Association between Steroid Anti-Inflammatory Drugs and Oral-Dental State- A Literature Review
Tsvetelina Borisova*
Medical University-Varna, Bulgaria
Submission: May 17, 2019; Published: June 11, 2019
*Corresponding author: Tsvetelina Borisova, Faculty of Dental Medicine, Medical University-Varna, Bulgaria
How to cite this article: Tsvetelina Borisova. Association between Steroid Anti-Inflammatory Drugs and Oral-Dental State- A Literature Review. Adv Dent & Oral Health. 2019; 11(1): 555801. DOI: 10.19080/ADOH.2019.11.555801
Abstract
It has been established that people accepting oral corticosteroids often suffer from lack of teeth or are characterized with caries-non-resistant dentition. Corticosteroids can affect the consistency of alveolar bone, causing its osteoporotic alteration related to reduction of osteoblasts and amount of osteoid matrix. Parallel to the application of corticosteroids, there is a tendency of decrease of the height of alveolar bone and fibrous transformation of the periodontal space. There can be established severe loss of supporting alveolar bone. Corticosteroids therapy interrelates to enhanced potential for clinical manifestation of alterations of taste sensation, periodontitis, gingivitis, ulceration, candidiasis, tooth decay, xerostomia. Authors have established that the prolonged use of corticosteroids is in direct ratio to elevated rate of incidence and progression of inflammatory disorders of the supporting periodontal apparatus. The pathophysiological mechanisms of disturbance of the function of local and systemic immunity, provoked and sustained by corticosteroids’ therapy, lead to considerable increase of the distribution of periodontal disorders.
Keywords: Steroid anti-inflammatory drugs; Oral health; Risk; Tooth decay; Periodontal disease; Oral mucosa alterations
Introduction
Steroidal anti-inflammatory drugs are characterized with definite anti-allergic, immune-suppressive and anti-inflammatory effects [1]. In parallel to their positive action, corticosteroids have the potential to cause bruising, cataracts, muscle weakness, gastro-intestinal disorder of hyperacidity, oral candidiasis [2]. It has been established that patients accepting oral corticosteroids often suffer from lack of teeth or are characterized with caries-non-resistant dentition [3,4]. Corticosteroids can affect the consistency of alveolar bone, causing its osteoporotic alteration related to reduction of osteoblasts and amount of osteoid matrix. As a result, there is decrease of the height of alveolar bone and fibrous transformation of the periodontal space [5]. Therefore, there can be established severe loss of supporting alveolar bone.
Researchers have reported conditions of considerable dilatation of blood vessels into the pulp vascular plexus [6,7]. Corticosteroids give impact upon the process of tertiary dentin synthesis and secretion [8]. In histological slides can be observed zones of disturbed odontoblasts in the region of coronal and radicular pulp chamber [9]. In affected teeth there has been recorded approximately four time increase of the size of the pre-dentin layer in comparison to intact teeth. There have been registered histological findings of overproduction of secondary dentin [10]. In other cases, there has been established the pathological substrate of fibrosis along the whole dentin width [11]. Because of persistent constriction of dentin pulp chamber there has been explicitly manifested suppression of blood circulation and disturbed nutrition of dentin-pulp tissue complex. There has been established inhibition of the functional activity of growth factors and deteriorated capability of odontoblasts’ regeneration, resulting in the process of metaplasia, respectively compensatory synthesis and apposition of fibrous tissue [11].
The aim of this study is to analyze the association between steroid anti-inflammatory drugs and oral-dental state in the context of a detailed scientific literature review. Many scientific literature sources have been thoroughly investigated.
Results and Discussion
Profound researches devoted to the effects of prolonged corticosteroids’ therapy ascertained their role for total disturbance of electrolytes’ equilibrium in the organism. Dental pulp is also affected by the adverse effects of these hormones. In 1993 Nasstrom et al. [12] investigated the impingement of corticosteroids upon dentin-pulp tissue complex and accentuated on the effect of considerable reduction of coronal and radicular pulp chamber volume [12]. In 1996 Nasstrom carried out detailed studies on patients going through renal transplantation under the protection of corticosteroids and proved that cells responsible for the synthesis and release of dentin, namely odontoblasts, have been under these medicines’ impact for the initial phase of treatment. After a period of several years of regular intake of corticosteroids there has been recorded the pathological alteration of calcification of pulp.
