Complications of Oral and Peri-Oral Piercings Among Group of Females Living in Riyadh City of Saudi Arabia
AlBandary Hassan AlJameel*, Salwa Abdulrahman AlSadhan, Mashael Sulaiman AlOmran and Nassr Saleh Al-Maflehi
Department of Periodontics and Community Dentistry, College of Dentistry, King Saud University, Riyadh, Kingdom of Saudi Arabia
Submission: June 01, 2020; Published: June 08, 2020
*Corresponding author: AlBandary Hassan AlJameel, Department of Periodontics and Community Dentistry, College of Dentistry, King Saud University, Saudi Arabia
How to cite this article: AlBandary H A, Salwa A A, Mashael S A, Nassr S A-M. Complications of Oral and Peri-Oral Piercings Among Group of Females Living in Riyadh City of Saudi Arabia. Adv Dent & Oral Health. 2020; 12(4): 555845. DOI: 10.19080/ADOH.2020.12.555845
Abstract
Background: Body piercing, including oral & peri-oral piercing, is the practice of puncturing specific sites of the body to adorn them with decorative ornaments. Although such practice is common, little is known about it in Arab countries including Saudi Arabia.
Aim: Therefore, the aim of this study was to assess oral piercing related complications and the level of awareness of these complications among a group of female users of oral and peri-oral piercing living in Riyadh, Saudi Arabia.
Method: To reach the study aim, an on-line, Arabic questionnaire was developed by reviewing relevant literature and was pilot tested, then it was distributed targeting females living in Riyadh, Saudi Arabia. The collected data was entered and analyzed using Statistical Package for Social Sciences (SPSS) version 22.0.
Results: The results revealed that the majority of females who had oral piercings were 17-25 years of age, with the lips being the most reported site of oral piercing (81%), and aesthetics being the main reason (84.1%) for having the piercing. Almost 13% reported that they received their piercings from a person without professional piercing qualification, and 57.1% reported that they were not made aware of the potential risks to oral health associated with the piercing. With regards to complications, 36.5% reported discomfort, 15.9% reported bad breath, and 3.2% chipped teeth. In conclusion, oral piercing seems to be gaining popularity among Saudi population and further research is needed to better understand this phenomenon.
Keywords:Oral piercing; Peri-oral piercing; Complications; Saudi Arabia; Cross-sectional study
Abbreviations: PMMA: Polymethyl methacrylate; PTFE: Polytetrafluorethylene; HIV: Human immunodeficiency virus; HSV: Herpes simplex; EBV: Epstein-Barr viru
Introduction
Body piercing is the practice of puncturing specific sites of the body to adorn them with decorative ornaments [1]. Piercing of body parts, including the oral and peri-oral regions, was once a cultural practice having ancient origins with deep rooted religious, tribal or sexual symbolism whilst also indicating ceremonial hierarchies among members of the society [2,3]. Today, this practice has re-emerged among the youth and is gaining popularity as a form of self-expression [4]. The major contributing factors for youth choosing to pierce their bodies include a desire to be fashionable [5]. Body piercings in the contemporary world are also attributed to religion, traditional or occult rituals, expression of independence of the spirit, body, and sensuality [6,7]. It is also believed to be a form of therapeutic healing from depression which suggests that piercing maybe correlated to psychological trauma [6,7]. Until recently body piercings were culturally restricted but due to rapid globalization and massive cross-cultural exchange through internet, television and other pop culture mediums, this practice has been widely adopted by different cultures. Body piercing usually involves sites such as the nose, earlobes, eyebrows, navel, nipples and occasionally, the genitals [8]. However, it is the oral and peri-oral piercing sites that are of special interest to the dental practitioner.
Oral and peri-oral piercings generally involve sites such as the lips, tongue, cheeks, lingual and labial frenulum and the uvula or a combination of these. A needle is inserted to create an aperture through which a jewelry is then installed [5,9]. According to Vozza and his colleagues (2015), the tongue was the most commonly pierced oral site.8 Piercing jewelry comes in a wide range of shapes and sizes but the most commonly used oral piercing jewelry include the labret, barbell, captive rings and magnetic studs [10]. A variety of materials are used to manufacture these jewelries and include surgical stainless steel, chrome-cobalt alloys, nickel, copper, brass, niobiun, titanium, silver, 14 or 18K gold and platinum [11]. Synthetic materials like polymethyl methacrylate (PMMA), polytetrafluorethylene (PTFE) and tygon are also used for making piercing jewelry as well as natural materials like bone, ivory, horn, wood and stone [12,13].
