Ramsay Hunt Syndrome: Case Presentation and Management
Ghofran M Hamouda1, Yousif I Eltoham2*, Ahmed Altayeb3, Abusofyan Salih4 and Ahmed M Suleiman5
1 Faculty of Dentistry, University of Alneelain, in Khartoum, Sudan
2,3,5 Department of Oral and Maxillofacial Surgery, University of Khartoum, Sudan
4 Department of Oral and Maxillofacial Surgery, King Khalid University, Sudan
Submission: March 13, 2020; Published: April 10, 2020
*Corresponding author: Yousif Idris Yousif Eltohami, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, University of Khartoum, Sudan
How to cite this article: Ghofran M H, Yousif I E, Ahmed A, Abusofyan S, Ahmed M S. Ramsay Hunt Syndrome: Case Presentation and Management. Adv Dent & Oral Health. 2020; 12(2): 555835. DOI: 10.19080/ADOH.2019.11.555835
Abstract
Introduction: Ramsay hunt syndrome is a Viral infection by VZV which involve the facial nerve (CN VII) mainly although others cranial nerves as (CN VII, IX, V and VI) may be involved, this syndrome presented as: vesiculation and ulceration of the external ear and ipsilateral anterior two third of the tongue and soft palate accompanied by ipsilateral facial palsy, with incidence of 5/ 1000 and most affected people lie within age group of (20-30) years old with no gender prediction.
Case Report: We report a case of a 24 years old male came to our OMFS department at KTDH complained of painful, burning multiple ulcers extra and intra orally restricted to the right side of his face only with prodromal symptoms. Fluid resuscitation, antibiotics and antiviral were given. After ten days the patient developed (lower motor neuron facial palsy) ipsilateral. Diagnosis of RHS was done and corticosteroids were added to his medications.
Conclusion: After revision of many previous studies with different modalities of treatment, we recommend using a combination of antivirals and steroids as the main modality of treatment as it seems plus early diagnosis and treatment are the main factors determine degree and speed of recovery.
Keywords:RHS; VZV; Facial Palsy; Bell’s palsy
Abbreviations: VZV: Varicella Zoster Virus; CN: Cranial Nerve; PCR: Polymerase Chain Reaction; OMFS: Oral and Maxillo Facial Surgery; KTDH: Khartoum Dental Teaching Hospital; RCT: Randomized; Controlled Trial; RHS: Ramsay Hunt Syndrome; HB: House-Brackmann grading System
Definition and Pathophysiology
The American neurologist (James Ramsay Hunt) described three different neurological syndromes and all of them known as Ramsay Hunt Syndrome. The incidence of RHS is 5 /100.000 people and most affected patients are within age group of (20-30) years with no gender prediction [1]. Ramsay hunt syndrome (type 2) is a Viral infection by VZV which involve the facial nerve (CN VII) mainly although others cranial nerves as (CN VII, IX, V and VI) may be involved, this syndrome presented as: vesiculation and ulceration of the external ear and ipsilateral anterior two third of the tongue and soft palate accompanied by ipsilateral facial palsy [2]. VZV infection started as primary infection which known as: varicella or chickenpox. After chickenpox subside and disappear, VZV remain latent in neurons of cranial nerve and dorsal ganglia. Subsequent reactivation of latent VZV can result in localized vesicular rash. Infection or reactivation which involve geniculate ganglion of facial nerve within the temporal bone considered as the main pathophysiological mechanism of ramsay hunt syndrome plus decreased level of VZV-specific cell mediated immunity may cause the reactivation of the virus [3].
Case Report
A 24 years old male patient presented to our OMFS out patient in KTDH complained of painful ,burning multiple ulcers inside his mouth and crusting on skin on the check area of 5 days duration ,started as vesicles then ruptured after three days extending to the ear and restricted only to the right side with swelling on the right infraorbital area accompanied with prodromal symptoms, tinnits and inability to eat with symptoms of hypervolemia and glycaemia .On extra oral examination there was crusted area spread along the distribution of mandibular division of trigeminal nerve on the right side not crossed the midline from angle of the mouth and extended upward and laterally till ear of the same side and continue in the external auditory meatus, with infraorbital oedema on the same side. On intra oral examination there were multiple ulcers distributed over buccal, labial, tongue and floor of the mouth also restricted to the right side and not crossing the midline. On examination of facial nerve, it was intact at the time of first presentation.