Steroids-related calcification of dental pulp tissue can be associated with interference with enzymatic metabolism, resulting in affliction upon the proper process of histological, morphological and physiological differentiation of the tooth structural constituents [9].
Other authors established that pulp calcification occurs because of necrosis of the outer pulp layer without disturbance of normal production of dentin in condition of prolonged application of corticosteroids [13]. The initiation of new dentin layers formation is related to fluctuations of steroid hormones and modified functional activities of mature odontoblasts [8]. These cells of the periphery topographic zone of the pulp tissue complex are characterized with specific sample of reaction to the dynamic variations of steroid hormones, not afflicting regular deposition of dentin [14].
On the other hand, some authors represent the statement that during pre-functional eruptive phase and early functional eruptive phase of teeth can be recorded decrease of the rate of synthesis and release of dentin [15]. Other researchers accentuate on the role of corticosteroids for stimulation of apposition of abundant pre-dentin tissue, with parallel and subsequently organized and performed process of accomplishment of predentin mineralization [12,16]. Simultaneously, according to some literature sources, in terms of electron probe X-ray microanalytical investigation of dentin minerals in participants going through steroids therapy, there has been established enlarged irregularly mineralized pre-dentin area [17].
In the scope of periodontology, systemic and topical administration of corticosteroids have been prescribed for patients suffering from dermatologic diseases, such as systemic lupus erythematosus, erythema exudativum multiforme, pemphigus, characterized with definite manifestation upon periodontal and gingival tissues [18].
Implementation of corticosteroids locally in the region of inflamed marginal gingiva leads to suppression of the rate of bleeding and inhibition of the inflammatory reaction [19]. In cases of topical administration of steroid anti-inflammatory drugs, injected into gingival tissue, there has been established the effect of disturbance of the permeability of capillaries and production of collagen, reduction in plasma cells and granulation tissue [19-21].
Some investigations have been devoted to concentrationrelated effect of corticosteroids. Researchers ascertained that high dosage of hydrocortisone is related to enhancement of the rate of bio-indicators of matrix metallo-proteinases, namely MMP1, MMP2, MMP7 and MMP11. Simultaneously, low level of hydrocortisone is associated to decrease of their expression [22].
In people with the diagnosis of asthma that is controlled by the means of long-term inhalational steroid therapy there has been observed loss of teeth in condition of periodontal disease [23,24]. More vulnerable to pathological mobility and loss occurred to be mandibular teeth, probably related to fractions of drug remaining in oral cavity [25]. So, patients undergoing inhalational corticosteroids treatment are more susceptible to periodontal disorder affecting lower jaw, especially in the presence of risk factors for osteoporosis [26,27].
In young adults with prescribed and applied long-term steroid anti-inflammatory drugs there has been outlined a tendency of suppressed secretion of saliva, accompanied by elevated risk of gingivitis and tooth decay. Namely people using inhalational corticosteroids are characterized with higher incidence of severe forms of gingival inflammation. Mouth breathing and application of corticosteroids-containing inhalers are associated to considerable fluctuations of the level of salivary pH, depression of the release of saliva, enhanced risk of dental plaque accumulation, initiation and progression of carious lesions [28,29].
Other authors, Safkan et al. [30], confirmed that patients in condition of steroid anti-inflammatory drugs’ therapy are explicitly predisposed to gingivitis. On the other side, participants in the control group were with clinical findings of lower rate of dental calculus deposition and less alveolar bone loss. It has been registered that duration of corticosteroids’ application for one year or more is related to greater degree of manifestation of clinical symptoms of periodontitis.
Markitziu et al. [31] performed a research of patients with established diagnosis of pemphigus vulgaris undergoing corticosteroids’ treatment protocol. The periodontal state of the participants was not characterized with statistically significant difference concerning the indicator of alveolar bone height compared to the control group. There has been revealed a reduction in the rate of cortisol in saliva, in relation to decrease in hypothalamic-pituitary-adrenal axis activity. Both groups into the study have shown statistically significant differences regarding clinical variables of bleeding and gingival recession. Essential to accentuate on the fact that, in difference from Safkan et al. [30], Markitziu et al. [31] have assessed results before and after performance of target periodontal therapy, with inclusion of basic items of scaling, root planning and instructions for oral hygiene level improvement and optimization.