Complications of oral piercings, both local and systemic, have been extensively discussed in the literature and they can have severe health consequences [12,14,15]. Local complications of oral and peri-oral piercing may include pain, persisting bleeding, nerve damage, swelling, infection, gingival trauma, gingival recession, chipped or fractured teeth, tooth sensitivity, halitosis, increased salivary flow, metal hypersensitivity, accidental aspiration of the piercing and interference with speech and swallowing [14,15]. Tongue piercing, which is usually done at the midline just anterior to the lingual frenum may result in the colonization of peri-odontogenic bacteria at the pierced site in the absence of proper oral hygiene measures leading to soft tissue lesions in the tongue [13]. Delayed local complications like bifid tongue, atypical trigeminal neuralgia and hypertrophic keloid lesions are also associated with oral piercings [16]. Apart from these local complications, oral piercing can also lead to the transmission of blood borne viruses like human immunodeficiency virus (HIV) and hepatitis (HAV, HBV, HCV), herpes simplex (HSV) and the Epstein- Barr virus (EBV) causing systemic complications.16 Furthermore, bacterial pathologies such as Neisseria and Streptococcus viridans induced endocarditis and Ludwig’s angina have also been identified as systemic complications of oral piercing [16].
Despite being associated with a myriad of health problems, oral piercing is still popular among young people, and dental health-care professionals are facing a growing number of patients that present with oral piercings [17]. This could be attributed to a general lack of awareness with regards to the complication of oral and peri-oral piercings [1]. Levin and colleagues [18] conducted a study on 389 young adults and reported that 57.8% of them were unaware of the complications related to oral piercings [18]. Similarly, a study conducted on an Italian sample of 225 teenagers found that only 25.3% were aware of the risk of HCV cross-infection, and only 17.3% reported of knowledge about risk of endocarditis [8]. In another study conducted in Italy, Gallè et al. [19] found that out of the 3,868 young adults participating in the study, 84.4% knew the infectious risks associated with body piercing but only 4.1% of them correctly identified the infectious diseases which can be transmitted through these procedures; while 59.2% declared that noninfectious diseases can occur after a tattoo or a piercing, but only 5.4% of them correctly identified them [19]. These global trends require dental health-care providers to be aware of the related concerns and to be able to provide accurate information to patients considering the use of oral piercings. While reports from around the world assessing the awareness of people regarding complication of oral piercings are found in dental literature, no such studies have been conducted in the Kingdom of Saudi Arabia. The aim of the present study was to assess oral piercing related complications and level of awareness of these complications among female users of oral and peri-oral piercing living in Riyadh, Saudi Arabia.
Materials and Methods
Study Design
The present study was a descriptive, cross-sectional study conducted on a sample of females living in Riyadh, Saudi Arabia.
Questionnaire Design
A self-administered, close-ended questionnaire was created by reviewing the literature on oral and peri-oral piercings. The questionnaire was made up of 18 items. It was initially created in English and later translated into Arabic. The questionnaire was distributed among females with oral piercing living in Riyadh. An online version of the questionnaire was created and published on Google drive in order to reach a larger number of participants. The questionnaire contained items pertaining to demographic data including age, nationality, and any smoking habits, in addition to questions related to the piercing such as location, cleaning frequency, reason for having the piercing done, component and style of the jewelry, and complications related to the piercing such as tooth fractures, gingival inflammation and infections. Before launching the questionnaire, it was pilot-tested and evaluated for clarity of wording, readability, and layout.
a) Inclusion criteria
i. Females living in the city of Riyadh who can speak, read and understand Arabic.
ii. Aged above 13 years.
iii. Females who already have oral and peri-oral piercings.
b) Exclusion criteria
i. Females who cannot speak, read, and understand Arabic.
ii. Females having body piercings other than oral and perioral.
Data Analysis
The participants’ responses were coded, summarized, and entered into a spreadsheet software (Statistical Package for Social Sciences, SPSS 22.0, IBM.USA). Frequency distribution of participants’ responses was calculated using simple descriptive statistics and inferences were drawn.
