Knowledge, attitude and practices of Dentists regarding management of patients on warfarin therapy
Israa Khatir Mohammed1* and Yousif Idris Eltohami2
1Department of clinical pharmacy, Faculty of post graduate studies, University of Medical Science and Technology, Khartoum, Sudan
2Department of oral and maxillofacial surgery, Faculty of dentistry, University of khartoum, Sudan
Submission: March 04, 2020; Published: March 18, 2020
*Corresponding author: Yousif Idris Eltohami, department of oral and maxillofacial surgery, faculty of dentistry, University of Khartoum, Sudan
How to cite this article: Israa Khatir Mohammed Knowledge, attitude and practices of Dentists about management of patients on warfarin therapy. Adv Dent & Oral Health. 2020; 12(3): 555834. DOI:10.19080/ADOH.2019.11.555834
Abstracts
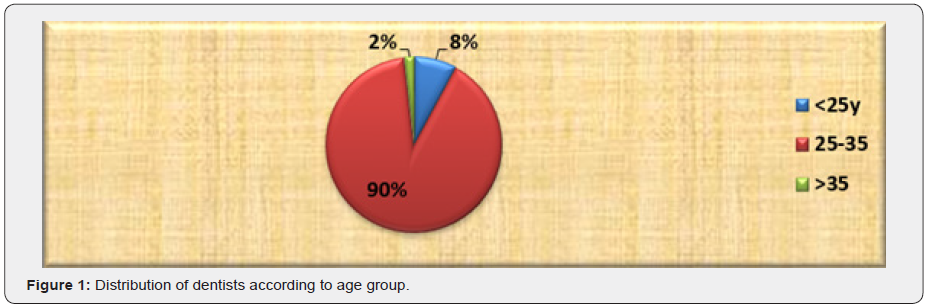
The aim of this study was to assess the knowledge, attitude and practices of dentists about management of patients on warfarin therapy in khartoum, Sudan. A cross sectional study was performed on 113 dentists selected randomly in Khartoum state between November 2017 and February 2018. In this study majority of dentists (90%) were within the age group (25-35y). (71%) were female, (61.1%) were bachelor’s degree holders, (61%) had less than 5 years of experiences. (60%) were coming across patients under warfarin. Regarding the knowledge questions (73.5%) of them knew that the patient taking warfarin should not undergo surgical procedure in primary care clinic even if the INR within the acceptable range. Regarding the practices question (41.6%) of dentists used infiltration or intrafilamentary type of Local anesthesia to patient under warfarin. (50.4%) of them recommended Paracetamol for pain control. The study concluded that most of the dentists (56.6%) had good knowledge and (48.7%) had inadequate practices toward management of patients taking warfarin.
Keywords: Warfarin; Dentists knowledge about warfarin; anticoagulants; INR
Introduction
Warfarin which acts by antagonizing the effect of vitamin k, is one of the most commonly used oral anticoagulants to prevent thromboembolic episodes. Its effect is measured by INR (international normalized ratio) which is a measure of patient prothrombin time divided by the laboratory control value of prothrombin time [1]. A normal coagulation profile has an INR of 1.0. The desirable INR range for patients depends on the condition being treated. Oral anticoagulants are usually prescribed for patients with previous thromboembolic events e.g., stroke, myocardial infarction, pulmonary embolism, atrial fibrillation, prosthetic heart valves and peripheral vascular disease. The clinical management of these patients is generally complex because they are usually older, have multiple comorbid conditions and are taking multiple medications. A range of strategies has been used to manage patient undergoing warfarin treatment before surgical procedure, these include stopping warfarin 2-3 days before surgical procedure, reducing warfarin dose, continuing warfarin, and measuring INR and replace warfarin with low molecular weight heparin [2,3]. Many reports stated that patient requiring minor dental proce dure and having an INR for up to 4.0 are able to continue warfarin without any dose adjustment [4,5]. Withdrawal of warfarin treatment may be responsible for the development of cerebrovascular accident CVA in patient undergoing dental extraction [6].