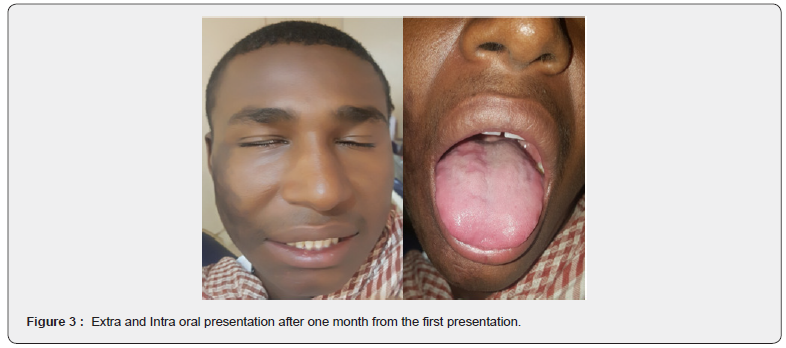
Patient was tachycardic, hypoglycemic with low blood pressure and associated fever, so he was admitted in ward, fluid resuscitation, antibiotics (to eliminate the superimposed infection) and antiviral (acyclovir 800 mg /five times per day) were given. Investigation were requested, they were in normal ranges except there was elevation in C-reactive protein (82.9mg/L). There was improvement started from the second day of first presentation and patient started fluid oral intake .after about 10 days patient develop facial palsy on the ipsilateral side (lower motor neuron) ,definitive diagnosis of Ramsay Hunt syndrome was done ,patient continued on antiviral therapy and referred to ENT hospital and physiotherapy for further management concerning his status and scheduled for regular follow-up and they prescribed prednisolone to him started by 25 mg twice a day for two weeks then reduced to 15 mg twice a day then after another five days till the dose reach 5 mg daily for a while then stopped (Figure 1-3).


Discussion
Literature Review
A retrospective study by Devriese PP et al. [4] on the natural history of facial paralysis in herpes zoster in 102 untreated patients with Ramsay Hunt syndrome; age, extent of paralysis, time, and location of rash were analyzed using a subjective muscle strength scale and response to facial nerve stimulation, the investigators found that maximum loss of function was complete in 1 week. Complete paralysis was two times more frequent comparing to incomplete paralysis and occurred more in patients older than 50 years. Lack of nerve excitability, complete paralysis, and age over 50 were considered as statistically significant factors for poor prognosis of the patients with partial clinical or electrical function at onset, 66% of them recovered completely, whereas only 10% of patients who presented with complete loss of clinical and electrical function recovered completely, while all of them had residual synkinesis. In patients with complete facial paralysis and a partial electrical response, oral synkinesis was developed in 70% while eyelid synkinesis in 60% of patients, whereas in patients with incomplete paralysis both electrically and clinically, oral synkinesis developed in 10% and the eyelid synkinesis in 15% of patients [4].
In Hato et al. [5] did a retrospective review of Ramsay Hunt syndrome in children and adult. The authors evaluated Facial strength using the House-Brackmann grading system. 85 patients were Completely recovered from 173 patients (49%) adults, and in 33 out of 42 patients (78%) younger than 16. Audiograms showed complete recovery in 66% of children with documented hearing loss by audiograms testing compared with 37.7% of adults [5]. A retrospective study in1986 done by Kaiser et about: Ramsay Hunt facial paralysis: clinical analyses of 185 patients .The authors found that 80% of patients presenting with ipsilateral facial palsy were treated orally with 60 mg steroids (prednisone) for 6 days and was decreased by 10 mg daily for the next 5 days. If pain returned or paralysis progressed, prednisone was increased to 60 mg daily for 5 to 7 more days. Use of the objective serial four points tests of nerve excitability to compare patients with Bell’s palsy and patients with Ramsay Hunt syndrome in this study showed that patients with Ramsay Hunt syndrome were statistically more likely to have severe and complete denervation with persistent synkinesis; and prednisone treated patients were less likely to progress to complete facial paralysis than untreated patients [6].