Results
A total number of 63 participants completely filled the questionnaire. Nearly 80% of them were in the age group of 17-25 years with only 6.3% below the age of 17 years. The majority of the participants (98.4%) were Saudis, and nearly half of them (50.8%) stated that they were smokers (Table 1). As shown in Table 2, most of the study sample had lip piercings (81%), and 14.3% had tongue piercings while only 4.8% had piercings in their cheeks. Over half of the respondents (52.4%) got their piercings done less than a year ago while only 14.3% have their oral piercings for more than 4 years. When asked about purpose of getting oral piercing, over three quarters of the respondents stated that esthetics was their main purpose of getting it done. Regarding the style of the piercing jewelry worn, the barbell was the most commonly type worn (58.7%) followed by the ball captive ring (23.8%). More than two thirds of the study sample (68.3%) were unaware of the component of their oral jewelry while among those who did know, titanium and “others” were equal choices (12.7%). Around 90% of the respondents had their oral piercings done by a professional, and 57.1% were not made aware of potential risks associated with oral piercing. When they were asked about recommending piercing to someone else, almost half of the study sample (54%) stated that they would recommend others to get oral piercings done (Table 2).
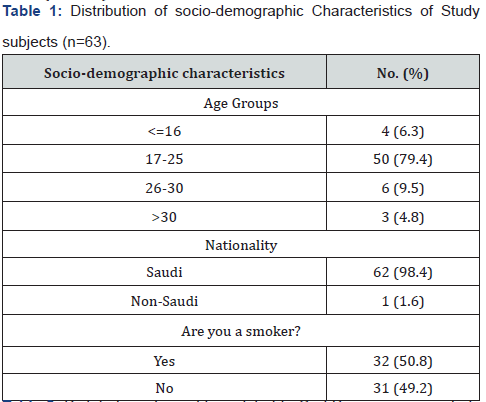
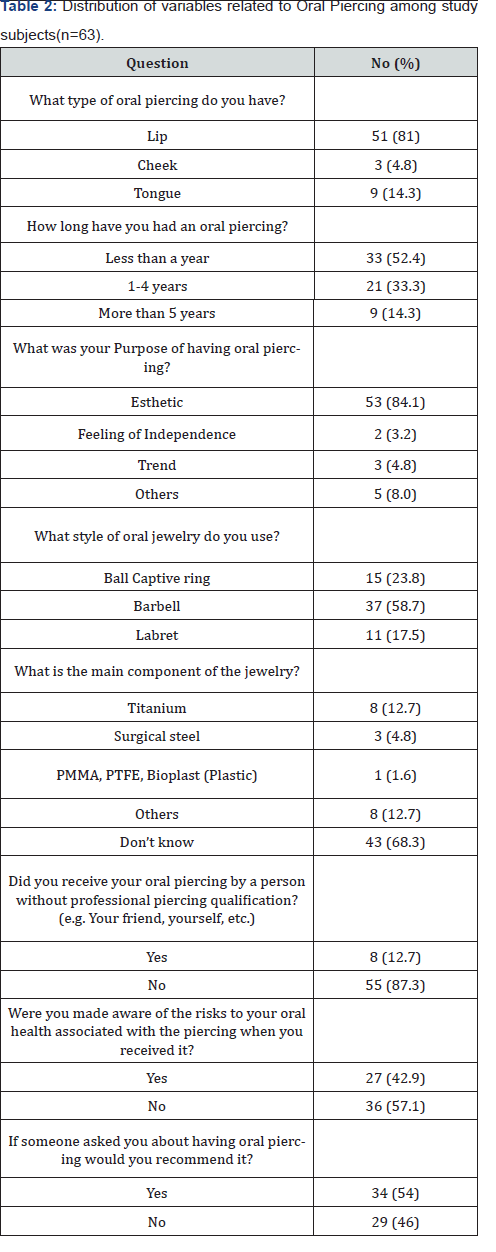
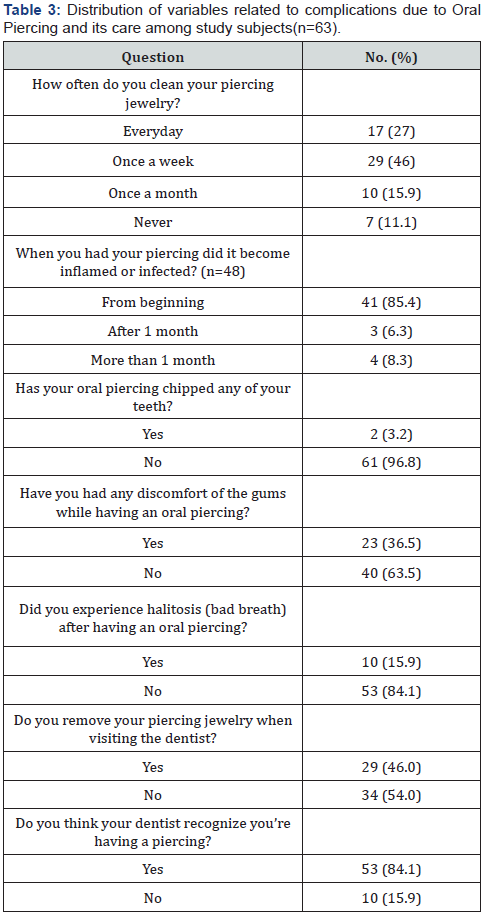
Table 3 depicts information related to the oral hygiene behavior of the participants and their awareness/experiences pertaining to complications of oral piercing. Only 27% of the participants reported that they cleaned their piercing every day, whereas 11.1% never cleaned them. With regards to the complications related to the piercing, 85.4% of the subjects had inflamed tissues around the piercings at the beginning of having them done. About 37% had discomfort in their gingival tissues, and early 15.9% experienced halitosis while having their oral piercings. Only 3.2% of the respondents stated that the piercing caused chipping of their teeth. Over half of the subjects (54%) do not remove their piercing jewelry when visiting their dentist, and only 15.9% of participants think that their dentists do not recognize that they have oral piercings.
Discussion
This present research aimed at assessing oral piercing related complications and level of awareness of these complications among female users of oral and peri-oral piercing living in Riyadh, Saudi Arabia. The results of this study revealed that the majority of the females who had oral piercings were 17-25 years of age, which indicated that such habit is common and teenagers and young adults. Also results showed that the lips seemed to be the most favored site for oral piercing among the sample. Other studies reported similar findings as the lips being the most commonly pierced site [9,20]. This could be attributed to the fact that piercings on lips are most visible and more esthetically located. Over three quarters of the participants in this study reported esthetics as the reason for oral piercings; so, the lips seem to be a natural option. Esthetics as the main motive for oral piercings has also been reported by another study which found that the main reason for piercings