Dental procedure with higher risk for post-operative bleeding complication includes complex extraction, adjacent extraction that will cause large wound and extraction of more than 3 teeth at once, flap raising procedure gingival recontouring and biopsies [7]. Certain medical condition are known to be associated with an increased bleeding risk due to effects on their coagulations or platelet functions and should be taken into consideration when planning dental treatment, these include liver, kidney bone marrow disorder, recent or current chemotherapy, advanced heart failure and inherited bleeding disorder [7]. Dental practitioners should have the necessary equipment and skills to perform appropriate local haemostatic measures, these include packing any open socket with haemostatic material and placing sutures to stabilize the clot [8]. Some guidelines recommend the use of tranexamic acid mouthwash as an additional haemostatic measure [7]. General dental practitioners (GDPs) should follow published guidelines, particularly for single, straight forward extractions. Many. For most patients undergoing simple single dental extractions, the morbidity of potential thromboembolic events if anticoagulant therapy is discontinued clearly outweighs the risk of prolonged bleeding [9]. A large number of patients seeking dental treatment in Sudan are on long term oral antithrombotic medication. Hence, the purpose of this study was to assess the knowledge, attitude and practices of dentists in Khartoum, Sudan towards the management of patients on warfarin therapy using questionnaire.
Materials and Methods
A total of 113 dentists with different qualification participate in the study in a period from November 2017 to February 2018 in Khartoum state, Sudan. The study was Non interventional – descriptive cross sectional, data was collected using questionnaire which include questions to assess Knowledge, attitude and practices of dentists towards management of patient taking warfarin. Also, Survey responses were further described according to pre-defined demographic parameters such as age gender, qualifications and experiences. Approval was taken from the ethics committee of the graduate college of UMST faculty of pharmacy, also verbal consent had been taken from all participants. Data analysis were performed using Chi-square test to test significant differences between variables. The data was analyzed using Statistical Package for Social Sciences (SPSS version 24) and Microsoft office excel program. P-value ≤ 0.05 was considered significant. All data was expressed as text, illustrated tables and figures. The dentist’s knowledge part was designed to assess dentist’s knowledge score by giving each correct response, assigned score 1 and wrong response 0 (zero), the maximum attainable score was 11 and minimum was 0(zero). The dentists practice part was designed to evaluate dentists practice score by giving each correct response, assigned score 1 and wrong response 0(zero). The maximum attainable score was 8 and minimum was 0 (zero).
Results
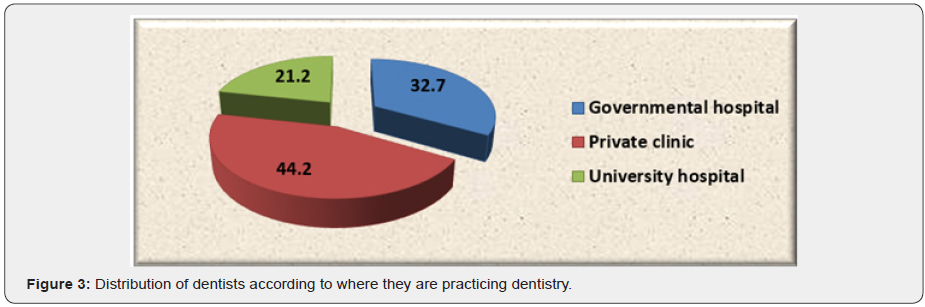
The study included 113 dentists, majority of them (90%) were within the age group (25-35y) (Figure 1). Most of dentists (71 %) were female and 29% were male, (61.1%) were bachelor’s degree holders, (38%) were master holders (Figure 2). (61.1%) of dentists had less than 5 years of experiences, (44.2%) were practicing dentistry in private clinic (Figure 3), (60 %) were coming across patient under warfarin in dental practices. Regarding the knowledge questions as shown in Table 1; majority of dentists (86.7%) knew the main indications of warfarin. only (19.5 %) of dentists answered correctly acceptable INR value that the dental treatment will be carried out safety. 73.5% of dentists knew the medical conditions which should not undergo surgical procedure in primary care clinic.