Von Wowern et al. [32] carried out a research devoted to analysis of gingival tissue and bone level of the marginal periodontium in subjects with diagnosed acute nephritis, in relation to mineral bone content of the forearm and jaw, measured by scanner. Participants were divided into two groups regarding application of prednisone and deflazacort, respectively. Nevertheless, both groups were marked by considerable mineral bone loss during the study, no statistically significant differences were recorded between participants of both groups concerning the indicator of bone mineral content loss in forearm and jaw after periods of 6 and 12 months. There were no statistically significant differences between groups on the base of the periodontal variables of clinical attachment loss, gingival index, visible plaque index.
Besides their definite strong anti-inflammatory and immunosuppressive effects, corticosteroids can impinge upon the normal physiological and functional traits of oral cavity structures. The prolonged application of these medicines can lead to severe deterioration of oral-dental health. Affliction of hard teeth structures, soft tissues and alveolar bone by misuse of steroid anti-inflammatory drugs must be taken into consideration. There have been performed studies accentuating on evaluation of the impact of corticosteroids simultaneously upon radiological visualized alterations in jaw bones and oral health status [33].
An investigation included a total number of 100 participants undergoing long-lasting corticosteroids’ therapy with duration of minimum 3 months and a control group of 100 healthy people. The routine clinical examination was combined with X-Ray image diagnostics of bone tissue by the means of intraoral periapical radiograph and digital orthopantomograph. Researchers evaluated levels of the para-clinical indicators of serum calcium, alkaline phosphatase and glucose. For the purpose of statistical analysis were implemented Mann-Whitney U test, Kolmogorov- Smirnov test, Chi-square test. The level of statistically based significance has been assumed for the value of P > 0.05 [33]. In the context of the study was established that people under steroids anti-inflammatory therapy were in greater degree predisposed to candidiasis and manifestation of considerable clinical findings of probing pocket depth and clinical attachment loss. The parameter of bone density was significantly higher in the control group in comparison to the study group. The last was characterized with statistically significant lower rates of calcium, respectively statistically higher rates of blood glucose. Authors concluded that prolonged application of corticosteroids is related to explicit impingement upon bone metabolism, accompanied with considerable reduction of mandibular bone mineral density [33].
Inhaled corticosteroids, sodium cromoglycate, anticholinergic bronchodilators, β-2 agonists are frequently administered alone or in combination in form of inhalation therapy for the treatment of asthma and chronic obstructive pulmonary disease [34].
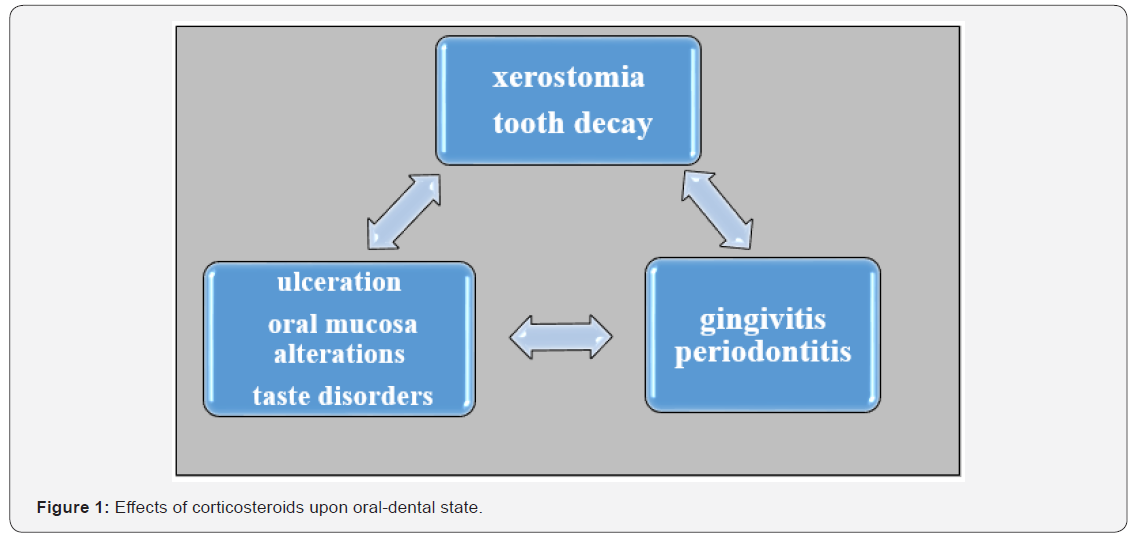
The dosage, duration and frequency of application of steroid anti-inflammatory drugs correlate to the severity of adverse effect upon oral-dental status. Corticosteroids’ therapy interrelates to enhanced potential for clinical manifestation of alterations of taste sensation, periodontitis, gingivitis, ulceration, candidiasis, tooth decay, xerostomia (Figure 1).
