Different Management for Patients with Two Types of Chronic Rhinosinusitis for their Oral Implant Therapy
Keiso Takahashi1*, Kosaku Yamazaki1, Mikiko Suzuki-Yamazaki2,3, Hiroshi Ito3 and Yuh Baba4
1Division of Periodontics, Department of Conservative Dentistry, Ohu University School of Dentistry, Tomita-machi Koriyama City, Japan
2Ohu University Dental Hospital, Ohu University School of Dentistry, Tomita-machi Koriyama City, Japan
3Division of Oral Pathology, Department of Oral Medical Science, Ohu University School of Dentistry, Tomita-machi Koriyama City, Japan
4Ohu University Dental Hospital Otorhinolaryngology, Ohu University School of Dentistry, Tomita-machi Koriyama City, Japan
Submission: June 26, 2021; Published: July 13, 2021
*Corresponding author: Keiso Takahashi, Division of Periodontics, Department of Conservative Dentistry, Ohu University School of Dentistry, Japan Adv
How to cite this article: Keiso T, Kosaku Y, Mikiko Suzuki-Y, Hiroshi I, Yuh B. Different Management for Patients with Two Types of Chronic Rhinosinusitis for their Oral Implant Therapy. Adv Dent & Oral Health. 2021; 14(4): 555894. DOI: 10.19080/ADOH.2021.14.555893
Abstract
Background: Maxillary sinus floor elevation surgery using lateral window technique (SES) is a reliable technique, however, care should be taken for this treatment for the patients with chronic rhinosinusitis.
Material and Methods: We present the different management of implant treatment and their prognosis of two patients with different types of chronic rhinosinusitis, neutrophilic chronic rhinosinusitis (NCS) and eosinophilic chronic rhinosinusitis (ECS), respectively. For a 69-year-old female with NCS, chronic rhinosinusitis was cured by long-term low-dose macrolide therapy as conservative treatment and then implant treatment was safely performed after SES. In contrast, for a 46-year-old male with ECS, SES were not performed because this patient showed the recurrence of polys after functional endoscopic sinus surgery performed by a previous otorhinolaryngologist. The implant overdentures were applied alternatively for the patient to avoid post-operative complications.
Conclusion: Collaboration between dentists and otorhinolaryngologists is necessary to get precise diagnosis of chronic rhinosinusitis and choose reasonable treatment regimen according to the pathological conditions of sinus.
Keywords: Maxillary sinus; Chronic rhinosinusitis; Neutrophilic chronic rhinosinusitis, Eosinophilic chronic rhinosinusitis; Dental implants
Abbreviations: SES: Maxillary sinus floor elevation surgery; CRS: Chronic rhinosinusitis; NCS: Neutrophilic chronic rhinosinusitis; ECS: Eosinophilic chronic rhinosinusitis; CBCT: Cone-beam computed tomography; LLMT: Long-term low-dose macrolide therapy; FESS: Functional endoscopic sinus surgery
Introduction
Maxillary sinus floor elevation surgery (SES) is a reliable technique [1]. However, this treatment is not riskless of postoperative complications such as maxillary rhinosinusitis and postoperative infection [2]. Especially, preoperative chronic rhinosinusitis (CRS) conditioning a stenosis of the maxillary sinus drainage pathways could cause postoperative acute maxillary rhinosinusitis in addition to the anatomical-structural impairments [3]. CRS is an inflammatory condition of the paranasal sinuses that most often causes chronic sinonasal symptoms such as facial pain/pressure, hyposmia/anosmia, nasal discharge. Then, preoperative CRS is diagnosed as a “reversible contraindication case” or “high-risk case” for SES in the field of ear, nose, and throat specialists (otorhinolaryngologists) [4]. Our dentists should perform SES after otorhinolaryngologists cures preoperative CRS to avoid possible postoperative complications after SES.
There are heterogeneous group of conditions that require multidisciplinary approach for CRS. One of the prominent features of CRS is persistent purulent nasal discharge and paranasal sinus effusion containing numerous neutrophils and is called as neutrophilic chronic rhinosinusitis (NCS) [5]. On the other hand, eosinophilic chronic rhinosinusitis (ECS) is a subgroup of CRS with nasal polyps, which is associated with severe eosinophilic infiltration and intractable [6]. The incidence of ECS is increasing in Japan and other countries, however, the reason is also still unknown and possible mechanisms including aberrant IgE production are discussed [7]. The lesion of ECS tends to be a predominant in the bilateral ethmoid sinus especially in early stage, while NCS tends to be predominantly occurred in the maxillary sinus. Both NCS and ECS could cause the stenosis of the maxillary sinus drainage pathways when the lesion is involved in the natural ostium of maxillary sinus. Therefore, care should be taken when we plan SES for the patients with CRS as described above, however, to the best of our knowledge, there was no report which explained detail clinical management and outcomes of different types of CRS. Here, we report different management and prognosis for two patients with different types of CRS, NCS and ECS.