among youth is to look fashionable [5]. Studies conducted by Garcia-Pola et al. [21], Plessas & Peppalasi [22] also showed esthetics as the main reason for piercings [21,22]. This also accounts for the fact that the most commonly reported delayed complication in the current study was gingival tissue irritation which is commonly associated with lip piercings [23]. The tongue was the next most pierced site although it accounted for only 14.2% of piercings in this study. The most common complication associated with tongue piercing is tooth chipping/cracked tooth syndrome [24]. In the present study, only 3.2% of the participants stated that they suffered from chipped teeth due to oral piercing. In 2016, a systematic review conducted by Hennequin-Hoenderdos and colleagues reported that individuals with tongue piercings were more likely to experience tooth injuries than those without tongue piercings, and tooth injuries were found in 37% of all observed cases in the review [23]. The lower incidence of tooth injuries in this study could be attributed to the fact that lesser number of participants in this study sample had tongue piercings as compared to lip piercings. With regards to the style of piercing jewelry worn, the majority of the participants wore the barbell type. This design of oral jewelry is most frequently associated with tooth chippings and cracked tooth syndrome [11,25,26] but this is not the only factor that determines tooth injury. Tongue jewelry, habitual biting or chewing of the device, barbell stem length, the size of the ornament attached to the barbell, and the type of material used in it may all cause trauma to the teeth [27]. Hence, despite the barbell being the predominantly worn jewelry type in this study, the incidence of chipped teeth was very low due to the fact that higher number of the participants had lip piercings as compared to tongue piercings which is the most commonly associated site with tooth fracture. The Association of Professional Piercers recommend that piercing should only be done using biosafe materials like stainless steel or titanium, 14K gold or higher, platinum or PTFE (Teflon) [28]. However, studies reported that stainless steel jewelry is more prone to bacterial accumulation than jewelry made from plastics such as Teflon and recommend that wearing plastic jewelry poses less risk for infection than ones made of metal [2]. It is important that people who want to get oral piercings done are well-informed about the range of materials available to choose from, and which materials are recommended that present the least threat of causing oral hard and soft tissue complications. Having a large number of respondents in our study got their oral piercings by a piercing professional is a positive trend, however, more than half of the respondents were not made aware of the associated risks. These findings are similar to a study conducted in Italy where 53.7% of the participants did not receive any information on risks associated with piercings from piercing professionals [8]. This could be attributed to the fact that these piercing professionals are either not aware of the risks or prefer not to disclose the risks in order to not scare away customers and lose business. This puts a lot of responsibility on the dentists who are visited by patients with piercings do educate them on potential risks and complications.