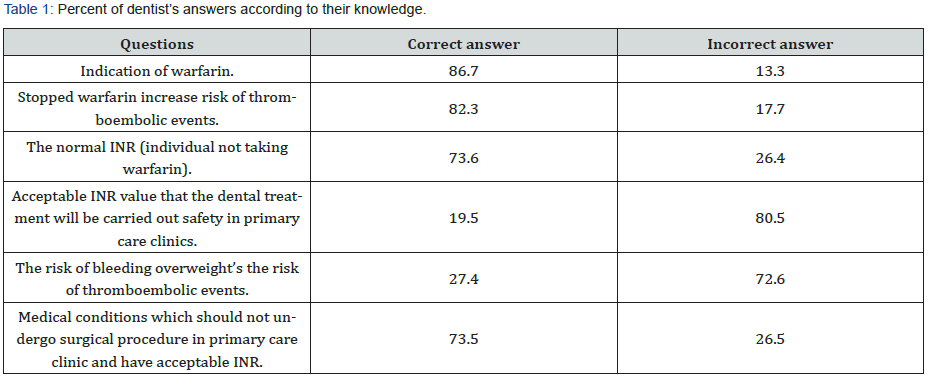
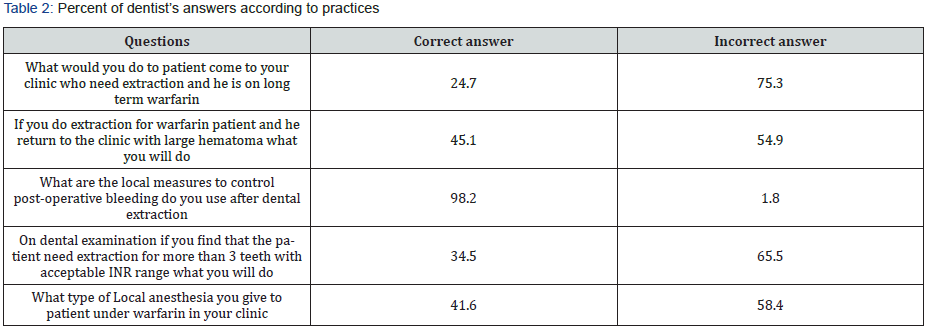
As shown in Figure 4 only 18.6% of dentists knew the dose of Paracetamol (2g /day) above which the INR and the risk of bleeding is increased and only 16.8% of them knew the 2nd line analgesic Dihydrocodeine when Paracetamol is not suitable. Regarding the antibiotics there were 24.8% of dentists knew that prescribing antibiotics while on warfarin significantly increases the chance of developing an INR above 7.0, and 16% of them knew the antibiotics with high risk of developing serious bleeding (quinolones and metronidazole) when co administer with warfarin. Regarding the attitude questions, majority of dentists showed the importance of dental procedure when it was in the beginning of the day and early in the week (Figure 5). In the practices question 41.6% of dentists used infiltration or intrafilamentary type of Local anesthesia to patients under warfarin. Only 34.5% of dentists don’t extracted more than three teeth in one visit if the patient with acceptable INR range, 98.2% of them had correct practices toward local heamostatic measures, 45.1% of them treat correctly the patients who return with large hematoma after extraction. Table 2 50.4%) of dentists recommended Paracetamol for pain control (Figure 6).
Knowledge and practice score
Most of dentists (56.6%) had good knowledge score and 40.7% mal the adequate knowledge (Figure 7). (48.7%) of dentists had inadequate practices and 45.1 % had good practices (Figure 8).
Associations between knowledge and practices
Chi –square correlation test was made between knowledge and practices. The result showed that depending on p-value (Pvalue <0.05) there were highly significant associations between knowledge and practices (Table 3). Chi –square correlation test was made between knowledge and practices with demographic data. The result showed that depending on p-value (P- value <0.05) there were no significant associations between knowledge and practices with demographic data (Table 4).