Case Reports
NCS
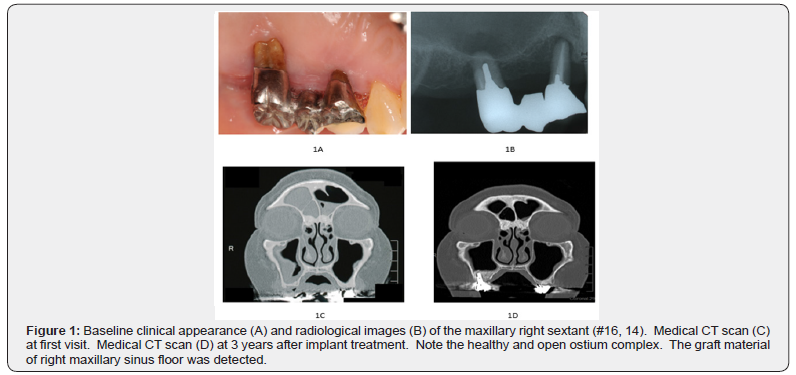
A 69-year-old Japanese female (patient A) came to our dental hospital in August 2016. Her chief complaint was a mobility of right maxillary molars because of her advanced periodontitis (Figure 1A, B). She had suffered Hashimoto’s disease and taken thyroid hormone for 35 years. She was a former smoker until 30 years ago. Preoperative cone-beam computed tomography (CBCT) indicated the thickness of the Schneiderian membrane at right maxillary sinus and inadequate bone volume to support dental implant placement (data not shown). There was no history of any operation in head and neck, and she did not have nasal allergy, however she had olfactory disorder (no smell) and stuffy nose for many years. Then, we asked consultation of otorhinolaryngologist (YB) in our dental hospital. CT examination indicated unclear images because of thickening of paranasal sinus mucosa at bilateral frontal and right maxillary sinus (Figure 1C). Neither nasal polyp nor allergic/inflammatory reaction was observed in nasal endoscopic examination (data not shown). The patient A was diagnosed as a right maxillary chronic rhinosinusitis without allergic rhinitis that is assessed as a “reversible otorhinolaryngological contraindication” to SES.
Case Management
After extracting hopeless teeth (#16, 14), partial denture was inserted for oral rehabilitation at first. This patient wanted to be able to chew with back site by implant therapy. We explained to treat her CRS and this regimen may be advantageous to suppress post-operative complications after SES. In general, oral or topical steroids with or without antibiotics tend to be used for management of CRS, however, few inflammatory reactions were found by nasal endoscopic examination and then preoperative medication, orally 200 mg Clarithromycin and L -Carbocisteine Tab. 250mg, were administered for 3 months by YB in October 2016.
Clinical Outcomes
Her chief complaint had completely improved three months later, although CT images was not dramatically changed (data not shown). She underwent SES at right maxillary sinus with bone graft materials by KT in October 2017. No intraoperative complication was occurred. After operative antibiotic prophylaxis (Amoxicillin hydrate) was also medicated for 3 days. After SES, no clinical symptoms had been occurred, and then no more medical treatment, including nasal and oral corticosteroids was performed. The postoperative course was uneventful after 4 months follow-up evaluation and then 3 implants (Nobel Biocare, Zurich, Switzerland) with a diameter of 4.2 mm and a length of 10 mm, were inserted at #16 - #14 in accordance with the surgical stent by KT under local anesthesia in February 2018. Postoperative prescriptions included Amoxicillin hydrate, three times daily for 3 days. Four months later, all implants were found to be osseointegrated, and then the definitive prosthesis was attached. The follow-up CT scan revealed a clear and pneumatized right maxillary sinus with slight thickness of the Schneiderian membrane at 3 years after SES (Figure 1D). The patient A was satisfied with her current good occlusal function and there has been no recurrence of otorhinolaryngological complications including rhinosinusitis to date.