When hygiene habits related to oral piercings were surveyed, it was found that less than one-third of the respondents cleaned their piercings every day. The American Dental Association recommends keeping the pierced site free of food debris by using a mouth rinse after every meal. To reduce risks of oral infection after piercing procedures, pierced individuals should be advised to maintain a standard oral hygiene regimen that includes: twicedaily tooth-brushing using fluoride-containing toothpaste and a soft-bristle toothbrush; regular use of floss or another interdental cleaner; and use of alcohol-free mouth rinse during and after the healing period [29]. When compared with these recommendations, the oral hygiene awareness, and practices of pierced individuals in this study are inadequate. To add to that, half of the respondents were also smokers which, coupled with inadequate cleaning of the pierced site can be the reason for halitosis being a complication among 15.9% of the respondents. This could also easily turn into a vicious cycle as smoking is known to be a contributing factor for plaque accumulation [30]. A limitation of this study was the small sample size which could be attributed to cultural influences which do not encourage individuals with oral piercings to be identified and participate in surveys despite assurances of anonymity. Due to lack of previous research on this subject in Saudi Arabia, it was not possible to gather information on current local guidelines with respect to body piercings. Furthermore, it was not within the scope of this research to screen the participants for blood borne diseases and establish correlations with oral piercings.
Conclusion
Despite the limitations of this study, it can be concluded that oral and peri-oral piercing is a practice that is gaining popularity among Saudi females, and esthetics is their main motivation for getting piercings. Gingival discomfort and halitosis were found to be the main complications associated with piercings in our study. The level of awareness among the sample regarding piercing complications and oral health practices was found to be inadequate. There is also a need for further research among the Saudi population to include larger sample sizes and across different cities as well as to establish correlations of demographic and psycho-social factors with oral piercings and related complications locally and systemically.
Clinical Significance
As results indicated low level of awareness among the sample regarding piercing complications and oral health practices, this presents a need for dental health care providers to update themselves of oral health guidelines and complications of oral piercings so as to educate patients who present to them with piercings.
References
- Plastargias I, Sakellari D (2014) The consequences of tongue piercing on oral and periodontal tissues. ISRN dentistry 2014: 876510.
- Maspero C, Farronato G, Giannini L, Kairyte L, Pisani L, et al. (2014) The complication of oral piercing and the role of dentist in their prevention: a literature review. Stomatologija 16(3): 118-124.
- Vozza I, Fusco F, Bove E, Ripari F, Corridore D, et al. (2014) Awareness of risks related to oral piercing in Italian piercers. Pilot study in Lazio Region. Annali di stomatologia 5(4): 128.
- Randall JA, Sheffield D (2013) Just a personal thing? A qualitative account of health behaviours and values associated with body piercing. Perspectives in public health 133(2): 110-115.
- Chimenos-Küstner E, Batlle-Travé I, Velásquez-Rengijo S, Garcia-Carabano T, Vinals-Iglesias H, et al. (2003) Appearance and culture: oral pathology associated with certain" fashions"(tattoos, piercings, etc.). Medicina oral: organo oficial de la Sociedad Espanola de Medicina Oral y de la Academia Iberoamericana de Patologia y Medicina Bucal 8(3): 197-206.
- Greif J, Hewitt W, Armstrong ML (1999) Tattooing and body piercing: Body art practices among college students. Clinical Nursing Research 8(4): 368-385.