Murakami S et al. [7] did the largest retrospective study in treatment of RHS, which showed a statistically significant improvement in the group treated with prednisone and acyclovir within 3 days of onset. Eighty patients were separated into groups based on the time of treatment starting that is, less than 3 days, 3–7 days, and after 7 days. All patients were treated with oral prednisone (1 mg/kg/day for 5 days followed by a 10-day taper), as well as with intravenous acyclovir (250 mg three times daily), or oral acyclovir (800 mg five times daily). Patients were followed up for 6–12 months with repeated clinical examinations, nerve excitability testing, and audiograms in patients who complained of tinnitus or hearing loss. Complete recovery was seen in 21 (75%) patients treated within the first 3 days (p<0.05), 14 (48%) patients treated at 4-7 days, and seven (30%) when treatment was not started until after 7 days. Further, 26 (50%) patients who were not treated in the first 3 days progressed to a complete loss of response to facial nerve stimulation. No statistically significant divergences were noted among patients treated with intravenous / oral acyclovir. Of 12 patients with mild to moderate hearing loss that were followed up with serial audiograms, six recovered completely, three had partial recovery, and three remained stable. Audio logical outcome did not diver significantly among the treatment groups [7].
Morgan et al. [8] did a study in1992on Facial palsy and infection; the study concluded 9.3% of patients with lower motor neuron facial palsy seroconverted to VZV [8]. In Terada et al. [9] did a study on detection of varicella-zoster virus DNA in peripheral mononuclear cells from patients with Ramsay Hunt syndrome or zoster sine herpete. The authors found that blood mononuclear cells from f4 of 17 patients with Bell’s palsy were positive for VZV DNA which detected by PCR. Resulted in a small proportion of patients with” Bell’s palsy” have RHS [10]. Ramsay Hunt Syndrome is known as a rare and severe complication of varicella zoster virus (VZV) with classic triad to diagnose it consist of otalgia, vesiculation in auditory canal and ipsilateral facial paralysis [10]. Pharmacologic treatment of HZ complicated by RHS is controversial and requires ongoing research. Antivirals and corticosteroids are the current main treatment. Antivirals have been shown to reduce symptomatic duration of acute HZ and long-term nerve damage [11]. While steroids used for their potent anti-inflammatory effect (reducing inflammation and oedema of facial nerve) [12].
In a study conducted by Furuta Y et al. [13] to determine the effect of antiviral agents on recovery from facial palsy in patients with zoster sine herpete (confirmed by PCR ), all 13 patients who received acyclovir-prednisone combined treatment within 7 days of onset recovered completely [13]. A Cochrane Review done by Uscategui T et al. [14] of the sole randomized controlled trial (RCT) comparing treatment with antivirals and corticosteroids to corticosteroids alone in 15 RHS patients showed no significant difference [14]. A meta - analysis by de Ru JA et al. [15] (RHS) articles concluded that antiviral therapy plus steroids compared to steroids alone significantly improved facial nerve function recovery (odds ratio of 2.8, with 95% Confidence Interval (CI)) [15]. The largest RHS treatment study was a retrospective analysis done by Murakami S, Honda N et al. [16] of 80 cases. Patient s treated with acyclovir and prednisone within 72 hours of symptom onset had a complete recovery rate of 75 % versus those who treated after 7 days, who had a complete recovery rate of 30 % [16].
In 2016 a literature review done by Rafael da Costa Monsanto et al. [17] on treatment and prognosis of facial palsy on Ramsay Hunt syndrome considering the different treatments proposed in the literature, the authors read the abstract of 78 studies; 31 studies selected and read and 19 studies were selected for appraisal. Among the 882 selected patients, 621 (70.4%) achieved a House-Brackmann score of I or II; 68% of the patients treated only with steroids achieved HB I or II, versus 70.5% when treated with steroids plus antiviral agents. Among patients with complete facial palsy (grades V or VI), 51.4% recovered to grades I or II. The rate of complete recovery varied considering the steroid associated with acyclovir: 81.3% for methylprednisolone, 69.2% for prednisone; 61.4% for prednisolone; and 76.3% for hydrocortisone [17]. Eye patches, taping the eye closed, artificial tears and oral analgesics are also used in the management of RHS and minimize its complications [11]. Complications associated with RHS include corneal abrasions and ulcers, if eye lid closure is impaired, secondary infection, post herpetic neuralgia, permanent and permanent ipsilateral hearing loss and tinnitus [11].