ECS
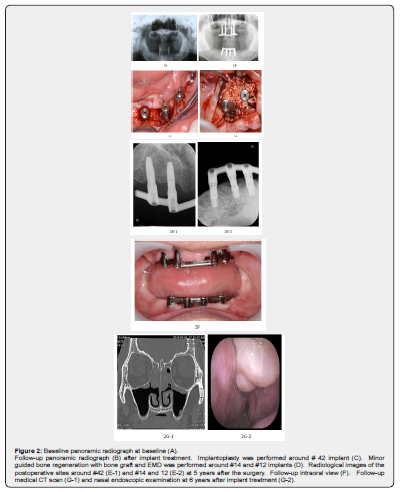
A 46-year-old Japanese male (patient B) came to our dental hospital in May 2011. He wanted to be able to chew by implant therapy rather than denture. He has lost his almost all teeth because of his advanced periodontitis (Figure 2A). He was a former smoker until last year. Preoperative CBCT indicated the slight thickening of paranasal sinus mucosa at bilateral maxillary sinus and inadequate bone volume to support dental implant placement at maxillary area (data not shown). From his medical interview, we knew that he had been diagnosed as an ECS and nasal septal curvature, and then nasal septal correction and bilateral functional endoscopic sinus surgery (FESS) had been performed by the otorhinolaryngologist in a previous hospital in October 2010. Although we were concerned postoperative complications after SES, this otorhinolaryngologist did not notice any possible postoperative complications by implant therapy with SES.
Case Management
After extracting hopeless teeth (#33, 43), full denture was inserted for oral rehabilitation at first. We decided to perform implant treatment only at incisor and premolar areas and implant overdenture was applied for his oral rehabilitation to avoid SES in August 2011. Eight implants (Nobel Biocare) were inserted into both maxilla and mandibular with bone graft material (Osteograft-S®, Kyocera Co., Japan) by KT in February and April 2012. No intraoperative complication was occurred. After operative antibiotic prophylaxis (Amoxicillin Hydrate) was also medicated for 3 days. After implant therapy, no clinical symptoms had been occurred. The postoperative course was uneventful after 4 months follow-up evaluation and then implant overdentures with dolder bar were inserted in March 2012 (Figure 2B).
After implant treatment, he has irregularly attended to our dental hospital and supportive therapy has been performed, however, he could not keep good oral hygiene and then suffered from peri-implantitis in September 2015. He was also diagnosed an obstructive sleep apnea, and then oral appliance for sleep was made in our dental hospital in January 2016. After non-surgical treatment, implantoplasty (Figure 2C) and guided bone regeneration (GBR) with enamel matrix derivative (EMD) gel (Straumann, Zurich, Switzerland) and bone graft (Apacerum-AX®) at #26 (Figure 2D) was applied in June and August 2016, respectively. Then, inflammatory reaction was mostly disappeared and bone around treated implant appeared to be stable (Figure 2 E-1, E-2). The patient B attended our dental hospital and asked additional implant treatment for his back sites, although implant overdentures are still working well in August 2018 (Figure 2 F). We asked consultation of otorhinolaryngologist (YB) in our dental hospital. CT examination indicated unclear images because of thickening of paranasal sinus mucosa at both ethmoidal sinus (Figure 2G-1). In addition, both nasal polyp and allergic/inflammatory reaction was observed in nasal endoscopic examination (Figure 2 G-2). Although L-Carbocisteine Tab. 250mg three times daily, Pranlukast hydrate 4 caps 2 times daily, and topical steroid were administered for 48 days by YB in September 2018, this treatment did not decrease the size of nasal polyps. Thus, the patient was diagnosed as polyp recurrence by ECS that was assessed as an “otorhinolaryngological irreversible contraindication” to SES (4). We had decided to do no additional implant treatment with SES and explained to him. Finally, he agreed with our decision and wanted an additional overdenture as a spare.
Discussion
This case reports showed our decision making for implant treatment for two different types of CRS, NCS and ECS. NCS can be treated conservatively with LLMT, while ECS cannot be treated well at present and then alternative plan was chosen without SES. LLMT for NCS is strongly recommended as conservative treatment in Japan [8], although this treatment regimen is still controversial in other guidelines. Otorhinolaryngologists perform this treatment to patients with NCS in order not to eliminate bacteria at sinus area but change the status of biofilms or reduce inflammatory reaction. Furthermore, it has been reported that this therapy is only effective in those individuals with low serum IgE [9], suggesting that this effect may be limited to those individuals with NCS, as opposed to ECS. Therefore, we have chosen LLMT in this case from the standpoint of anti-inflammatory effect of macrolide. If this medical treatment had been failed, FESS is only recommended for patients with NCS, although FESS was not done because patient A recovered her symptoms after LLMT. Medical conservative therapy for chronic rhinosinusitis before SES includes pre-operative administration of topical steroid in addition to LLMT [3]. However, we did not use any anti-allergic drugs for patient A because no allergic reaction was found.