Discussion
Patients taking Vitamin-K inhibitors had a significantly higher risk of a postoperative bleeding compared to patients without any anticoagulation therapy [10]. A relative study found that 15.4% practitioners were favor of continuing the medication without alteration while 6.6% were unsure about stopping or continuing the medication [11]. In this study majority of dentists thinking that beginning of the day and early in the week of the dental procedure was important, also thinking that the primary care dentist ever advise an alteration to warfarin regimen. Oral anticoagulants are usually prescribed for patients with previous thromboembolic events. The clinical management of these patients is generally complex. The respondent has limited knowledge about diseases that require use of OAM and selection of screening test of Oral antithrombotic medications. In this study regarding the knowledge questions when participated dentists were asked about indications of warfarin, there were 86.7% of them had correct answer.
Many reports stated that patient requiring minor dental procedure and having an INR for up to 4.0 are able to continue warfarin without any dose adjustment [4,5]. In this study only (19.5%) of dentists know the acceptable INR through which treatment can be carried out safety. A range of strategies has been used to manage patient undergoing warfarin treatment before surgical procedure, these include stopping warfarin 2-3 days before surgical procedure, reducing warfarin dose, continuing warfarin, and measuring INR and replace warfarin with low molecular weight heparin [2,3]. In this study (73.5%) of dentists knew that the patient taking warfarin should not undergo surgical procedure in primary care clinic even if the INR within the acceptable range. A different study made by Gaspar et al. [12] about the tranexamic acid mouthwash, the results indicated that a combination of local antifibrinolytic therapy and a local hemostatic agent is effective in preventing postoperative bleeding after oral surgery in patients treated with anticoagulants. Also, recent literatures support newer hemostatic agent e.g. Oral rinse with 4.8% tranexamic acid for better and earlier hemostasis [10].
In this study (57.5%) of dentists were knew the Tranexamic acid 5% mouthwash that is used specifically for people taking anticoagulant therapy to prevent bleeding after dental surgery. A meta-analysis by Hughes G et al. [13] found that small prospective studies of various designs and case studies describe aberrant INR results in patients using acetaminophen while receiving warfarin. These INR elevations typically involved acetaminophen ingestion of at least 2 g/day for several consecutive days. In this study 18.6% of dentists were knew the dose of Paracetamol that can raise the INR and increase the risk of bleeding, 16.8% of them knew Dihydrocodeine which was the 2nd line analgesic when Paracetamol is not suitable, (64.6%) of them didn’t prescribe NSAID to control the pain. Study made by Michael in 2014 about serious bleeding events due to warfarin and antibiotics co – prescription. Antibiotics prescriptions lasting less than 3 days were excluded. Antibiotics which are known to interact in a way which may increase bleeding risk were considered “high-risk.” High-risk antibiotics included trimethoprim/sulfamethoxazole (TMP/SMX), ciprofloxacin, levofloxacin, metronidazole, fluconazole, azithromycin and clarithromycin. Low-risk antibiotics included clindamycin and cephalexin. Receipt of a high-risk antibiotic and azithromycin were associated with increased risk of bleeding as a primary diagnosis. TMP/SMX, ciprofloxacin, levofloxacin, azithromycin and clarithromycin were associated with serious bleeding as a primary or secondary diagnosis. INR alterations were common; 9.7% of patients prescribed fluconazole had INR value >6. Patients who had INR performed 3-14 days of co-prescription were at a decrease risk of serious bleeding [14].