Considering the definite tendency of increase of chronic respiratory disorders distribution, researchers accentuate on the inevitable necessity of performance of optimized oral health cares for the purpose of prophylaxis and efficient management of the risk of oral cavity diseases [34].
Xerostomia is a pathological state of definite suppression of salivary flow and is indicated among the adverse effects of administration of beta-2 agonists, [35] anticholinergic inhalers, [36] and inhaled corticosteroids [37]. Complaints of people suffering from xerostomia are related to improper retention of dentures, burning sensation, mouth soreness, manifested discomfort into oral cavity, taste alterations, handicaps in talking and/or swallowing. There can be observed clinical findings of epithelial atrophy, ulceration, oral fissuring. Oral mucosa can be affected by generalized erythema. The dorsal surface of the tongue can be characterized with the pathological trait of lobulated appearance [38].
The application of inhalation corticosteroids’ therapy is often characterized with the combined adverse effects of xerostomia and immunosuppression. Blockage of the protective mechanisms of local immunity in the medium of impingement of the homeostasis into oral cavity leads to pathological alterations of sub-epithelial penetrating lesions of ulcers. These are lesions surrounded by erythematous halo and covered by yellowish fibrinous membrane. Ulcers occur and aggravate upon the movable oral mucosa [39,40].
In condition of administration of inhaled steroid antiinflammatory drugs, the deteriorative consequence of xerostomia can be accompanied by bad breath, respectively halitosis [41].
Corticosteroids’ therapy related state of xerostomia can be in interrelation to disturbance of taste sensation due to suppressed transport of tastant molecules to the taste buds and improper food solubilization [42].
Tooth decay is a behavioral disease with infectious nature characterized with destruction of the hard teeth tissues [43]. Saliva is an essential constituent of the fluid medium of oral cavity. Oversaturated with phosphate and calcium ions, especially in combination with fluoride compounds, in conditions of proper fluoride prophylaxis, saliva is characterized with definite protective properties and potentials for re-mineralization of enamel [44].
Metabolic activities of disintegration of fermentable carbohydrates by cariogenic microorganisms lead to considerable reduction of the rate of pH to the so-called critical value of 5,5 or lower. As a result, there is provoked the process of irreversible demineralization of enamel [45]. Salivary constituents of calcium, phosphates and fluorides serve as essential factors for the performance of the opposed process of re-mineralization at the stage of caries incipience [46].
The renal disorder of nephrotic syndrome is characterized with high rate of recurrences, with no predisposition to progressive functional impingement of the excretory system. As etiological factors are concerned allergic reactions, burn lesions, intoxications, immunization procedures. In these conditions are administered immune-suppressive medicines because of their definite potential for restorative effects. On the other side, steroid anti-inflammatory drugs suppress the proper immune reactions on systemic level and locally into the oral cavity. A para-clinical parameter of explicit significance is the elevation of proteinconnected calcium at the expense of decreased value of the serum one [47,48].
Accumulation of dental plaque is in direct ratio to decrease of the rate of salivation. The disturbed buffer capacity of saliva and persistent low values of pH serve as favorable conditions for growth of acids-producing and acidophilic cariogenic microorganisms of Streptococcus mutans and Streptococcus sobrinus. The disturbed equilibrium between protective and predisposing factors for caries, namely between incessant sugar intakes, cariogenic microflora, quality and quantity traits of enamel, dental plaque, saliva, endogenous and exogenous fluoride products, remineralizing therapy, with prevailing activity of the predisposing ones, correlates to increased intensity and distribution of caries.
