or even during the pre-surgical period it becomes obvious that the reduced periodontal support around the teeth either in the entire dentition or in several parts of the individual’s arches with SAP may be insufficient to withstand force resulted from torque, occlusal, lateral directions. Left alone before, and following periodontal therapy, such teeth may be subjected to forces large enough, sooner or later to mechanically deteriorate the receiving periodontal supports and to extract the teeth.
The clinical data, reported from Nyman et al. [19] and Lundgren et al. [20] showed that permanent periodontal prosthesis can be hyper-mobility of isolated abutment teeth, especially even the prosthesis with a cross-arch design. More recent report in 2016 by Hou et al. [21] presented a study of case series for treatment of intentional replantation (IR) for periodontal compromised and hopeless teeth with extensive bone loss even teeth or beyond the apex. However, there still permitted prominent bone gain without bone grafting and got an 88.2% of overall cumulative survival rate. The present study is one of our long-term series studies regarding the nature teeth preservation using NSPT, TPP, and CSCTD periodontal prosthetic procedures. The present study also showed the difference of initial and end of RABLs in both the maxillary anterior teeth and maxillary premolars are 8.36(±12.54)%(equal to 1.26±2.19 mm) and 6.73(14.16)% (equal to 0.69mm); where there are mandibular anterior teeth 7.83(11.00)% (equal to 0.90±1.31mm) to 7.74(10.40)% (equal to 0.98±1.33mm) and premolars are 31.29 to 84.38%, respectively.
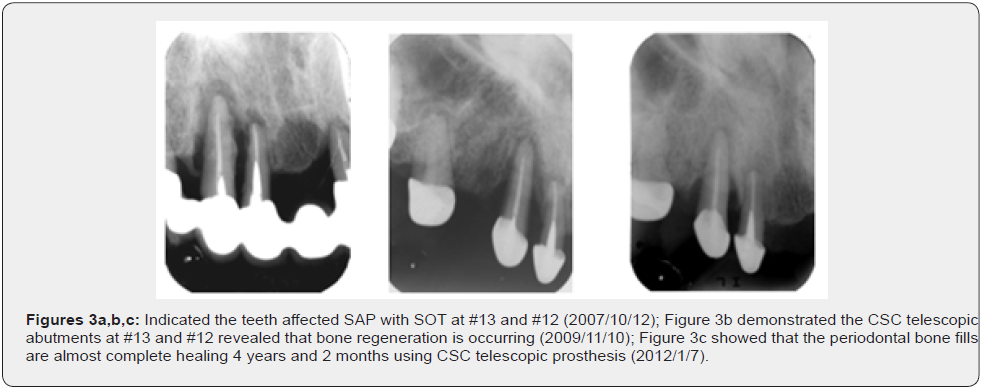
The Sandwich’s technique showed that the clinical followup periods were 6.71±2.51 yrs. Results illustrated conservative approaches of this technique including TPP, NSPT, and CSCTD prosthetic strategies are applied to evaluate not only maintain the periodontal health resolve teeth with SOT, but also got the periodontal bone gains from 0.69 mm to 1.26 mm on the maxillary anterior teeth and premolars, and 0.90mm to 0.98 mm, respectively. The result is consisted with the former reports that the TPP, NSPT, and periodontal prosthesis application will provide an effective method in treating SAP affected SOT (Figure 3a,b,c) [22]. Little literatures are available concerning the untreated subjects with adult periodontitis are documented using digital scanning radiographic analysis method (DSRIA) [23]. The present study indicated the differences of RABLs before and after periodontal and prosthetic treatment using TPP, NSPT and CSC telescopic denture design on the abutments of non-molars for the long-term study of abutments with SAP using DSRIA. This technique can effectively and precisely assess the changes of cumulative and annual alveolar bone levels each year [24]. Even may provide the difference of RABL between baseline data and the end of treatment, respectively.
References
- Yukna RA (1992) Clinical human comparison of expanded polytetrafluoroethylene barrier membrane and freeze-dried dura mater allografts for guide tissue regeneration of lost periodontal support. I. Mandibular molar class II furcation. J Periodontol 63: 431-442.