In this study 22% of dentists didn’t routinely prescribe antibiotics after dental procedure for patient under warfarin, (16%) of them knew quinolones and metronidazole which are Antibiotics with high risk of developing serious bleeding when co administer with warfarin. Local anesthesia should be delivered using aspirating syringe and contain vasoconstrictor unless contraindicated [7]. In this study 41.6% of dentists used infiltration or intrafila mentary type of Local anesthesia for patient under warfarin. Dental procedure with higher risk for post-operative bleeding complications include complex extraction, adjacent extraction that will cause large wound and extraction of more than 3 teeth at once, flap raising procedure gingival recontouring and biopsies [7]. (34.5%) of dentists in this study extracted no more than three teeth in one visit if the patient with acceptable INR. The arrest of bleeding is a core skill for primary dental care and the dental practitioners should have the necessary equipment and skills to perform appropriate local hemostatic measures. These include packing any open socket with hemostatic material and placing sutures to stabilize the clot [8] in this study 45.1% of dentists made evacuation of clot, packing and closure to warfarin patient who return to the clinic with large hematoma after extraction. A prospective study found that extractions in patients on oral anticoagulants must be performed in the least traumatic manner possible. It is not necessary to stop anticoagulant therapy to perform extractions. Local hemostasis techniques, such as obliterative sutures alone are sufficient to prevent hemorrhagic complications15. In this study 98.2% of dentists had correct practices toward local measures to control post-operative bleeding [15].
Conclusion
The current study revealed most of dentists (56.6%) had good knowledge score and (40.7%) mal the adequate knowledge. Also (48.7%) of dentists had inadequate practices.
References
- Salam S, Yusuf H, Milosevic A (2007) Bleeding after oral extraction in patient taking warfarin. Br J Oral maxillofac Surg 45(6): 463-466.
- Jaffer AK, Brotman DJ, Chukwumeriji N (2003) When patient on warfarin need surgery. Cleve clin J Med 70(11): 973-984.
- Hong C, Napenas JJ, Brennan M, Furney S, Lockhart P (2012) Risk of post-operative bleeding after dental procedure in patient on warfarin: aretrospective study. Oral Surg Oral Med Oral pathol Oral Radiol 114(4): 464-468.
- Nematullah A, Alabousi A, Blanas N, Douketis JD, Sutherland SE (2009) Dental surgery for patient on anticoagulant therapy with warfarin: a systematic review and meta-analysis. Tex Dent J 126: 1183-1193.
- Randall C (2005) Surgical management of the primary care dental patient on warfarin. Dent Update 32(7): 414-420.
- Stiefelhagen P (2009) Stroke after tooth extraction. MMW Fortschr Med 151(25): 17.
- (2015) Scottish dental clinical effectiveness programme SDCEP, Anticoagulants – guidance. Management of dental patient taking anticoagulants or antiplatelet drugs.
- McCormick NJ, Moore UJ, Meechan JG (2014) Haemostasis Part 1; The management of post extraction haemorrhage. Dent Update 41(4): 290-292.
- Campbell JH, Alvarado F, Murray RA (2000) Anticoagulation and Minor Oral Surgery: Should the Anticoagulation Regimen Be Altered? J Oral Maxillofac Surg 58(2): 131-135.
- Clemm R, Neukam FW, Rusche B, Bauersachs A, Musazada S, et al. (2016) Management of anticoagulated patients in implant therapy. A clinical comparative study. Clin Oral Impl Res 27(10): 1274-1282.
- Altaf H, Hesham S, Faleh A, Soban G, Nasser R, et al. (2015) Knowledge of medical and dental practitioners towards dental managements of patients on anticoagulants and / or antiplatelets therapy. The Saudi journal for dental research 6(2): 91-97.
- Gaspar Rone, Brenner Beni, Leon Ardekian, Peled Micha, Laufer Dov (1997) Quintessence International 28(6): 375-379.
- Hughes GJ, Patel PN, Saxena N (2011) Effect of acetaminophen on international normalized ratio in patients receiving warfarin therapy. Pharmacotherapy 31(6): 591-597.
- Lane Michael A, Angelique Zeringue, Jay R, McDonald (2014) Serious Bleeding Events due to Warfarin and Antibiotic Co-Prescription in a Cohort of Veterans. The American journal of medicine 127(7): 657-663.
- Pereira, Claudio Maranhão, et al. (2011) Tooth Extraction in Patients on Oral Anticoagulants: Prospective Study Conducted in 108 Brazilian Patients. ISRN Dentistry 2011: 203619.






