The disturbance of somatic health, with a wide spectrum of clinical manifestations, can result in limitation of activities for restoration and optimization of oral health in functional, prophylactic and esthetic aspect [49-51].
The disturbance of somatic health, with a wide spectrum of clinical manifestations, can result in limitation of activities for restoration and optimization of oral health in functional, prophylactic and esthetic aspect [49-51].
A great variety of indicators, namely topographic location of decay lesions, deepness of advancing carious process, oralhygiene status, traits of nutrition, age of children, are associated to the severity of caries clinical findings and their reflection upon oral health. It has been ascertained that more vulnerable to aggressively proceeding destruction of hard teeth tissues are small children, these deprived of regular prophylactic procedures, as well as children with systemic diseases, respectively nephrotic syndrome [56]. In these conditions the lack of adequate therapeutic dental cares provokes definite pain discomfort, negative effects on physical well-being, psychological and emotional state, behavior, social activities [57,58].
Profound scientific investigations ascertain that children with mixed or permanent dentition undergoing corticosteroids’ inhalation therapy are evaluated to be in higher risk for caries compared to healthy children [59,60]. The initial carious lesions determined as white spots of de-mineralization, as well as the progressed cavity lesions, are clinically manifested on the vestibular surfaces of frontal teeth and the occlusal surfaces of distal teeth [61,62].
Oral mucosa alterations- Inhaled corticosteroids’ therapy, particularly the prolonged misusage of such medicines, is associated to high level of risk of oropharyngeal candidiasis [61]. Most frequently manifested form of oral cavity affecting candidiasis is the pseudomembranous one. It is characterized with the clinical findings of white colored, soft in consistency plaques. The most vulnerable areas are lateral surfaces of the tongue, oropharynx, buccal mucosa. Underneath the plaques, when mechanically removed, occurs ulcerated or eroded erythematous layer, associated to the definite symptom of pain. The disintegration of the pseudomembranous lesions is accompanied with complaints of burning and dysphagia. The implementation of inhaled steroid anti-inflammatory drugs can lead to adverse effects such as cough, dysphonia, irritation of throat, dryness of oral cavity, pathological enlargement of the tongue [63,64].
Authors have established that the prolonged use of inhaled corticosteroids is in direct ratio to enhanced rate of incidence and progression of gingivitis [65]. The harmful habit of mouth breathing in these patients contributes to aggravation of the state of gingival inflammation in condition of dehydration of alveolar mucosa. The pathophysiological mechanisms of disturbance of the function of local and systemic immunity, provoked and sustained by corticosteroids’ therapy, including inhaled drugs, are related to considerable increase of the distribution of periodontal disorders [66].
In the context of another study it has been ascertained that the common health status of the individual, respectively the application of steroid anti-inflammatory drugs in children with diagnosed nephrotic syndrome, is related to establishment of statistically significant effects on different factors for caries such as pH, number of carious lesions, PLI, GI [67].
Taking into consideration the fact that saliva serves as an essential factor for protection against gingival and periodontal diseases, therefore medicines with impact upon quality and quantity characteristics of saliva exercise influence on the severity of periodontal noxae [68].
Conclusion
To summarize, based on a profound scientific literature review there has been ascertained definite association between steroid anti-inflammatory drugs and oral-dental state.
References
- Ashwini P, Meena N, Santosh R, Anjali K, Ashish S, et al. (2010) Effect of Long-term Corticosteroids on Dental Pulp. World Journal of Dentistry 1(1): 17-20.
- Walsh LJ, Wong CA, Oborne J, Cooper S, Lewis SA, et al. (2001) Adverse effects of oral corticosteroids in relation to dose in patients with lung disease. Thorax 56(4): 279-284.
- Kässer UR, Gleissner C, Dehne F, Michel A, Willershausen-Zönnchen B, et al. (1997) Risk for periodontal disease in patients with longstanding rheumatoid arthritis. Arthritis Rheum 40(12): 2248-2251.