On the other hand, conservative and/or surgical treatment using FESS technique is also used for ECS, however, these treatments are only partly effective for ECS [10]. In addition, the recurrence rate after these treatments for ECS is high [7]. In fact, polyp recurrence of ECS was observed in patient B (Figure 2 G-2). Thus, we have decided treatment plan according to the ENT assessment as described before [4]. Implant overdenture and implant-assisted partial denture may be candidates for implant-associated oral rehabilitation without SES as described in this report. We had at first contacted with the otorhinolaryngologist who had treated patient B by FESS in October 2010. He made a guarantee for us any dental treatment was not problematic. However, we avoided SES and implant treatment at maxillary sites because we had been worried for the polyp recurrence and possible complications. The second otorhinolaryngologist (YB) whom we asked consultation, agreed with our previous decision, suggesting that decision making is changeable among otorhinolaryngologists. Therefore, it would be recommended to work with otorhinolaryngologists who are familiar with dental treatment including SES to obtain a precise diagnosis for CRS and adequate treatment regimen according to the status of patients to minimize postoperative adverse events.
We selected two staged approaches for patient A (with bone grafting in one stage and implant placement in a later stage) to avoid the risk of infection of grafted materials and inserted implants by postoperative rhinosinusitis. Implant treatment is also not riskless as well as SES, and then we need to select safer treatment regimen as much as possible. Patient B has been suffered from peri-implantitis. We had performed implantoplasty at #42 (Figure 2C) and EMD and bone graft were added to regenerate bone around the #12 (Figure 2D). Although our treatment is now successful, the possibility of the recurrence of peri-implantitis still exists in the patient B. There is not an actual “gold standard” treatment showing the most favorable results for CRS and peri-implantitis at present. Therefore, more clinical data and scientific evidence should be added in the future. Further, implant-assisted oral rehabilitation with or without SES for patients with advanced periodontitis and CRS should be carefully considered.
Conclusions
These two cases suggest that precise diagnosis and personalized medicine according to the different types of CRS is crucial to minimize postoperative complications after SES and implant treatment for atrophic maxilla. Implant treatment with SES is associated with both sides between dentists and otorhinolaryngologists, therefore, we need to obtain reliable information from otorhinolaryngologists who are familiar with dental treatment including SES.
References
- Vazquez JCM, Angel de Rivera SG, Gil HS, Mifsut RS (2014) Complication rate in 200 consecutive sinus lift procedures: guidelines for prevention and treatment. J Oral Maxillofac Surg 72(5): 892-901.
- Schwartz-Arad D, Herzberg R, Dolev E (2004) The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol 75(4): 511-516.
- Kim JS, Choi SM, Yoon JH, Lee EJ, Yoon J, et al. (2019) What affects postoperative rhinosinusitis and implant failure after dental implant: a meta-analysis. Otolaryngol Head Neck Surg 160(6): 974-984.
- Pignataro L, Mantovani M, Torretta S, Felisati G, Sambataro G (2008) ENT assessment in the integrated management of candidate for (maxillary) sinus lift. Acta Otorhinolaryngol Ital 28(3): 110-119.
- Suzuki H, Ikeda K (2002) Mode of action of long-term low-dose macrolide therapy for chronic rhinosinusitis in the light of neutrophil recruitment. Curr Drug Targets Inflamm Allergy 1(1):117-126.
- Ishitoya J, Sakuma Y, Tsukuda M (2010) Eosinophilic chronic rhinorhinosinusitis in Japan. Allergol Int 59(3): 239-245.
- Fujieda S, Imoto Y, Kato Y, Ninomiya T, Tokunaga T, et al. (2019) Eosinophilic chronic rhinorhinosinusitis. Allergol Int 68(4): 403-412.
- Shimizu T, Suzaki H (2016) Past, present and future of macrolide therapy for chronic rhinosinusitis in Japan. Auris Nasus Larynx 43(2): 131-136.
- Wallwork B, Coman W, Mackay-Sim A, Greiff L, Cervin A (2006) A double-blind, randomized, placebo-controlled trial of macrolide in the treatment of chronic rhinosinusitis. Laryngoscope 116(2): 189-193.
- Matsuwaki Y, Ookushi T, Asaka D, Mori E, Nakajima T, et al. (2008) Chronic rhinosinusitis: risk factors for the recurrence of chronic rhinosinusitis based on 5-year follow-up after endoscopic sinus surgery. Int Arch Allergy Immunol 146(Suppl 1): 77-81.






