- Stirn A (2003) Body piercing: Medical consequences and psychological motivations. The Lancet 361(9364): 1205-1215.
- Vozza I, Fusco F, Corridore D, Ottolenghi L (2015) Awareness of complications and maintenance mode of oral piercing in a group of adolescents and young Italian adults with intraoral piercing. Medicina oral, patologia oral y cirugia buccal 20(4): e413.
- Hennequin‐Hoenderdos NL, Slot DE, Van der Weijden GA (2011) Complications of oral and peri‐oral piercings: a summary of case reports. International journal of dental hygiene 9(2): 101-109.
- Inchingolo F, Tatullo M, Abenavoli FM, Marrelli M, Inchingolo AD, et al. (2011) Oral piercing and oral diseases: a short time retrospective study. International journal of medical sciences 8(8): 649-642.
- Barbería Leache E, García Naranjo AM, González Couso R, Gutiérrez González D (2006) Are the oral piercing important in the clinic. Dental Pract 1: 45-49.
- Escudero-Castaño N, Perea-García MA, Campo-Trapero J (2008) Oral and perioral piercing complications. The open dentistry journal 2: 133.
- Ziebolz D, Hornecker E, Mausberg RF (2009) Microbiological findings at tongue piercing sites–implications to oral health. International journal of dental hygiene 7(4): 256-262.
- Firoozmand LM, Paschotto DR, Dias Almeida J (2009) Oral piercing complications among teenage students. Oral health & preventive dentistry 7(1): 77.
- Singh A, Tuli A (2012) Oral piercings and their dental implications: A mini review. Journal of investigative and clinical dentistry 3(2): 95-97.
- Oberholzer TG, George R (2010) Awareness of complications of oral piercing in a group of adolescents and young South African adults. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 110(6): 744-747.
- Francu LL, Calin DL (2012) Lingual piercing: dental anatomical changes induced by trauma and abrasion. Romanian Journal of Functional & Clinical, Macro-& Microscopical Anatomy & of Anthropology/Revista Româna de Anatomie Functionala si Clinica, Macro si Microscopica si de Antropologie 11(1).
- Levin L, Zadik Y, Becker T (2005) Oral and dental complications of intra‐oral piercing. Dental Traumatology 21(6): 341-343.
- Gallè F, Quaranta A, Napoli C, Di Onofrio V, Alfano V, et al. (2012) Body art practices and health risks: young adults’ knowledge in two regions of southern Italy. Ann Ig 24(6): 535-542.
- Farah CS, Harmon DM (1998) Tongue piercing: case report and review of current practice. Australian Dental Journal 43(6): 387-389.
- Garcia-Pola MJ, Garcia-Martin JM, Varela-Centelles P, Bilbao-Alonso A, Cerero-Lapiedra R, et al. (2008) Oral and facial piercing: Associated complications and clinical repercussion. Quintessence international 39(1): 51-59.
- Plessas A, Pepelassi E (2012) Dental and periodontal complications of lip and tongue piercing: prevalence and influencing factors. Australian Dental Journal 57(1): 71-78.
- Hennequin‐Hoenderdos NL, Slot DE, Van der Weijden GA (2016) The incidence of complications associated with lip and/or tongue piercings: a systematic review. International journal of dental hygiene 14(1): 62-73.
- Campbell A, Moore A, Williams E, Stephens J, Tatakis DN (2002) Tongue piercing: impact of time and barbell stem length on lingual gingival recession and tooth chipping. Journal of periodontology 73(3): 289-297.
- De Urbiola Alís I, Viñals Iglesias H (2005) Some considerations about oral piercings. Av Odontoestomatol 21(5): 259-269.
- Peticolas T, Tilliss TS, Cross-Poline GN (2000) Oral and perioral piercing: a unique form of self-expression. The journal of contemporary dental practice 1(3): 30-46.
- Di Angelis AJ (1997) The lingual barbell: a new etiology for the cracked-tooth syndrome. Journal of the American Dental Association 128(10): 1438-1439.
- Association of Professional Piercers. Picking your piercer (2010). choosing-a-piercer.
- American Dental Association. Department of Scientific Information (2019), ADA Science Institute.
- Haffajee AD, Socransky SS (2001) Relationship of cigarette smoking to the subgingival microbiota. Journal of clinical periodontology 28(5): 377-388.