- Kankaala TM, Virtanen JI, Larmas MA (1998) Timing of first fillings in the primary dentition and permanent first molars of asthmatic children. Acta Odontologica Scand 56(1): 20-24.
- Glickmann I, Stone IC, Chawla TN (1951) Effect of cortisone acetate on the periodontal tissues of white mice. J Dent Res 30:461.
- Applebaum E, Seelig A (1955) Histologic changes in jaws and teeth of rats following nephritis, adrenelectomy and cortisone treatment. Oral Surg Oral Med and Oral Path 8: 881-891.
- Goldsmith EP, Ross TA (1956) Histochemical and histological study of the effects of cortisone on the lower incisors of fetal and post-natal rats. Acta Endocrine 22(1): 23-25.
- Nasstrom K, Petersson A, Konard P (1989) Effect of intravenous administration of corticosteroids on dentine formation in adult rat molar. Scand J Dent Res 97(4): 301-306.
- Anneroth G, Bloom G (1966) Structural changes in the incisors of cortisone treated rats. J Denr Res 45(2): 229-335.
- Nasstrom K, Forsberg B, Petersson A, Westesson PL (1985) Narrowing of the dental pulp chamber in patients with renal diseases. Oral Surg 59(3): 242-246.
- Yoshiho C, Tateo D, Makoto M, Yasushi M, Mitsuko M, et al. (2007) Dental pulp changes observed in patient on long-term corticosteroids. Journal of Hard tissue biology 16(1): 31-35.
- Näsström K, Möller B, Petersson A (1993) Effect on human teeth of renal transplantation: A postmortem study. Scan J Dent Res 101(4): 202-209.
- Obersztyn A, Jedrzejczyk J, Smiechowska W (1968) Application of Lyophilized dentin chips mixed with prednisolone and neomycin on infected rat incisor pulp. J Dent Res 47(3): 374-380.
- Capik I, Ledecky V, Sevcik A (2003) Effects of Flumetazone on exposed dental pulp of dogs. Acta Vet Brno 72: 279-283.
- Ball PC (1977) Lack of effect of excess gloucocorticoid hormone on the rate of dentin deposition in rats. J Dent Res 56(6): 685-690.
- Wysocki GP, Daley TD, Ulan RA (1983) Predentin changes in patients with chronic renal failure. Oral Surg Oral Med and Oral Pathol 56(2): 167-273.
- Huumonen S, Larmas M (1999) An electron probe X-ray microanalytical study of dentin minerals in sucrose fed or glucocorticoid medicated rats. Calcif Tissue Int 65(3): 223-225.
- Harshita N, Deepa GK, Swati (2018) Corticosteroids- Assets and Liabilities on Periodontium. Asian Journal of Pharmaceutical and Clinical Research 11(8): 56-60.
- Berliner DL, Nabors CJ (1967) Effects of corticosteroids on fibroblast functions. J Reticuloendothel Soc 4(4): 284-313.
- Bauer EA, Kronberger A, Valle KJ, Jeffrey JJ, Eisen AZ (1985) Glucocorticoid modulation of collagenase expression in human skin fibroblast cultures. Evidence for pre-translational inhibition. Biochim Biophys Acta 825(2): 227-235.
- Priestley GC, Brown JC (1980) Effects of corticosteroids on the proliferation of normal and abnormal human connective tissue cells. Br J Dermatol 102: 35-41.
- Cury PR, Araújo VC, Canavez F, Furuse C, Araújo NS (2007) Hydrocortisone affects the expression of matrix metalloproteinases (MMP-1, -2, -3, -7, and -11) and tissue inhibitor of matrix metalloproteinases (TIMP-1) in human gingival fibroblasts. J Periodontol 78: 1309-1315.
- Martin RJ, Szefler SJ, Chinchilli VM, Monica K, Myrna D, et al. (2002) Systemic effect comparisons of six inhaled corticosteroid preparations. Am J Respir Crit Care Med 165: 1377-1383.
- Derendorf H (1997) Pharmacokinetic and pharmacodynamic properties of inhaled corticosteroids in relation to efficacy and safety. Respir Med 91: 22-28.