- Hou GL, Chen SF, Wu YM (1994) The topography of the furcation entrance in Chinese molars. Furcation entrance dimension. J Clin Periodontol 21(7): 451-456.
- Muller HP, Eger T, Langer DE (1995) Management of furcation-involved teeth – a retrospective analysis. J Clin Periodontol 22(12): 911-917.
- Rosling B, Nyman S, Lindhe L (1976).
- Polson AM, Heijl LC (1978) Osseous repair in intra-bony periodontal defects 5(1): 13-23.
- Hirschfeld L, Wasserman B (1978) A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol 49(5): 225-237.
- Ramfjord SP (1980) Root planning and curettage. Int Dent J 30(2): 93-100.
- McFall WT (1982) Tooth in in 100 treatment patients with periodontal disease: a long-term study. J Periodontol 53(9): 535-549.
- Renvert S, Badersten A, Nilvenus R (1981) JCP.
- Baderstein A, Nilvenus R, Egelberg J (1984) Effect of non-surgical periodontal therapy. III. Single versus repeated instrumentation 11(2): 114-124.
- Lindhe J, Socransky SS, Nyman S (1982) Critical probing depths in periodontal therapy. J Clin Periodontol 9(4): 323-336.
- Isidor F, Karring T (1986) Long-term effect of surgical and non-surgical periodontal treatment: a 5 –year clinical study. J Periodont Res 21(5): 462-472.
- Hou GL (2021) A long-term evaluation of bone levels using digital scanning radiographic image analysis on the CSC telescopic abutments in severe advanced periodontitis affected secondary occlusal traumatism. Advances in & Oral Health 14(5): 1-5.
- Hou GL, Hou LT (2019) Therapeutic outcomes using the Sandwich’s technique in treating severe advanced periodontitis with secondary occlusal traumatism: A long-term study for 5.1-39 years. Int J Dent and Oral Health 5(7): 76-85.
- Hou GL, Lin CH Yang YS, et al. (2000) The consistency and reliability of periodontal bone level measurements using digital radiographic image analysis – A pilot study. Kaohsiung J Med Sci 16(11): 566-573.
- Hou GL (2020) Digital scanning radiographic image analysis of alveolar bone loss in individuals with untreated adult periodontitis and aggressive periodontitis. A cross-sectional study. Adv Dent and Oral Health 13(4): 555870.
- Lindhe J, Nyman S (1975) The effect of plaque control and surgical pocket elimination on the establishment and maintenance of periodontal health. A longitudinal study of periodontal therapy in cases of advanced disease. J Clin Periodontol 2(2): 67-79.
- Rosling B, Nyman S, Lindhe J (1976) The effect of systematic plaque control on bone regeneration in infra-bony pockets. J Clin Periodontol 3(1): 38-53.
- Nyman S, Rosling B, Lindhe J (1975) Effect of professional tooth cleaning on healing after periodontal surgery. J Clin Periodontol 2(2): 80-86.
- Lundgren D, Rylander H, Laurell L (2009) To save or extract that is the question. Natural teeth or dental implants in periodontitis-suspectable patient: clinical decision-making and treatment strategies ecemplified with patient case presentation. Periodontology 2000 47: 25-50.
- Hou GL, Hung CC, Yang YS (2003) Radiographic alveolar bone loss in untreated Taiwan Chinese subjects with adult periodontitis measure by digital scanning radiographic image analysis method. Dentomaxillofacial Radiology 32(2): 104-108.
- Hou GL, Hou LT, Weisgold AS (2016) Survival rate of teeth with periodontally hopeless prognosis after therapies with intentional replantation and perioprosthetic procedures - a study of case series for 5-12 years. Clinical and Experimental Dental Research 2(2): 85-95.
- Hou GL (2020) Annually radiographic periodontal bone loss rates of tooth affected severe advanced periodontitis with secondary occlusal traumatism. Intern J Dent and Oral Health 6(6): 1-5.
- Hou GL (2021) Annual and cumulative radiographic alveolar bone loss rates using digital scanning image for the periodontal disease groups before and after periodontal treatment. European J Dental and Oral Health 2(3): 23-27.






