Conclusion
After revision of many previous studies with different modalities of treatment, we recommend using a combination of antivirals and steroids as the main modality of treatment as it seems plus early diagnosis and treatment are the main factors determine degree and speed of recovery.
References
- Donati D, De Santi L, Ginanneschi F, Cerase A, Annunziata P (2012) Successful response of non –recovering Ramsay Hunt Syndrome to interavenous high dose methylprednisolone. J Neurol Sci 318(1-2): 160-162.
- Kleinschmidt-De Masters BK, Gilden DH (2001) The expanding spectrum of herpes virus infections of the nervous system. Brain Pathol 11(4): 440-451.
- Haginomori S, Ichihara T, Mori A, Kanazawa A, Kawata R, et al. (2016) Varicella zoster virus –specific cell-mediated immunity in Ramsay Hunt Syndrom. Laryngoscope 126(1): E35-39.
- Devriese PP, Moesker WH (1988) The natural history of facial paralysis in herpes zoster. Clin Otolaryngol 13: 289-298.
- Hato N, Kisaki H, Honda N (2000) Ramsay Hunt syndrome in children. Ann Neurol 48: 254-256.
- Robillard RB, Hilsinger RL, Adour KK (1986) Ramsay Hunt facial paralysis: clinical analyses of 185 patients. Otolaryngol Head Neck Surg 95: 292-297.
- Murakami S, Hato N, Horiuchi J (1997) Treatment of Ramsay Hunt syndrome with acyclovir-prednisone: significance of early diagnosis and treatment. Ann Neurol 41: 353-357.
- Morgan M, Nathwani D (1992) Facial palsy and infection: the unfolding story. Clinical Infectious Diseases 14: 263-271.
- Terada K, Niizuma T, Kawano S (1988) Detection of varicella-zoster virus DNA in peripheral mononuclear cells from patients with Ramsay Hunt syndrome or zoster sine herpete. J Med Virol 56: 359-363.
- Adour KK (1994) Otological complications of herpes zoster. Ann Neurol 35: 62-64.
- Worme (2013) An unexpected case of Ramsay hunt syndrome: Case report and literature review. BMC Research Notes 6: 337.
- Whitley RJ, Weiss H, Gnann JW, Tyring S, Mertz GJ, et al. (1996) Acyclovir with and without prednisone for the treatment of herpes zoster. A randomized, placebo-controlled trial. Ann Intern Med 125(5): 376-383.
- Furuta Y, Ohtani F, Mesuda Y (2000) Early diagnosis of zoster sine herpete and antiviral therapy for the treatment of facial palsy. Neurology 55: 708-710.
- Uscategui T, Dorée C, Chamberlain IJ, Burton MJ (2008) Antiviral therapy for Ramsay hunt syndrome (herpes zoster oticus with facial palsy) in adults. Cochrane Database Syst Rev 2008(4): 1-2.
- De Ru JA, Van Benthem PP (2011) Combination therapy is preferable for patients with Ramsay hunt syndrome. Otol Neurotol 32(5): 852-855.
- Murakami S, Honda N, Mizobuchi M, Nakashiro Y, Hato N, et al. (1998) Rapid diagnosis of varicella zoster virus infection in acute facial palsy. Neurol 51(4): 1202-1205.
- Rafael da Costa Monsanto, Aline Gomes Bittencourt, Natal José Bobato Neto (2016) treatment and prognosis of facial palsy on Ramsay Hunt Syndrome: results based on a review of the Literature. Int Arch Otorhinolaryngol 20(4): 394-400.






