- Selroos O, Halme M (1991) Effect of a volumatic spacer and mouth rinsing on systemic absorption of inhaled corticosteroids from a metered dose inhaler and dry powder inhaler. Thorax 46(12): 891-894.
- El O, Gulbahar S, Ceylan E (2005) Bone mineral density in asthmatic patients using low dose inhaled glucocorticosteroids. J Investig Allergol Clin Immunol 15(1): 57-62.
- Jones A, Fay JK, Burr M, Stone M, Hood K (2002) Inhaled corticosteroid effects on bone metabolism in asthma and mild chronic obstructive pulmonary disease. Cochrane Database Syst Rev 1: CD003537.
- Boskabady M, Nematollahi H, Boskabady MH (2012) Effect of inhaled medication and inhalation technique on dental caries in asthmatic patients. Iran Red Crescent Med J 14(12): 816-821.
- Daudt DL, Cavagni J, Gaio JE, Souza A, Torres SL, et al. (2011) Effect of inhaled corticosteroid on TNF-α production and alveolar bone loss in Wistar rats. Arch Oral Biol 56: 1398-1403.
- Safkan B, Knuuttila M (1984) Corticosteroid therapy and periodontal disease. J Clin Periodontol 11(8): 515-522.
- Markitziu A, Zafiropoulos G, Flores de Jacoby L, Pisanty S (1990) Periodontal alterations in patients with pemphigus vulgaris taking steroids. A biannual assessment. J Clin Periodontol 17(4): 228-232.
- von Wowern N, Klausen B, Olgaard K (1992) Steroid-induced mandibular bone loss in relation to marginal periodontal changes. J Clin Periodontol 19(3): 182-186.
- Beeraka SS, Natarajan K, Patil R, Manne RK, Prathi VS (2013) Clinical and radiological assessment of effects of long-term corticosteroid therapy on oral health. Dent Res J (Isfahan) 10(5): 666-673.
- Godara N, Godara R, Khullar M (2011) Impact of inhalation therapy on oral health. Lung India 28(4): 272-275.
- Ryberg M, Moller C, Ericson T (1987) Effect of beta-2 adrenoceptor agonists on saliva proteins and dental caries in asthmatic children. J Dent Res 66(8): 1404-1406.
- Casaburi R, Mahler DA, Jones PW, Wanner A, San PG, et al. (2002) A long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary disease. Eur Respir J 19(2): 217-224.
- Torres SR, Peixoto CB, Caldas DM, Silva EB, Akiti T, et al. (2002) Relationship between salivary flow rates and Candida counts in subjects with xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93(2): 149-154.
- Regezi JA, Sciubba JJ, Jordan RC (2008) Salivary Gland Diseases. In: Regezi JA, Sciubba JJ, et al. (Eds.) Oral Pathology, Clinical Pathologic Correlations. (5th edn), St. Louis: Saunders, pp. 191-192.
- Karl LH (2002) Asthma and oral health: A clinical and epidemiological study. Acta Electronica Universitatis Tamperensis. 1-82.
- DeRossi SS, Ciarrocca KN, Alawi F (2010) Oral ulcerations in a patient with severe asthma. J Am Dent Assoc 141(1): 47-51.
- Porter SR, Scully C (2006) Oral malodor (halitosis) BMJ 333(7569): 632-635.
- Hyyppa T, Paunio K (1979) Oral health and salivary factors in children with asthma. Proc Finn Dent Soc 75(1-2): 7-10.
- Roberson TM (2006) Cariology: The lesion, etiology, prevention, and control. In: Roberson TM (Ed.) Sturdevant’s Art and Science of Operative Dentistry. 5th edn. St. Louis: Saunders, pp. 68-69.
- Kidd E (2005) Introduction. In: Kidd E (Ed.) Essentials of Dental Caries. (3rd edn), p. 8.
- Featherstone JD (2004) The continuum of dental caries-evidence for a dynamic disease process. J Dent Res 83: C39-C42.
- Featherstone JD (1999) Prevention and reversal of dental caries: role of low-level fluoride. Community Dent Oral Epidemiol 27(1): 31-40.
- Bliznakova D (2010) Pediatrics for Dentists. Varna, pp. 227-272.
- Angelova S (2018) Clinical Manifestation of Caries in Association with Salivary Markers in Children with Nephrotic Syndrome. Humanities - Past, Nowadays and Future. The 6th Human and Social Sciences at the Common Conference, pp. 54-58.
- Eddy AA (2003) Symons JM Nephrotyic syndrome in childhood. Lancet 362(9384): 629-639.
- Meyrier A, Radhakrishnan J (2018) Acute kidney injury (AKI) in minimal change disease and other forms of nephrotic syndrome.
- Moosani A (2012) Evaluation of Oral Neutrophil Levels as a Quantitative Measure of Periodontal Inflammatory Load in Patients with Special Needs. A thesis submitted in conformity with the requirements for the Degree of Master of Science, Graduate Department of Paediatric Dentistry, Faculty of Dentistry, University of Toronto, Canada.
- Devarajan P (2019) Acute kidney injury in children: clinical features, aetiology, evaluation and diagnosis.
- Mihalaş E, Matricala L, Chelmuş A, Gheţu N, Petcu A, et al. (2016) The Role of Chronic Exposure to Amoxicillin/Clavulanic Acid on the Developmental Enamel Defects in Mice. Toxicol Pathol 44(1): 61-70.
- Moradian Oldak, J (2012) Protein-mediated enamel mineralization. Front Biosci (Landmark Ed) 17: 1996-2023.
- Angelova ST, Targova Vl, Panov D, Bliznakova SP (2015) Assessment of Tooth Decay Risk in Children Suffering from Nephrotic Syndrome. - Scientific Cooperation’s Medical Workshops Titanic Business Europe. Proceedings Booklet. Istanbul, Turkey, pp. 52-57.
- Alm A, Wendt LK, Koch G (2004) Dental treatment of the primary dentition in 7-12-year-old Swedish children in relation to caries experience at 6 years of age. Swed Dent J 28(2): 61-66.
- Adulyanon S, Vourapukjaru J, Sheiham A (1996) Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol 24(6): 385-389.
- Angelova S (2018) Oral-Hygiene Condition in Children with Nephrotic Syndrome. The 6th Human and Social Sciences at the Common Conference. Humanities - Past, Nowadays and Future; pp. 59-62.
- Wogelius P, Poulsen S, Sorensen HT (2004) Use of asthma-drugs and risk of dental caries among 5 to 7-year-old Danish children: A cohort study. Community Dent Health 21(3): 207-211.
- Milano M, Lee JY, Donovan K, Chen JW (2006) A cross-sectional study of medication- related factors and caries experience in asthmatic children. Pediatr Dent 28(5): 415-419.
- Pingeleton WW, Bone RC, Kerby GR, Ruth WE (1977) Oropharyngeal candidiasis in patients treated with triamcinolone acetonide aerosol. J Allergy Clin Immunol 60(4): 254-258.
- Toogwood JH (1990) Complications of topical steroid therapy for asthma. Am Rev Respir Dis 141(2): 89-96.
- Linder N, Kuint J, German B, Lubin D, Loewenthal R (1995) Hypertrophy of the tongue associated with inhaled corticosteroid therapy in premature infants. J Pediatr 127(4): 651-653.
- Linder N, Kuint J, German B, Lubin D, Loewenthal R (1995) Hypertrophy of the tongue associated with inhaled corticosteroid therapy in premature infants. J Pediatr 127(4): 651-653.
- Bjerkeborn K, Dahllöf G, Hedlin G, Lindell M, Modéer T (1987) Effect of disease severity and pharmacotherapy of asthma on oral health in asthmatic children. Scand J Dent Res 95(2): 159-164.
- Ryberg M, Moller C, Ericson T (1991) Saliva composition and caries development in asthmatic patients treated with beta-2 adrenoceptor agonists: A 4-year follow-up study. Scand J Dent Res 99: 212-218.
- Angelova S (2018) Impact of Renal Diseases upon the Risk of Caries in Childhood. The 6th International Virtual Conference on Advanced Scientific Results.
- Kaufman E, Lamster IB (2000) Analysis of saliva for periodontal diagnosis: A review. J Clin Periodontol 27(7): 453-465.






























